Fall 2010
the magazine from FirstHealth of the Carolinas
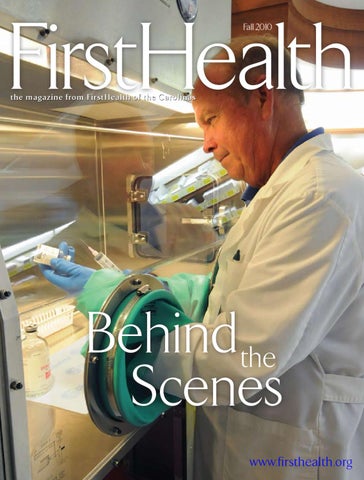
Behindthe Scenes www.firsthealth.org
Our Center for Rehabilitation is
Making the Grade
Staff members at FirstHealth Moore Regional Hospital’s Center for Inpatient Rehabilitation follow their patients closely as they improve.The facility is fully credentialed by UDSMR , which provides us with this facility report so we can ®
compare our performance with other inpatient rehabilitation centers. When it comes to caring for people, we’re at the top of the class.
Accredited by
O cto ber 1, 2008 - September 30, 2009
If you have questions about this information or would like to review the entire report, please call Inpatient Rehabilitation at (910) 715-1600, or e-mail us at rehab@firsthealth.org.
w w w.fir sthealth.o rg 537-105-10
firsthealth CEO message
Charles T. Frock
Chief Executive Officer FirstHealth of the Carolinas
An update on health care reform
A
s the Patient Protection and Affordable Care Act, better known as health care reform, remains in news headlines, consumers, employers and health care organizations have begun to feel the impact of the legislation. The main components of the reform bill are insurance reforms and insurance coverage changes. Insurance reforms affect insurance companies and address how they can operate in the future. Insurance coverage changes guarantee coverage for certain populations and eliminate many barriers to coverage. I think you will be interested in this overview of some of the changes that have already occurred or will take place in 2010. Free prevention benefits As of September 2010, all newly sold insurance plans and plans renewed through employers will be required to cover prevention and wellness benefits with no deductibles or cost-sharing. This requirement applies to both private and public insurance coverage, i.e. Medicare and Medicaid. Reduction of the Medicare “doughnut hole” Medicare beneficiaries (seniors and people with disabilities) who fall into the Medicare Part D prescription drug coverage gap, or “doughnut
hole,” will receive a discount on some medications as well as a rebate on prescription drug costs. Medicare participants who fall into the “doughnut hole” will receive a onetime rebate in 2010 only. In fact, more than one million seniors have already gotten a check from the federal government for $250. Starting in January 2011, “doughnut hole” beneficiaries will receive a 50 percent discount on brand-name drugs and other discounts on generic drugs that will increase every year until the “hole” is closed. Help for people with pre-existing conditions In the first year, the new law will create a new, temporary insurance program for people who have been uninsured for six months and who have a pre-existing condition. Premiums will be the same as those that individuals without a preexisting condition pay for the same coverage. This interim program will operate until exchanges are available. Also in the first year, the new law will bar insurers from denying coverage for children based on pre-existing conditions. Under existing law, insurers have the right to pick and choose their customers. With reform, they do not. Limits on insurance premium increases In the first year, insurance companies will be required to report and justify
their premium rates and any requests to increase premiums. This data must be reported to state insurance commissioners and federal authorities under new, uniform standards. Guarantees that premiums pay for health care services In the first year, insurance companies will be required to spend at least 80 percent (individual market) or 85 percent (employer market) of the premium dollars they collect on health care services and improvements in the quality of care. If they fail to do so, they must provide a premium rebate to consumers. In 2006, and without a mandate from the federal government, FirstCarolinaCare (FirstHealth’s wholly owned insurance subsidiary) returned premium dollars to its customers after it experienced stronger-than-expected financial results due to lower-thanexpected medical costs for its members. Continued insurance coverage for young adults In the first year, young adults who do not have an offer of coverage through an employer will be allowed to stay on their parents’ health insurance policy until their 26th birthday. FirstCarolinaCare has offered this benefit to its customers since 2006, four years before the passage of health care reform. New website If you would like more information on health care coverage options, go to the federal government’s newly launched health care website, www.HealthCare. gov. This site lists all available coverage options for individuals under age 65 as well as those for small businesses. Options include private plans, Medicaid, Children's Health Insurance Programs and high-risk pools, including existing state pools and new pools established under the health-reform law.
www.firsthealth.org
1
155 Memorial Drive P.O. Box 3000 Pinehurst, NC 28374 Editor, FirstHealth of the Carolinas . . . . . . . . . . . . . . . . . . Brenda Bouser Managing Editor. . . . . . . . . . . . . . . . . . . . . . . . . . . Jason Schneider Creative Director . . . . . . . . . . . . . . . . . . . . . . . . . . . Jan McLean Senior Art Director . . . . . . . . . . . . . . . . . . . . . . . . . . James Davis Production Director. . . . . . . . . . . . . . . . . . . . . . . . . . Traci Marsh
w w w. f i r s t healt h . o rg Contributing Writers
Brenda Bouser, Erica Stacy
Contributing Photographers
Eric Baker, Brenda Bouser, Don McKenzie, Mike Martin
Cover Photography Don McKenzie
Board of Directors FirstHealth of the Carolinas Mr. Alex Bowness, Chair Mr. Julian King, Vice Chair Robert Bahner Jr., M.D. Mr. H. Edward Barnes Jr. David Bruton, M.D. Mr. Jim Bulthuis Mr. David L. Burns David M. Cowherd, M.D. John N. Ellis, M.D. Walter S. Fasolak, D.O. Mr. Charles T. Frock
Mrs. Carolyn Helms Mrs. Anna G. Hollers Mr. John M. May C. Kenneth Mitchell Jr., M.D. Dr. Susan Purser Bruce S. Solomon, D.O. John S. Stevenson, M.D. William L. Stewart, M.D. David C. Thornton, M.D. Mr. Bob Tweed Mr. David Woronoff
Corporate Officers Chief Executive Officer, FirstHealth of the Carolinas
. . . .
Mr. Charles T. Frock
Chief Operating Officer, FirstHealth of the Carolinas President, Moore Regional Hospital. . . . . . . . . . . . . . . . . . . Mr. Stuart G. Voelpel Chief Financial Officer, FirstHealth of the Carolinas . . . . . Mrs. Lynn DeJaco Chief Medical Officer, FirstHealth of the Carolinas . . . . . . George D. Bussey, M.D. Chief Information Officer, FirstHealth of the Carolinas. . . . . . . . . . . . . . . . . . . . . . . . . . Mr. David Dillehunt Vice President, Human Resources, FirstHealth of the Carolinas. . . . . . . . . . . . . . . . . . . . . . . . . . Mr. Daniel F. Biediger
Departments 3 FHC Happenings 6
Calendar
24 Letters Features 7
Behind the scenes
Health care jobs that you may not know about
14 Exercise is medicine 16 Moving on up …
The Reid Heart Center
Vice President, Finance, FirstHealth of the Carolinas. . . . Mr. Jeffrey A. Casey Vice President, Community Services, FirstHealth of the Carolinas. . . . . . . . . . . . . . . . . . . . . . . . . . Mrs. Vivian Harrington Vice President, Quality . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Mrs. Cindy McNeill-McDonald Vice President, Patient Care Services/CNO, Moore Regional Hospital . . . . . . . . . . . . . . . . . . . . . . . . . . . . Mrs. Linda Wallace President, Montgomery Memorial Hospital. . . . . . . . . . . . Mrs. Kerry Hensley President, FirstHealth Richmond Memorial Hospital . . . Mr. John J. Jackson President, FirstCarolinaCare Insurance Company. . . . . . . Mr. Kenneth J. Lewis
28 The personal safety net of FirstHealth Response 30 Volunteering: How to and why
President, Foundation of FirstHealth . . . . . . . . . . . . . . . . . . Mrs. Kathleen Stockham The not-for-profit FirstHealth of the Carolinas is headquartered in Pinehurst, N.C., and is composed of Moore Regional Hospital, Montgomery Memorial Hospital, Richmond Memorial Hospital (a division of Moore Regional Hospital), the Foundation of FirstHealth, FirstCarolinaCare Insurance Company, and Regional Health Services. Comments on FirstHealth of the Carolinas magazine or changes of address should be directed to bbouser@firsthealth.org or to (910) 715-4278.
FirstHealth of the Carolinas is published three times a year by Vitality Communications 407 Norwalk St. Greensboro, NC 27407 (336) 547-8970 President. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . William G. Moore Senior Staff Accountant. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .Kelly Carter © Copyright 2010 by Vitality Communications, an operating company of StayWell/MediMedia USA, and FirstHealth of the Carolinas, Inc. No part of this publication may be reproduced or transmitted in any form or by any means without written permission from Vitality Communications. Articles in this publication are written by professional journalists who strive to present reliable, up-to-date health information. However, personal decisions regarding health, finance, exercise and other matters should be made only after consultation with the reader’s physician or professional adviser. All editorial rights reserved. Opinions expressed herein are not necessarily those of Vitality Communications or FirstHealth of the Carolinas. Models are used for illustrative purposes only.
On the cover Bob Beddingfield has been a pharmacist for 38 years, the last several as a pharmacist specializing in medical oncology at FirstHealth’s Outpatient Cancer Center. His job is one of the “Behind the Scenes” health care jobs at FirstHealth of the Carolinas that you might not know about. Read about them in a feature that begins on page 7 in this issue of FirstHealth of the Carolinas.
FHC happenings FirstHealth participates in national breast cancer study
C
ancer specialists at FirstHealth Moore Regional Hospital and some of their patients are participating in a nationwide clinical trial to find out if a new combination of drugs can help prevent the recurrence of breast cancer. Women who have breast tumors removed typically undergo radiation therapy or chemotherapy following surgery if, given the nature of the tumor, it appears likely that the cancer will come back. While a combination of chemotherapy drugs has increased the survival rate among women with high-risk breast cancer, many patients
still experience a recurrence. When the cancer recurs, it often spreads to other parts of the body and can be fatal. The current clinical trial tests whether a biologic agent—an antibody called Avastin—can help prevent or delay the recurrence of breast cancer in high-risk patients when given along with the standard chemotherapy drugs. In trials involving women with advanced metastatic breast cancer, Avastin doubled the time it took for their tumors to start growing again by preventing the growth of new blood vessels to tumors. A study of cancer care patterns by the Intercultural Cancer Council
FirstHealth gets grant to study hourly rounding
FirstHealth of the Carolinas has received a $25,380 grant from the Cardinal Health Foundation to fund a pilot program on the effectiveness of hourly nursing rounding. The program, called “The Effectiveness of Hourly Rounding on Patient Safety, Satisfaction and Nursing Workload,” will look at the evidence-based implementation of hourly rounding in the Orthopaedics and Urology Services unit at Moore Regional Hospital. Current research demonstrates that scripted hourly
determined that participation in clinical trials “increases access to state-of-the-art cancer care.” The study also found that people who live in small towns and rural areas are typically under-represented in cancer clinical trials. “The fact that a hospital our size in a rural setting can offer patients access to clinical trials and cutting-edge treatment options is unique,” says Chris Miller, director of clinical trials at Moore Regional. Moore Regional’s medical oncologists are Ellen M. Willard, M.D.; Todd A. Moore, M.D.; Robert A. Pohlmeyer, M.D.; Charles S. Kuzma, M.D.; and David G. Allen, M.D.
rounding can reduce or prevent errors in care, improve patient and nurse satisfaction, and decrease call-light usage. As a result, the FirstHealth study is designed to prove that the proactive approach of hourly rounding allows nurses to organize daily tasks and reduce the noise and interruptions in workflow, resulting in increased availability to meet patient needs efficiently and safely. Most of the FirstHealth grant will finance the hiring of two casual part-time certified nursing assistants (CNAs) who will conduct hourly rounding during peak medication administration times. The Cardinal Health Foundation received more than 250 letters of intent and invited only 100 organizations to submit full grant proposals for its E3 Grant Program. Only 40 organizations were selected to receive grants. www.firsthealth.org
3
MRH Foundation funds chest disease diagnostic equipment Thanks to a disbursement from the Moore Regional Hospital Foundation, state-of-theart technology that provides a safer and more accurate diagnosis of lung cancer and other diseases of the chest is now available at FirstHealth Moore Regional Hospital. Previously, endobronchial ultrasound (EBUS) and electromagnetic navigation bronchoscopy were available only at major academic medical centers in North Carolina. The Board of Trustees of the Moore Regional Hospital Foundation approved the $235,000 disbursement to provide the equipment for Moore Regional. “Our Foundation is committed to funding improvements to Moore Regional Hospital that enhance FirstHealth’s core purpose, to care for people,” says Howie Pierce, chair of the Foundation’s Grant Review Committee. “With this new technology, we will have the opportunity to care for people who previously had fewer options for diagnosis and treatment. I can’t think of a more appropriate use of Foundation resources.” According to Michael Pritchett, D.O., a board certified pulmonologist with FirstHealth’s Chest Center of the Carolinas and Pinehurst Medical Clinic, the new technology gives Moore Regional “a significant technological leg-up” in its ability to diagnose diseases of the chest. “We can use these tools together to improve the process of diagnosing, staging and treating lung cancer and other diseases,” he says.
4
Fall 2010
FHC happenings FirstHealth donations help Richmond County schools A FirstHealth of the Carolinas donation of strength and conditioning equipment will allow students at two alternative schools in Richmond County to get some exercise. The FirstHealth Center for Health and Fitness– Richmond donated seven pieces of cable-training equipment to Leak Street High School and several pieces of exercise equipment to the Richmond County Transitional School. “This equipment will allow us to offer a course in strength and conditioning as part of our curriculum offerings through our Health and Physical Education Department,” says Leak Street Principal Darryl Mason. According to John Caliri, director of the FirstHealth Centers for Health & Fitness, one-third of the children in North Carolina are overweight or obese, which underscores the importance of opportunities for physical activity in local schools. “We are pleased to donate this equipment to Richmond County Schools to support and encourage physical activity for area youth,” he says. Leak Street and the Richmond County Traditional School were created during the school district’s realignment efforts to offer students who have struggled in traditional classrooms the opportunity to graduate in a setting that offers more personal attention through smaller class sizes.
For more information on any of these stories, call (800) 213-3284
State hospital association recognizes FirstHealth CEO Charles T. Frock, CEO of FirstHealth of the Carolinas, received the 2010 Distinguished Service Award from the North Carolina Hospital Association (NCHA). The award goes to the chief executive officer of an NCHA member institution and recognizes a health care leader who has made valuable contributions to his/her institution, the health care field and to NCHA. Frock accepted the award in July during the annual NCHA meeting attended by representatives from more than 100 hospitals from across the state. “Chuck’s great leadership has moved the association into positions we couldn’t have imagined being in without him, positions from which the association can advance the quality of care provided in hospitals all across our state,” said NCHA President Bill Pully. FirstHealth of the Carolinas As chief executive officer of FirstHealth of the Carolinas since its creation in 1995, Frock is CEO Charles Frock accepts the NCHA's 2010 responsible—in coordination with policies adopted by the Board of Directors—for directing Distinguished Service Award. all activities related to the corporation’s development and operation and for ensuring that FirstHealth’s core purpose, to care for people, is fulfilled. He received a B.S. degree in industrial and systems engineering with a minor in business administration from the University of Florida in 1971 and a master’s degree in health administration from Duke University in 1974. He later completed certificate programs at Harvard University and Kings Fund College in London, England.
Former FHC Board chair to serve on NCHA Board John May, former chair of the FirstHealth of the Carolinas Board of Directors, has been named to a three-year term on the North Carolina Hospital Association (NCHA) Board of Trustees. May, who is an attorney with the local Robbins May & Rich law firm, has also served on the Board of Trustees for FirstHealth Moore Regional Hospital. A graduate of Wake Forest University and the Wake Forest School of Law, he received his master's in tax law from New York University. NCHA is a statewide trade association representing 130 hospitals and health systems. The association promotes improved delivery of quality health care in North Carolina through leadership, advocacy, information and education.
John May
www.firsthealth.org
5
For information on any of these events, call (800) 213-3284 or visit www.firsthealth.org/calendar.
October
Pottery Plus Auction Saturday, Oct. 2 5:30 to 8:30 p.m. Country Club of North Carolina Pinehurst Silent and live auctions to benefit the FirstHealth Hospice Foundation, supporting the work of FirstHealth Hospice & Palliative Care and the construction of the Hospice Chapel on the campus of the new FirstHealth Hospice House. Annual Wellness Screening Day Saturday, Oct. 9 8 a.m. to noon. FirstHealth Richmond Memorial Hospital Pre-draws will be conducted weekdays, Sept. 27-Oct. 8, 6 to 10 a.m. Wellness Profile, $25; PSA, $10; A1C, $10; EKGs, PFTs, Osteoporosis screenings, free; carotid artery, peripheral vascular disease (PVD) and abdominal aneurysm screenings, $30 each or all three for $85. Myself: Together Again—One Young Woman’s Story of Breast Cancer Recovery & Reconstruction Thursday, Oct. 21 5:30 to 7:30 p.m. Rooms A&B, Conference Center FirstHealth Moore Regional Hospital Diagnosed with breast cancer at age 32 and facing a mastectomy and reconstruction, Debbie Horwitz documented her journey so others would have a resource. She will share her story as told in her book, “Myself: Together Again,” in a program financed by the Moore Regional Hospital Auxiliary. Free. Registration is required as space is limited. Diabetes Health Fair Saturday, Oct. 23 10 a.m. to 2 p.m. FirstHealth Specialty Centers Building Pinehurst People living with diabetes and their families are invited to attend this information event featuring screenings, including blood sugar, 6
Fall 2010
blood pressure and foot; guest speakers on such topics as heart disease, neuropathy and nutrition; free meter trade-out (swap an old meter for a new one); door prizes; and cooking demonstrations. Tours of the FirstHealth Wound Care & Hyperbaric Center will be offered. Free.
November
Turkey Trot Saturday, Nov. 20 FirstHealth Center for Health & Fitness–Pinehurst This annual race includes a one-mile fun walk, 5K walk/run (3.1 miles), 10K walk/run (6.2 miles) and a half-marathon.
December
19th Annual Light Up a Life Tree-Lighting Ceremony Thursday, Dec. 2 5 p.m. FirstHealth Hospice & Palliative Care Aviemore and Memorial Drives, Pinehurst The Light Up a Life program provides an opportunity to share remembrances of family and friends as well as to honor those who are important in our lives. 23rd Annual Love Lights Ceremony Tuesday, Dec. 7 6:30 p.m. Main Entrance FirstHealth Montgomery Memorial Hospital Love Lights are $5 and can be made in memory or honor of a loved one. The event is sponsored by the Hospital Auxiliary. MRH Auxiliary Holiday Ball Friday, Dec. 10 The Carolina Hotel Ballroom, Pinehurst The 2010 Holiday Ball supports an initiative to assist Inpatient Rehabilitation patients at FirstHealth Moore Regional Hospital in completing their transition back home.
Behind the scenes… FirstHealth people with health care jobs you may not know about By Brenda Bouser
Bob Beddingfield, RPH Clinical Pharmacist, Outpatient Oncology
When you think about jobs in
health care, you probably think about doctors and nurses. If you’ve ever had occasion to use their services, you may also include physician assistants, nurse practitioners, various technologists and therapists among that number. But there are lots of other jobs associated with health care—many of them involved with quality assurance, patient safety or high technology. Most of them are behind the scenes and out of sight from the daily hustle and bustle of the health care world. Here are a few health care jobs at FirstHealth that you may not know about …
Bob Beddingfield has been a pharmacist for 38 years. For the past several years, he has been the pharmacist for FirstHealth’s Outpatient Cancer Center. He is the only pharmacist among FirstHealth’s community of 15-plus clinical pharmacists who works full time in a particular specialty. A registered pharmacist with a degree from the University of North Carolina at Chapel Hill, Beddingfield is actually part of a three-person team that attends to the medication needs of patients undergoing infusion chemotherapy at the FirstHealth Outpatient Cancer Center. His longtime colleague is Jane Monroe, a certified pharmacy technician, registered through the Board of Pharmacy and a FirstHealth employee for 32 years. Newer to the organization is Dianna Jones, PharmD, a graduate of the Pharmacy School at Campbell University, who works part time. “Jane is the primary person at mixing and has an amazing ability to remember all of the patients, orders, diagnoses and protocols,” Beddingfield says. “Dianna and I frequently dose the chemos based on the renal (kidney) and hepatic (liver) labs. We provide drug information and research articles frequently for the nurses, patients and physicians.” All three collaborate with the rest of the clinical team to improve the safety and effectiveness of medication use at FirstHealth. With five on-site hematologists/medical oncologists and a patient load of 40 to 50 every day, Beddingfield, Monroe and Jones stay busy. Protocols are lengthy, and medications and therapies are constantly changing. Drug information and reimbursement issues require continuous research. Some medications are now well into their fourth generation, others are new, and still others are associated with clinical trials. Beddingfield is especially encouraged by the level of research into cancer treatment. “We look forward to improvements that will help with increasing survival rates and maybe even cures for cancer,” he says. www.firsthealth.org
7
David Quinlan Picture Archive Administrator
Lynn Agee, R.N. (left) with new mom Adrienne Noll and newborn Hadley London Noll
Lynn Agee, R.N. Newborn Visitation Nurse There’s nothing quite as precious as a newborn. There’s also nothing quite so intimidating, especially if you’re a first-time mom with questions about infant feeding and weight-gain or a host of other concerns. As the registered nurse for the Moore Great Beginnings Newborn Visitation Program, Lynn Agee, R.N., calls on Moore County families who have just welcomed a baby into their home. The service is funded by a grant from Partners for Children and Families, Moore County Smart Start, and provided through FirstHealth Home Care Services. “Babies don’t come with instructions,” Agee says. “Although the birth of a baby is a joyous occasion, it can be overwhelming.” The Newborn Visitation service is designed to help ensure that every Moore County newborn gets off to a healthy start. While not every family accepts Agee’s offer of a visit, those who do usually have plenty of questions for this veteran nurse with a background in pediatric and neonatal intensive care nursing and lactation counseling. During an in-home visit, Agee will weigh the baby, provide guidance and assistance with breast- and bottle-feeding, talk about health risks associated with second-hand smoke, discuss the proper way of putting a baby down to sleep (not on the tummy, please), and review safety measures or recall issues involving car seats and other infant equipment. If she observes a need or a problem, she’ll discuss community resources or suggest a physician follow-up. “It’s not intended to take the place of the pediatrician’s visit,” Agee says of her service. “I try to catch families within the first couple of weeks of their baby’s birth so if they’re having issues, I can offer support early on.” Although most of the moms Agee visits are brand new to the motherhood gig, many are not. It’s not all that unusual for a mom with several children to accept her offer for an in-home visit. Every baby is different, she points out, whether it’s the first or the fifth for the family. “A lot of moms want reassurance that baby is doing well and gaining weight,” Agee says. “It helps to have someone follow up.”
8
Fall 2010
David Quinlan has an office in the Patient Care Administration area of FirstHealth Moore Regional Hospital, but he is only occasionally there. As administrator for FirstHealth’s Picture Archive and Communications System (PACS), Quinlan moves effortlessly throughout the warren-like world of medical imaging to work with radiologists, technologists and Information Systems personnel. His job is to ensure that the organization’s digital radiology archive performs as it is intended and to investigate ways of making it better. In what Quinlan describes as the “digital world” of modern radiology, his daily responsibilities cover a wide range of tasks—from helping a radiologist with a study issue to working with the Information Systems staff on a troubleshooting matter or training a technologist on a new function. “My job is to make sure the system is running smoothly,” says Quinlan. “My job is to make sure the images are making it across the system.” PACS is a state-of-the-art system for the digital access, viewing and storage of all kinds of radiologic images— conventional X-rays and MRIs, mammograms and CTs, bone density tests and ultrasounds—“pretty much anything we’re doing in the X-ray imaging department,” Quinlan says. Because the system is entirely electronic, patient images and the accompanying patient reports can be accessed simultaneously at multiple locations throughout
David LaRouche Microwave Operator For the past 15 years, David LaRouche has quietly gone about the business of performing an important task for FirstHealth of the Carolinas that most people probably don’t even know about. As the organization’s microwave operator, LaRouche is responsible for the controlled disinfection and discard of regulated medical waste—much of it blood-soiled. Working from a nondescript metal building in a gated area on the campus of FirstHealth Moore Regional Hospital, he uses state-of-the-art technology that combines cutters, steam and microwaves to shred, moisten and heat about 1,500 pounds of contaminated hospital waste each day. “It comes to me in red cans, and I take it from there,” LaRouche says. “The guys who haul it to me call it ‘redbag’ waste.”
the FirstHealth system as well as in the numerous participating FirstHealth and independent clinics. “When a patient’s radiology study is done, the images are in the system instantaneously,” Quinlan says. “As soon as they are in PACS, any authorized person can see them. You’ve taken a tremendous lag time out of the process, because it’s instantaneous now.” Trained as a general radiology technologist, Quinlan first came in contact with a PACS system in 1999 while working at Boston’s Beth Israel Deaconess Hospital. After being trained on the job, he moved to Duke Medical Center, where he served as PACS administrator until joining FirstHealth in February 2006. The organization was just weeks away from going live with its own PACS system. “I was here prior to the implementation of the PACS Administrator David Quinlan (standing) system and helped set it up,” Quinlan says. with radiologist Michael Edwards, M.D. Since the implementation of FirstHealth’s PACS system, physicians who once depended on stacks of manually transported filmed images and written reports now need only secure computer access, access that can be not only immediate but also simultaneous. An orthopaedist at Pinehurst Surgical can look at the X-ray of a broken bone at the same time as an Emergency Department physician at Montgomery Memorial Hospital, for example. A family practitioner at the FirstHealth clinic in Raeford can access a CT scan at the same time as a radiologist at Moore Regional. Huge storage areas once devoted to thousands of pieces of film are steadily shrinking as new images are captured electronically with backup at each of the three FirstHealth hospitals. As storage space has shrunk, so have film budgets, resulting in an annual cost-savings of thousands of dollars to the organization. Most importantly, however, is the effect on workflow and ultimately to patient care in terms of time and efficiency. “I think everyone has found this to be a great system,” Quinlan says.
LaRouche was working as the maintenance engineer for a local hotel when he heard that FirstHealth planned to buy a microwave. He applied for the job, got it and was trained in the equipment’s operation by the manufacturer, ABB Sanitec. The technology had originated with a German firm in the 1980s. According to LaRouche, a programmable logic controller with simplified fault management controls the microwave operation, which begins as the waste is lifted and dumped into a hopper and onto rotating shredder-cutters. As the shredded waste travels through an enclosed screw conveyor system, it is moistened with super-heated steam and then heated with microwaves that use four 1.2-kilowatt microwave generator power supplies. By the end of the process, which takes about 90 minutes, the waste is essentially unrecognizable, reduced in volume by about 80 percent and ready for disposal in a designated landfill. LaRouche, who works from 6 a.m. to 3 p.m. Monday through Friday, responds when the machine “tells me when it’s hungry” and monitors the entire process. While on-site disinfection of contaminated matter means a considerable cost-savings for FirstHealth of the Carolinas, the disinfection process involves an even more important concern, according to LaRouche. “Safety is of the utmost importance,” he says.
www.firsthealth.org
9
Brenda Cranford, MLT, H.T. Laboratory Histotechnologist Blessed with a steady hand and a head for multi-tasking, Brenda Cranford has made a life’s work in the medical lab at FirstHealth Moore Regional Hospital. Schooled as a laboratory technician more than 30 years ago, she was handpicked by one of the hospital’s pioneer pathologists, the late Robert Studer, M.D., to move into the specialized area of histology. “We process tissue,” Cranford says. “Anything that comes out of the operating room comes through our department. We help the pathologists to diagnose disease by preparing slides and tissues for them to read.” As a registered histotechnolgist, as well as a registered lab technician, Cranford prepares human tissue samples for microscopic examination by a pathologist. She freezes and cuts sections of tissue and then mounts samples on slides and stains them to emphasize details, or she embeds them in wax before cutting them into very small slices. Some samples might be no bigger than the head of a pin; others might resemble a thread off a ribbon. Each will ultimately go to a pathologist who will review the sample and make a diagnosis. With quality and safety increasingly ingrained in the process, automation now figures prominently into the operation of the contemporary hospital lab. Not so when Cranford joined the Moore Regional lab, with an associate in applied science degree from Sandhills Community College, 32 years ago. “We have a lot of luxuries now that we didn’t have then,” she says. “Everything was manual; now it’s automated. It’s incredible how far we’ve come since those days.” As patients have become more proactive in being screened for various diseases and because laboratory tests have become increasingly important in the diagnosis and treatment of those diseases, histotechs and the cytotechnologists who prepare fluid samples are vital members of the medical laboratory team. Each of their processes has a different protocol. Each step is checked and double-checked to ensure accuracy. “There’s a lot of room for error,” says Cranford. “It takes a lot of concentration, a lot of focus. We double-check everything, and there are a lot of checklists to make sure everything gets done. You’re dealing with something that’s very important to the patient.”
Leigh Perry & Julie Jenkins, CMDs Certified Medical Dosimetrists
Leigh Perry, CMD (seated), and Julie Jenkins, CMD
10
Fall 2010
More than 4,000 people work for FirstHealth of the Carolinas. Of that number, only two—Leigh Perry and Julie Jenkins—are certified medical dosimetrists. The work keeps them tucked away in a quiet, out-of-the-way office in the Radiation Oncology department at FirstHealth Moore Regional Hospital. Few people know they are there, but their work is an essential part of a radiation therapy team that also includes physicians who specialize in radiation oncology, medical physicists, radiation therapists and nurses. Briefly, their job involves developing a treatment plan for patients who are undergoing radiation therapy for cancer. The task involves calculating the radiation dose that targets and destroys the cancerous tumor while sparing surrounding healthy tissue.
The robotic surgery team As a urologist finishes up one prostate surgery, a registered nurse and four surgical technicians are already preparing FirstHealth’s da Vinci Robotic Surgical System for the next case. As the surgical team wakes and moves the drowsy patient, the specially trained da Vinci crew is removing and replacing surgical drapes and detaching and replacing surgical arms. The clean-up and next-case preparation takes about 45 minutes—all in the gowned, gloved and masked sterile environment of the operating room. From left: Dione Collins, surgical tech; Sharron Purvis, R.N.; Judy Hunsucker, surgical tech; Amy Comer, surgical tech; and Jamie Waldschmidt, surgical tech. Registered nurse Sharron Purvis and surgical tech Judy Hunsucker, longtime members of the urology A second, and totally different, team is trained to assist with the surgical team, have been at the da Vinci job the longest. gynecology cases that are also done by da Vinci. Registered nurse They were trained to clean, care for and calibrate the state-of-the-art Crystal Locklear works with surgical techs Stefanie Dean and Karen surgical robot at the time it was acquired in 2006. Rhone on that team. “We, as a team, the R.N. and the certified surgical techs, always Although the robot stands idle as its care team rushes about clean the robot and make sure it is working for the next case,” Purvis preparing for the next case, it is central to the success of these says. “I cannot tell you how valuable each member of the robot team procedures and is, according to Hunsucker, almost like a member of is for the procedure and for an excellent outcome for the patient. this OR family—inanimate but ready to go when the time comes. Safety is very important to each and every one on the robot team, so “Once you start a surgery, you’re relying on it to do its share of the the robot is very much taken care of and very much loved.” work,” Hunsucker says. Helping Purvis and Hunsucker with the set-up are surgical techs Dione Collins and Amy Comer. Surgical tech Jamie Waldschmidt fills in for Whitney Brinkley, who is on maternity leave.
“The radiation oncologists will outline the tumor and prescribe the dose they want to deliver,” Jenkins says. “Using a 3D treatment planning system, we will customize a treatment plan for each patient.” Many dosimetrists start out as radiation therapists, as Perry and Jenkins did, and then get their dosimetry training—often under the supervision of medical physicists or other dosimetrists. FirstHealth’s two medical physicists, Michelle Tortora and Michael Gnaster, are responsible for high dose rate treatment planning. They also develop and direct quality control programs for equipment and procedures. Dosimetry is a delicate science. Dosimetrists must have a wide range of mathematical skills, including algebra, trigonometry and introductory calculus, as well as be extremely comfortable with computers. They must also be able to visualize objects in threedimensional concepts. Perry and Jenkins are called upon daily to use their knowledge of
physics, math, anatomy, physiology and radiobiology to develop a critical arrangement of radiation beams that deliver an individualized dose of radiation to the cancer site according to the physician’s prescription. A dosimetrist for 17 years and a FirstHealth employee for five years, Perry says, “I absolutely love what I do. It’s always challenging, which is why I chose dosimetry to begin with. Nothing is ever the same. It’s such a changing field, and we are learning on a continual basis as the technology changes so much.” Jenkins has been a dosimetrist since 1997 and a FirstHealth employee for five years. “I enjoy working closely with the physicians to come up with the best treatment plan for our patients,” she says. “We play a key role in how patients are going to be treated, and that is very satisfying for me. At the end of the day, it’s all about quality patient care.”
www.firsthealth.org
11
Albert Thomas Floor Specialist, Environmental Services Every once in a while, in a letter to the CEO or in a comment to a member of the staff, a visitor to a FirstHealth hospital will remark on the shining spotlessness of the floors. Albert Thomas is always happy to hear those compliments. He is part of an Environmental Services team whose job it is to keep the floors so clean. “I do the floors,” he says. “I do the carpets.” Thomas has been cleaning floors for FirstHealth of the Carolinas for the better part of the last 16 years. Until a year ago, his was a part-time job, performed in conjunction with his full-time work with the North Carolina Department of Corrections. He retired in May 2009 after eight years as assistant warden of Scotland Correctional and 29 years with the DOC. With FirstHealth Environmental Services, Thomas is part of an 11-man/ one-woman team that maintains the floors throughout Moore Regional Hospital. He works second shift on a crew that is also responsible for eight FirstHealth buildings outside Moore Regional. The first-shift crew cleans the floors in patient rooms.
Every hallway is swept, scrubbed and buffed daily. “Some ride, some scrub, some strip and wax,” Thomas says about the work he and his co-workers do. “We’re all over.” All of that riding, scrubbing, stripping and waxing occurs with the operation of some fairly sophisticated equipment: five Clark Boost auto-scrubbers, plus a riding Avenger scrubber; four carpet cleaners; four indoor pressure washers; and eight buffers (some walk-behind, some riding and some hand), according to Floor Crew manager William Ross. Everyone is cross-trained on each piece of equipment. As a semi-lead person for his crew, Thomas is “very particular” about his work, especially about cleanliness and safety. “They tell me I’m a safety fanatic,” he says. The job is not without its frustrations, though. One is seeing a scratch on a just-waxed floor; the other involves the sometimes-bossy Tug robots that can pop on a floor at any time while making Pharmacy and Materials Management deliveries throughout the hospital. Both quirks are just part of the job, though. The work is hard, but every task has a plan, which makes it easier, according to Thomas. “I enjoy it,” he says. “If I didn’t, I wouldn’t be here. I enjoy the people, too. I’m the kind of person who likes to have a plan together. It’s hard work, but it’s not as hard when you have a system.”
Tony Duguay Plant Engineer, Central Laundry Name it and Robert “Tony” Duguay can fix it. It’s an important job for FirstHealth’s Central Laundry, which turns out anywhere from 12,000 to 26,000 pounds of soiled-to-clean linens each weekday. As plant engineer, Duguay is resident plumber, electrician, handyman and jack-of-all-trades, ensuring that mammoth conveyor belts convey, washers wash, dryers dry, ironers iron and folders fold. “My job is to keep the plant running,” he says. “We try not to outsource anything. The more things I know how to fix, the less we have to outsource.” When the Central Laundry opened on Oct. 1, 1999, it represented an immediate boost to FirstHealth’s bottom line. At the time, an outside contract cost the organization around 58 cents a pound for clean linens. On average, the in-house operation currently processes about 17,300 pounds of laundry a day or 4.5 million pounds a year, which translates into upwards of $400,000 in annual cost-savings to FirstHealth. According to his supervisor, Central Laundry Director Earl Carter, Duguay does his share to assure that this cost-savings continues. “Tony is an all-around great guy,” says Carter, “dedicated and very
12
Fall 2010
Marty Davis Biomedical Technician
knowledgeable, always willing to assist when/where he can. He is an asset to FirstHealth of the Carolinas and the Laundry.” Despite the fundamental nature of the job, washing, drying and folding linens and scrubs, the Central Laundry is a high-tech, computerized business. It is Duguay’s job to see that the operation runs smoothly. His day starts early—at 7 a.m. when he starts up the machines—and ends around 3:30 p.m. after all of the equipment has been checked, cleaned and readied for the next day’s production. There is no job too large or too small for him to tackle. That includes preventive maintenance as well as repairs. “We can’t stand to be down for long,” he says. “It’s a fulfilling job to keep these things up and running in A No. 1 shape.” Duguay’s priorities are quality, timeliness and safety. “Our main thing is quality, and everybody gets what they’re supposed to get on time,” Duguay says. “We work on whatever breaks down, and we do not cut corners on any kind of safety.”
As the only biomedical technician at FirstHealth Richmond Memorial Hospital, Marty Davis is responsible for ensuring that every piece of patient care equipment at the hospital is, first of all, functional and, most importantly, safe. “Anything that’s attached to the patient, I take care of it,” he says. The work that Davis and his colleagues perform in the biomedical/clinical engineering field covers an impressive array of fields and devices. Infusion pumps, anesthesia machines, monitors, dialysis machines, diagnostic and lifesaving equipment—Davis has touched it all, installing, inspecting, maintaining, repairing and calibrating machines throughout the hospital. “Marty takes care of all of our equipment and is the biomed point person for several pieces of specialized equipment,” says Richmond Memorial’s Chief Operating Officer Allison Duckworth. “He is a great biomed technician who really goes above and beyond on a regular basis.” Although he is the only technician directly assigned to Richmond Memorial, Davis is part of an eight-person FirstHealth of the Carolinas biomedical engineering team— seven men and one woman—who cover the three FirstHealth hospitals. Two other technicians are solely responsible for the radiology equipment located throughout the organization. Like all of FirstHealth’s biomed techs, Davis regularly takes a week of call for all three locations. All of the technicians are cross-trained, although each has a specialty. Davis’s is dialysis equipment. Davis reports to Brian Lefler, director of Biomedical Engineering, who attributes his success in his position to two important qualities. “Marty is successful due to his technical abilities, certainly, but the main reason he's successful is his customer service skills,” Lefler says. “That cannot be overstated.” In addition to his equipment responsibilities, Davis serves on Richmond Memorial’s Safety Committee and is the point person for new equipment purchases. To ensure quality and patient safety, he has a lengthy schedule for major/minor prevention maintenance that assures every piece of equipment will be thoroughly checked out at least once a year—some several times. A born tinkerer who even as a boy wanted to know how things work, Davis has a bachelor’s degree from Wingate University, but returned to Stanly Community College for training in the biomedical engineering field. Additional training occurs with each new equipment purchase or with quality and/or safety updates from The Joint Commission and the Food and Drug Administration. “Technology changes so quickly now,” Davis says. “It changes every day, and we have to stay with it. That way, you’re going to do the best job you can.”
www.firsthealth.org
13
By Brenda Bouser
J
erry Stremick had packed on a few extra pounds and felt like he needed to shed some weight. “The object was to lose about 20 pounds or so,” the 68-year-old Stremick says. “It was fine when I was 200 pounds and playing football in college.” Stremick took his concerns about his weight to his primary care physician who gave him a medical referral to the new Exercise is Medicine program at the FirstHealth Center for Health & Fitness–Pinehurst. “It’s been good,” Stremick says about the program. “It’s been working well, and I’m pleased with it. ” Launched by the American College of Sports Medicine and the American Medical Association, Exercise is Medicine (EIM) encourages health care providers to make exercise a part of their regular patient treatment plans. Ideally, according to Darrell Simpkins, M.D., participating physicians will begin to regard physical activity as a vital sign—just as they would weight and blood pressure—and encourage their patients to use exercise to become more involved in improving their own health. “This is a tremendous program to link exercise, patients and their doctors,” says Dr. Simpkins, an emergency department physician and medical director for the FirstHealth Centers for Health & Fitness. “Almost everybody is interested in results and statistics, and lots of patients like to please their doctor. This is a way the doctor can say, ‘I’d like you to go to the fitness center,‘ and there's a program in place to help them.“ 14
Fall 2010
After discussing physical activity needs with their patients, participating doctors refer them to the Center for Health & Fitness– Pinehurst for another part of the EIM program, a professional—and free—exercise assessment and treatment plan developed by a trained exercise technologist. “Our program builds on the EIM initiative by giving participating physicians a referral pathway and the tools to make appropriate referrals to FirstHealth’s qualified exercise professionals,” says John Caliri, director of the FirstHealth Centers for Health & Fitness. “The referral gives the patient access to a no-cost physical fitness assessment, goal-setting and an actual activity program that’s suited to their specific needs. Participation in the program also includes communication back to the physician so he, or she, can assist patients in effectively using exercise as a prevention or treatment method for attaining or maintaining health.” n
If you think you might be interested in a referral to FirstHealth’s Exercise is Medicine program, talk to your primary care provider. For more information on the program, call (800) 213-3284.
Exercise is Medicine step by step • Step 1: At every office visit, the physician measures the patient’s physical activity as a vital sign. • Step 2: If appropriate, the physician refers the patient to the Center for Health & Fitness–Pinehurst for a health assessment, consultation and program development. There is no charge to the patient for this service. • Step 3: A Health & Fitness exercise technologist meets with the referred patient for the health assessment and to create a personalized exercise program that the patient can perform in the environment of his/her choice (i.e., park, gym, home). The patient receives a two-week membership to the Center for Health & Fitness* of his/her choice and, as appropriate, is referred to other health services. (Patients are under no obligation to join the Center for Health & Fitness.*) • Step 4: The Health & Fitness staff communicates with the referring physician about the participant’s screening results, participation and progress. Anyone, age 16 and up, who needs to start an exercise program to improve his/her health can participate in the EIM program as long as there has been a physician’s referral—even those dealing with a chronic illness such as hypertension or diabetes or even cancer or heart disease.
A physician’s perspective Phillip Mondi, M.D., who specializes in internal medicine at Pinehurst Medical Clinic, started referring patients to the Exercise is Medicine program through a pre-launch pilot. A long-time proponent of physical activity, both personally and for his patients, Dr. Mondi describes EIM as an “excellent program” that could be “beneficial to almost everyone,” especially the chronically ill, patients with strength and flexibility issues, and those at risk of falling. He has been especially impressed with the treatment plans, which are tailored to each participant’s specific abilities and needs. “My patients have been very responsive and think this is going to be a great program,” he says. “Once they see what their options are, I think a fair number will ask to be referred to the program. The sky’s the limit.”
Foundation involvement
A
disbursement from the Moore Regional Hospital Foundation funded the purchase of the Technogym Wellness System software and exercise equipment that will complement FirstHealth’s Exercise is Medicine program at the FirstHealth Center for Health & Fitness–Pinehurst. “The equipment is really state of the art,” says Ron Schuch, a Foundation Board member. “There are only a few facilities in the country that use this kind of technology.” While the EIM program encourages a patient and his personal physician to partner in an exercise plan geared toward improving the patient’s health, the Technogym system provides the technology for ensuring that the patient safely follows his personal “exercise prescription.” It also stores the information so the program participant and the Health & Fitness staff can follow the participant’s progress and share the information with the participant’s physician. Founded in Italy and now headquartered in Seattle, Technogym was the Official Supplier for the 2000 Sydney, 2004 Athens, 2006 Torino and 2008 Beijing Olympic Games and for the World Cup 2010. It will be the official fitness equipment supplier for the London 2012 Olympic Games.
www.firsthealth.org
15
T
h e
R
e i d
Facility stats n 186,000
square feet
n Five
floors
n Two
inpatient floors
n One
floor for outpatient clinics
n Main
floor with Operating Room/Cath
Lab/Electrophysiology n One
floor with Nuclear Medicine,
the potential for sterile processing expansion, utilities and shell space
“A project of this scope is a once-in-a-lifetime opportunity,” says Project Manager Jay Snyder, FirstHealth’s director of Planning, Design and Construction. “I can’t tell you how great the project is."
16
Fall 2010
H
e a rt
C
e n t e r
The construction phase of the Reid Heart Center, the FirstHealth Cardiac and Vascular Institute, is nearing completion on the campus of FirstHealth Moore Regional Hospital. The state-of-the-art facility, which combines all elements of Moore Regional’s cardiovascular care into one area, is scheduled to open in early 2011. The construction project has been an unusual one in many ways, and you may be interested in learning about it.
www.firsthealth.org
17
Reid Heart Center
Construction stats Construction on the main building began in April 2009, with excavation in June 2009. Completion is anticipated for December 2010 with stocking and unit moves to follow in a phased occupancy that should be completed in January 2011. n 30,000
cubic yards or 3,000 truck loads of mass excavation
n 10,000
cubic yards or 1,000 truck loads of excavation refill
n 750
tons of steel
n 5,400
cubic yards of concrete
“Every space has a purpose,” says Project Manager Jay Snyder.
Project manager Jay Snyder, the director of Planning Design and Construction for FirstHealth of the Carolinas, serves as project manager for the Reid Heart Center construction project. A native of northern New York, near Montreal, Quebec, Canada, he received a B.S. in Construction Management Engineering from Syracuse University. While serving in the United States Air Force in both Logistics and Civil Engineering, Snyder managed several construction efforts in the Middle East, South America and California. He continues to serve as a captain in the Air Force Reserve. Before joining FirstHealth of the Carolinas, he was employed by R.J. Griffin & Company, the contractor that was involved in the demolition of the buildings that came down to prepare the Heart Center footprint. Married with a 3-year-old son, he enjoys spending his spare time with his family and as a private pilot.
Operating room workflow In an unusual attempt to anticipate workflow, each type of operating room and patient room in the Reid Heart Center was built as a full-sized mock-up and rooms were prepped to look as they would at completion. Cabinets were represented. Cover plates doubled for outlets and switches. Boxes represented medical equipment. Tubes and piping were assembled and suspended from the ceiling to represent medical booms. During the simulation process, members of the Heart Center’s Surgical Services staff walked through the space, providing feedback and making revisions to the layout in order to optimize flow and match current practices.
18
Fall 2010
Reid Heart Center
Reid Heart Center Project Manager Jay Snyder (at right) takes Cynthia Ward, director of Specialty Centers/CVT Clinic (left), and Health Information Management Director Cassina Hunt on a hard-hat tour of the soon-to-be completed Reid Heart Center.
Multi-Use ORs The availability of two multi-use operating rooms will allow FirstHealth medical teams to perform two or more procedures during one operating room visit without the need for moving the patient to a different OR suite. Adapting the X-ray capabilities of a cardiac catheterization lab into an operating room creates better imaging capabilities for complicated procedures that may require a conventional open-surgical approach. The multi-use rooms will be used by the Vascular Service for placing grafts in patients—those being treated for aortic aneurysm, for example, and for cardiovascular procedures that might incorporate imaging or cardiac catheterization. All levels of anesthesia, up to and including general anesthesia, will be available in these new rooms. www.firsthealth.org
19
Reid Heart Center
Custom air handling systems The three air handlers in the Reid Heart Center provide custom conditions for particular areas of the building. Purchased through Trane and built by Ingenia in Montreal, Canada, the units were delivered on 21 tractor-trailers and assembled in the field. They provide 75 percent redundancy and incorporate an internal trolley system to expedite fan motor swap-outs to reduce downtime. The custom air-handling systems have stainless steel interiors to minimize corrosion and infection control concerns. They also include silencers to reduce the amount of noise generated by airflow through the equipment and duct work.
Local hiring & purchasing About 30 percent of the labor force for the Reid Heart Center construction project was employed locally, and subcontractors recruited local skilled labor to reduce costs. Most of the structural materials were obtained from within 75 miles of the Moore Regional Hospital campus. These materials include steel, site utility piping, concrete, plumbing, electrical, medical gas piping and drywall.
Energy plant upgrade The Reid Heart Center project includes a $10 million upgrade to the energy plant that boasts a major increase to chilled water capacity (used to cool the facility). The project also includes the installation of two 2500-killowat generators for a total of 7500 kilowatts of generator capacity— enough to provide 100 percent backup power to the Heart Center regardless of the color plug. The same capability will eventually be provided to the main hospital.
20
Fall 2010
Reid Heart Center
An elevator of record size The Reid Heart Center has seven elevators: four public elevators, one service elevator, one patient elevator and one trauma elevator. According to Otis Elevator Co., the 10-by-15-foot trauma elevator (with its 15,000-pound capacity) is the largest elevator the company has installed in the state of North Carolina. The elevator serves as a pathway for large clinical equipment that is installed in the basement.
www.firsthealth.org
21
Reid Heart Center
“Greening” the project Project Manager Jay Snyder revised the drywall from standard paper drywall to mold resistant drywall in an effort to reduce infection control risks due to mold and mildew. This has become the standard of practice for new construction in the clinical environment. The building maximizes the use of natural light by incorporating full-height window assemblies and creating open expanses to allow for the passage of light to the interior spaces of the building. The air handler units that condition and circulate the air in the facility use variable speed drives that provide maximum energy efficiency. The system also reclaims condensate water from the system and recycles it into the chilled water system to reduce water consumption.
A stone wall forms the main focus of the lobby level and provides a grounding point. The lobby’s interior wall is built with sold cherry wood panels. All of the cabinetry throughout uses multi-tone wood grain laminate with neutral solid surface counter areas for a warmer feeling. Patient floors use simulated wood grain sheet vinyl flooring. Paint colors fall within typical spa tones including use of soft yellows, warm blue and light green. Light fixtures in most areas provide indirect lighting, which produces fewer glares, reduces eye fatigue and simulates daylight.
Matching the old with the new The Reid Heart Center project began with the separation and demolition of hospital buildings constructed in 1935, 1949 and 1970 from the original 1928 building. The project included placing a new end wall on the 1928 building.
Waiting room areas include more private restrooms and vending space. The main lobby, which acts as an extension of all waiting areas, incorporates numerous private seating arrangements within a public space.
The same brick is also used on the Reid Heart Center’s façade. Fall 2010
Reid Heart Center interiors focus on use of natural elements.
A building highlight is a bistro, staffed by Moore Regional Hospital Food & Nutrition, which will serve prepared sandwiches and hot and cold beverages.
An exhaustive effort found brick at the local Triangle Brick brickyard that allowed the construction team to match the 80-year-old brick in the original 1928 building with brick produced in 2009.
22
Aesthetic/ visitor-friendly qualities
Reid Heart Center
Covered walkways and connections An enclosed walkway at ground level that connects Moore Regional’s original 1928 building to the Reid Heart Center will be open for public and staff use. An enclosed bridge on the third floor connects the Critical Care floor to the current Critical Care areas of the hospital’s third floor
The name The Reid Heart Center is named in honor of Pinehurst residents Walter and Betty Reid whose multi-million-dollar contribution to the project-supporting Stepping Stones Campaign constituted the largest single gift to FirstHealth Moore Regional Hospital in its 80-plus-year history. This is the first time that a FirstHealth building has been named for individuals.
The enclosed third-floor bridge that connects the Critical Care floor in the Reid Heart Center for the current Critical Care areas of the hospital.
Outside interest in the Reid Heart Center The North Carolina Department of Health Service Regulations displayed the Reid Heart Center’s life safety plan as an example of best practice at the annual meeting of the North Carolina Healthcare Engineer Association in March 2010. Southeastern Building Construction magazine published a three-page story on the Heart Center as part of its monthly issue recognizing complex health care construction initiatives. The local newspaper, The Pilot in Southern Pines, has featured the Reid Heart Center in numerous stories. www.firsthealth.org
23
Extraordinary attention to service
I
am the daughter of a patient who was recently treated at FirstHealth Moore Regional Hospital. My mother lives in Pinehurst and over the last 18 months has had many admissions to your hospital due to declining health with many complications. As Mom’s pulmonologist said, “Your mother has a constellation of disease processes.” It is heartbreaking to watch her decline. I write to you today to express my Note: After Ms. Ramey’s mother sincere gratitude for the outstanding passed away on June 5, 2010, care and service mother receives Ms. Ramey added the following every time she has a hospital stay message to her previous note: at FirstHealth. Mother would write to “The Hospice care my mother you herself and echo my compliments (as we) received was a blessing to you and your team if she were and another tribute to the great capable. She is a retired R.N. and services FirstHealth provides. Mom knows good care from both sides. passed with dignity and grace. The My experience, as the daughter of Hospice nurse, Donna Neal, was a a patient observing your staff, has comfort to the entire family.” been extremely positive beginning with the auxiliary staff at the entrance to the food service worker who told my mother that if she needed anything or was not satisfied, she could call him and he would help. The nursing staff and health care team are competent, committed and caring. I was referred by Pinehurst Medical, where mother gets her outpatient care, to Sharon Saunders, the case manager assigned to Mom for discharge planning at FirstHealth. She has been a blessing to us as we navigated Mom to a skilled nursing facility where she may stay indefinitely. Sharon has offered to address any question or request by the family and has worked to meet our needs with a kind heart. As a family with health care backgrounds, our expectations for quality care are quite high. My father is a retired family practice physician. We have been pleased with the quality of care and the extraordinary attention to service that every member of the FirstHealth team has delivered. Thank you for giving Mother great care and medical attention. Thank you for your commitment to excellence. Bess Ramey Senior Account Manager Pfizer CGC McLeansville
24
Fall 2010
Grace, good humor and caring
T
uesday, Jan. 26, 2010, was a busy day in the Outpatient Department at FirstHealth Moore Regional Hospital. I know, because I was there for most of the day. I was scheduled for a liver biopsy, a procedure I’d been dreading for the previous two weeks. We always fear the unknown, and I am no exception. While I didn’t know for sure what to expect from a pain perspective, I was pretty certain it was going to be awful. Things could not have gone better for me once I entered the hospital. I received excellent care and attention, starting with the folks in reception and registration who speedily got me on my way. The nursing staff was stellar—from the nurse who took the clotting test and drew my blood to the nurse who hooked me up to the IV and finally the nurse who went over my medical history. And I’ll never forget the nurse who brought me extra blankets. On one of the busiest of days, this special staff managed to keep me calm with their easy conversation and sense of caring. Then I was wheeled off to see Joey Phillips in Radiology. What a guy! The first thing he noticed was that I am eight days older than he. After some kidding around, he explained the procedure, potential complications and results. He showed me my organs on the ultrasound, answered all of my questions and kept me relaxed. Had I been able to consult with him when the procedure was scheduled, I would not have worried for two weeks. All right, I probably wouldn’t have slept the night before, but that’s expected. Dr. David Furie walked in, asked if I was ready and began. I’d have to say that the whole procedure was over in three minutes. “That was a piece of cake,” I told him. To which he responded, “Maybe it was for you.” I was overjoyed to know that it was over, that I did fine, and that I could look forward to six hours of bed rest. I want to congratulate you on your exceptional team of professionals who perform with grace, good humor and caring. I would not hesitate to recommend Moore Regional Hospital to anyone requiring medical attention in a first-rate facility. I would also like to thank Dr. Bruce Solomon for his referral of Dr. David Martin, who continues to monitor my condition.
Ultrasound technologist Joey Phillips (seated) and radiologist David Furie, M.D.
Diane Lisevick Pinehurst
For more information on these or any of the services provided by FirstHealth of the Carolinas, please call (800) 213-3284. www.firsthealth.org
25
Great programs and facilities
T
his letter is written in appreciation for the excellent care I received while in FirstHealth Richmond Memorial Hospital and FirstHealth Moore Regional Hospital. On July 30, 2009, Dr. Peter Duffy inserted a stent to open a blockage in my heart. When I left the hospital, it was recommended that I participate in the Cardiac Rehabilitation program. I was somewhat reluctant, but I did decide to attend. It has truly been a great decision. After completion of the Cardiac Rehab program, I joined the FirstHealth Center for Health & Fitness Center-Richmond and have continued to exercise on a regular basis. The people of Richmond County are so Melissa Stewart, Cindi Leshko and Betsy fortunate to have such a facility. Enough cannot be said Young of the Cardiac Rehab team for Rockingham and Pembroke about the rehab program and the great staff. Special thanks go to Melissa Stewart, Betsy Young and Cindi Leshko (Cardiac Rehab, Rockingham/ Pembroke) for all they did to help me and the many others who have completed the program. They were very professional, competent, friendly, kind and dedicated in helping each person in their recovery. n the morning of May 2, 2010, our very seriously Thank you and FirstHealth of ill brother/uncle was brought into the emergency the Carolinas for providing the room at FirstHealth Richmond Memorial much-needed facilities that serve Hospital. On May 26, he was transferred to a skilled the medical needs of Richmond nursing center for rehab. A miracle! and surrounding counties. We want to thank you all for your knowledge in knowing how to respond to his emergency, the quickness in which G.R. Kindley you all so earnestly worked, and especially the care and Rockingham concern for him and his family. God bless you all.
A great response from the RMH ED
O
Otelia McDonald Sandra Long Rockingham
26
Fall 2010
The best ED anywhere
I
was recently in the Emergency Department at FirstHealth Moore Regional Hospital and wanted to write you with a few comments. I am a retired anesthetist and know how seldom health care providers get positive feedback or hear good things about themselves. My care in your ED was excellent—the absolute best I have had anywhere, ever. My nurse, Vicky Jorgensen, and my physician, Dr. Matthew Reinhardt, were efficient, attentive and reassuring. It was truly amazing to me that this caring attitude prevailed with everyone I met—the registrar, the triage nurse, the nursing assistant who took me to Radiology and the technician who did my CT scan. My daughter-in-law, who works in the lab there, assured me that these characteristics pervade throughout the hospital. I’m impressed! And kudos to your housekeeping department. The hospital is noticeably spotless! Martha Lou Kirkland Southern Pines
Vicky Jorgensen, R.N., and Matthew Reinhardt, M.D., of the Emergency Department at FirstHealth Moore Regional Hospital
Employees make Moore Regional special
S
ince my heart attack and bypass surgery, which led to other problems, I realized what a terrific bunch of people I work with all over the hospital I wish to express my heartfelt gratitude to each one for all the prayers, thoughts and inquiries to my well-being. The phone calls and cards were appreciated, as well as the visits. I’d like to say a special thanks for the milkshakes, flowers, T-shirts and that wonderful bowl of New Year’s black-eyed peas. There were some who even gave me money. I would also like to thank those who took time to work on my hair, cut and style it. You did a beautiful job. Even after I came home, people still thought about me and sent me cards, money, bags of goodies to make me fat again and other things I could use. They also called to say “hello” and see how I’m doing. I would love to thank each one with a personal thank you, but I’d have to send one to everyone there, so I might as well do this: Thank you to each person for any and all things. I do want each person who took even the smallest part of my stay there to know their work is appreciated by me. Thank you! You are what makes this hospital such a pleasure. Sarah F. Butler Environmental Services FirstHealth Moore Regional Hospital
For more information on these or any of the services provided by FirstHealth of the Carolinas, please call (800) 213-3284. www.firsthealth.org
27
I
t’s been called the sandwich generation—that period of life when many adults are working hard to establish themselves while taking care of children and aging parents. Juggling the responsibilities isn’t easy. Managing a job, school, a home, errands and the needs of your loved ones can seem a lot like walking a tightrope. FirstHealth Response offers a safety net for those times when things get a little out of balance. A personal emergency response service based at FirstHealth Moore Regional Hospital, FirstHealth Response provides 24-hour assistance and is available to residents in Hoke, Lee, Montgomery, Moore, Richmond, Scotland and surrounding counties. A monthly fee covers the cost of the equipment and monitoring service. Each subscriber receives a lightweight, comfortable Personal Help Button that should be worn at all times—on a neck chain or wrist band or clipped to clothing. Also provided is an Emergency Home Communicator, an electronic device about the size of an answering machine that connects to the telephone line. When help is needed, a simple touch reaches out to a monitoring center in Pinehurst. Trained personnel receive the signal and immediately attempt to help—first by calling the subscriber’s home, friends or relatives on a contact list. If the situation is serious, they contact emergency personnel.
By Erica Stacy
The personal safety net of
FirstHealth Response 28
Fall 2010
FirstHealth Response at work Ida Mae Steele is 94. She lives in Mt. Gilead with her son, Thomas, who attends classes every day. He didn’t like leaving his mother at home alone, but his choices were limited. “She isn’t always steady on her feet and falls a lot,” he says. “I worried every time I left and even when I was just in a different part of the house. What if I didn’t hear her? What if she got hurt? What if I wasn’t home?” A year ago, Steele subscribed to FirstHealth Response. “We’ve had to use it on two occasions so far,” he says. “I was amazed at how quickly they responded. It seemed like as soon as she pushed the button the ambulance was here to help.” FirstHealth Response is a helping hand for families who are caring for loved ones. It offers security, safety and, just as importantly, peace of mind. “I feel more secure when I have to be away,” says Steele. “The whole family is happy we have it. I have even recommended it to several other people. I wouldn’t have it any other way—or with any other organization.”
Safe, reasonable and convenient Jody DeNauro says FirstHealth Response isn’t just for older people. “It doesn’t matter what your age is,” she says. “Anyone who lives alone would benefit from FirstHealth Response.” DeNauro should know. She is active and healthy and takes every opportunity to enjoy the “golden years.” Both she and her late husband, Anthony “Tony” DeNauro, have been volunteers at FirstHealth Moore Regional Hospital. More than 10 years ago, Tony DeNauro, who had diabetes, began to suffer from various medical complications. Getting out became a challenge, and Jody worried when she had to leave him home alone— even if she was just making a quick run to the grocery store. That’s when the couple decided to subscribe to FirstHealth Response. “My husband was an amputee,” DeNauro says. “He had numerous health issues—mostly related to diabetes. He fell a lot, and I couldn’t pick him up. When I needed someone I could depend on, FirstHealth Response was there. Just knowing that with the push of a button help was on the way made all the difference.” DeNauro was able to run needed errands, go to appointments and still feel secure—knowing that her husband would be safe in her absence. “It helped me slow down,” she says. “I didn’t feel I had to rush to get home to make sure that he was OK. In some ways, I felt that I had had a weight lifted off my shoulders. I didn’t have to spend every moment worrying about what was happening with Tony at home. For the first time in a long time, I felt safe.” When Tony passed away in August 2009, Jody decided to keep FirstHealth Response. “You never know what might happen,” she says. “I feel secure, even at night, knowing that I can reach someone if I need help. It’s safe, reasonable and convenient. It absolutely provides peace of mind, night and day. It’s another plus for getting FirstHealth Response.” n
Subscription information
The cost for a monthly FirstHealth Response subscription is $21 for Moore County residents and $23.50 for residents of all surrounding counties. For more information about FirstHealth Response, call (800) 213-3284.
www.firsthealth.org
29
Volunteering How to and why By Erica Stacy
Care at the end of life
R
eaching out with kindness is a way of life in the mid-Carolinas. Neighbors help neighbors. Friends support friends. Families care for each other. Across the region, there are numerous examples of individuals giving back to the community, inspiring the future by extending their hands in old-fashioned service delivered from the heart. Across the FirstHealth of the Carolinas network, more than 1,000 volunteers contribute more than 100,000 hours to FirstHealth services each year. They help patients and visitors navigate the hospitals. They support families during times of crisis. They make toys for children. They provide leadership on boards and 30
Fall 2010
Volunteers at FirstHealth Hospice & Palliative Care understand letting go. They provide unique services that support staff and families as patients near the end of life. “Supporting patients throughout Moore and Montgomery counties is an ongoing challenge,” says Volunteer Coordinator Susanne Martínez. “Obviously, all of our patients don’t live in downtown Pinehurst, Southern Pines or Aberdeen. We always need more volunteers to provide patient support, especially in Montgomery County and the northern and western areas of Moore County.” Hospice volunteers serve in three primary areas: n Patient/Family volunteers support the family by providing companionship, running errands and sitting with patients for a while to give caregivers a break. Bereavement volunteers can provide similar support for family members after the death of a patient. n Special Projects volunteers assist with special events and serve on committees. n Administrative volunteers support the office staff as needed.
committees. They operate transport shuttles, make copies and deliver supplies. These generous, giving people are retirees, stay-at-home moms, teens, business leaders and ministers. Every day, they extend a helping hand. “Our volunteers are an inspiration,” says Cindy Strother, administrative director of Guest Services at FirstHealth Moore Regional Hospital. “There is no way to measure the real value they bring to our organizations. As we add new services to the hospitals, our volunteers are ready and willing to explore new opportunities to share their compassion through service.” In the fall of 2010, with the opening of the new Reid Heart Center, FirstHealth volunteers will take on a new role. “We anticipate having around 15 to 20 volunteers dedicated to the heart hospital,” says Strother. “However, service in this area will be a very different concept from the one we have traditionally used at Moore Regional.” A Reid Heart Center volunteer will function much like a concierge in a large resort or hotel, managing multiple tasks that range from providing information to acting as a liaison to families and escorting patients to various areas of the hospital.
“We are looking for people who have a high-energy level, are confident and customer-oriented, comfortable with technology, flexible and physically active,” says Strother. “They will be operating equipment from laptop computers to wheelchairs.”
Cardiac CARE-Net The Cardiac CARE-Net program will provide another new opportunity for volunteers through the Reid Heart Center. Based on a successful program that has served oncology patients at Moore Regional for several years, Cardiac CARE-Net matches trained volunteers with cardiac patients. Many of the program volunteers have personal experience with cardiac issues, either as a patient or caregiver, so they understand the anxieties and concerns associated with the disease. However, personal experience with cardiac issues is not a requirement. “As we implement the program in the heart hospital, we initially plan to serve patients who have undergone bypass surgery or other surgical procedures,” says Laura Kuzma, Cardiac CARE-Net coordinator. “However, there are plans to make the program available to additional cardiac patients in the future.”
From the heart “I started volunteering about three or four years ago,” says Judi Giles of Pinehurst. “After my husband died, it was a way to give something back. I am proud to do it for him, and for the others who benefit from our services.” Giles, an escort guide, is available to help patients and visitors navigate FirstHealth Moore Regional Hospital. “Sometimes I give them directions, but often I take them directly to the area myself. It can be confusing when you are trying to get around the hospital, especially if you are worried about your health or that of a loved one.” Giles enjoys being helpful and highly recommends volunteering. “There are so many different areas,” she says. “There is something to fit every personality. It just makes you feel good to know that you are making a difference, no matter how small it might seem at the time.”
Having a purpose Seven Lakes resident Mel Anderson hopes to volunteer at the Reid Heart Center beginning this fall. “I had a heart problem myself about two years ago,” he says. “I had surgery to replace a valve and repair an aneurysm. It saved my life. I’m living proof that you can come back after heart disease. My experience gives me a purpose. If I can use my illness to take away someone else’s anxiety, it’s a good day.” Anderson has volunteered off and on since he retired. The former accountant relocated to Moore County about four years ago and began volunteering at FirstHealth Moore Regional Hospital. He currently works in Patient Registration. “I greet patients, direct them to where they need to check in and escort them to the department they need to see when they are called,” he says. “There’s no age limit on giving back to your community,” Anderson adds. “If you think you might want to volunteer somewhere, try it. Share your experiences. If you don’t like it, try something else. There’s always something you can do to help no matter what or where.”
www.firsthealth.org
31
Cardiac CARE-Net volunteers provide emotional support and encouragement through visits, phone calls and letters. They also link patients with community support and assistance as needed. Over time, true friendship often emerge as Cardiac CARE-Net volunteers work one on one with patients and families. They set their own schedules, devoting as much time as they feel is needed to support each patient and family.
Interviews, education and training Anyone who is interested in volunteering at a FirstHealth facility is encouraged to contact the volunteer coordinator for that area and complete an application. “Once an individual makes contact, we will set up a time to talk with them,” says Mandy Phifer, the volunteer manager for
Want to volunteer?
If you are interested in learning more about volunteer opportunities at FirstHealth of the Carolinas, please contact: n Cindy
Strother FirstHealth Moore Regional Hospital (910) 715-1266
n Tina
Thompson FirstHealth Montgomery Memorial Hospital (910) 571-5020
n Mandy
Phifer FirstHealth Richmond Memorial Hospital (910) 417-3432
n Laura
Kuzma Cardiac CARE-Net lkuzma@firsthealth.org (910) 639-0001
n Kathy
Milewski CARE-Net (910) 695-7507
n Susanne
Tyndall Martínez FirstHealth Hospice & Palliative Care (910) 715-6000
32
Fall 2010
FirstHealth Richmond Memorial Hospital. “During that discussion, we try to get a feel for what they are interested in doing so that we can match them with the right position. Different positions require different skills. We want to be sure our volunteers enjoy the time they spend with us so that they want to keep coming back.” All FirstHealth volunteers receive a special orientation and on-the-job training. “The type of education varies from location to location,” says Strother. “Some of our volunteers complete online programs; others participate in group education sessions. You will be informed of the expectations during your interview.” Each of the three FirstHealth hospitals offers special summer volunteer opportunities for teens who are 14 years of age and older. Interested young people should contact the hospital of their choice for more information. n
Opportunities in Montgomery County At FirstHealth Montgomery Memorial Hospital, volunteers greet patients in the main lobby and the outpatient center. They offer information on how to find departments and answer any questions visitors may have. “Our volunteer program is unique,” says Volunteer Coordinator Tina Thompson. “We have an Auxiliary made of individuals from the community who want to support our local hospital. Some of them actually have volunteer positions, but many simply participate in fundraisers and help out with special events. We are always looking for new Auxiliary members.” The MMH Auxiliary hosts the hospital’s annual Lovelight Tree, provides funding for the spring Teddy Bear Affair, and sponsors a book fair and bake sales to raise money to support the hospital.
Reaching out in Richmond County Around 25 volunteers dedicate their time to FirstHealth Richmond Memorial Hospital in Rockingham. They serve as greeters, transporters and in various offices throughout the hospital. “Our volunteers offer a helping hand to the staff and ultimately enhance the personal care that patients and families experience when they visit the hospital,” says Volunteer Manager Mandy Phifer. Phifer encourages interested individuals to come to the information desk or stop by the hospital gift shop. “Once we have your completed application and background check, we’ll find the perfect spot for your skills,” she says.
FirstHealth Mobile Health Services offers three preventive screenings in the comfort and convenience of its mobile unit. Screenings are conducted using painless, non-invasive ultrasound technology. Screenings are for those 18 years and older.
Take charge of your health with three simple screenings. Abdominal Aortic Aneurysm (AAA) Stretching and weakening of the aortic wall can eventually cause the aorta to burst or rupture, leading to life-threatening bleeding. Risk factors: hardening of the arteries, genetics, injury to the abdomen and aging. Men who have smoked more than 100 cigarettes during their lives are also at increased risk.
Thursday, November 4 Hamlet Senior Center- Richmond County 9 a.m. to 2 p.m.
Saturday, November 6 FirstHealth Center for Health & Fitness- Pinehurst 9 a.m. to 12 p.m.
Thursday, November 11 FirstHealth Center for Health & Fitness- Southern Pines
Stroke Screening / Carotid Artery
9 a.m. to 2 p.m.
Carotid artery disease is the number one cause of stroke in the United States. Plaque buildup on the artery walls restricts blood flow to the brain, causing a stroke.
Saturday, November 13
Risk factors: family history, age, smoking, high blood pressure, diabetes, obesity and lack of exercise.
FirstHealth Center for Health & Fitness- Pinehurst 9 a.m. to 12 p.m.
Thursday, November 18 FirstHealth Center for Health & Fitness-Raeford 9 a.m. to 2 p.m.
Peripheral Vascular Disease (PVD)
Saturday, November 20
Plaque buildup in the arteries limits the blood supply to the body’s muscles, organs and tissue, which may lead to the loss of limbs.
9 a.m. to 12 p.m.
Risk factors: smoking, diabetes, excess weight, lack of exercise, high blood pressure, high cholesterol and age.
Montgomery Senior Center- Troy
Appointments required, call (888) 534-5333. Please plan on spending 30 minutes for all three screenings.
Pricing Information* $85 for all three screenings $60 for two screenings $30 for one screening Financial assistance available for those who qualify. *Please note that insurance, including Medicare, does not cover preventive screenings.
FirstHealth Center for Health & Fitness- Southern Pines
Thursday, December 2 9 a.m. to 2 p.m.
Saturday, December 4 FirstHealth Center for Health & Fitness- Southern Pines 9 a.m. to 12 p.m.
Thursday, December 9 FirstHealth Center for Health & Fitness- Richmond 9 a.m. to 2 p.m.
w w w. f i r s t h e a l t h . o r g 878-103-10
NON-PROFIT U.S. POSTAGE PAID PERMIT NO. 4 LONG PRAIRIE, MN
155 Memorial Drive P.O. Box 3000 Pinehurst, NC 28374
Because we use a variety of sources for mailing, duplications sometimes occur. Please pass an extra copy along to a friend or neighbor.
firsthealth.org
titled-1 1
8/13/04 9:05:06 AM
People living with diabetes face many challenges. We offer more solutions. The FirstHealth Wound Care & Hyperbaric Centers at Moore Regional Hospital and Richmond Memorial Hospital are specially equipped to treat diabetic wounds with Medicare-approved advanced treatments including hyperbaric oxygen therapy, which is proven to increase healing success. Get back to doing the things you love. If you have a wound
ir Diabetes Hea10 lta.mh. - Fa 2 p.m. Saturday, Oct. 23 •
Building in Pinehurst FirstHealth Specialty Centers , call For more information
(8 00) 2 13-3284
that has not healed, we have solutions. Our state-of-the-art wound care offers a comprehensive pathway of care. Call (910) 715-5901 in Moore County or (910) 417-3636 in Richmond County and find out how we can expand your treatment options.
www.firsthealth.org
569-40-10