FRANCA MELFI IS THE FIRST WOMAN TO BE VICE

As the new Secretary General of EACTS I would like to thank all of you for being part of this year’s successful Annual Meeting. With your support the EACTS Annual Meeting continues to be not just the largest event for the cardiothoracic community, but also an opportunity for us all to come together, share, discuss and learn.



EACTS has its roots in Europe, but I’m delighted that members and speakers from all over the world as well as from other specialities and professions have joined us in Milan. As cardiothoracic surgeons, we work in multi-disciplinary teams, and I’m so pleased that our Domains and Task Forces truly embraced the importance of multi-disciplinary approaches when they prepared the huge scientific programme on offer here.
Cutting-edge science
It has been fantastic to hear from global leaders in their field and learn more about the cutting-edge science that we can implement in our practice. In yesterday’s Late Breaking Clinical Trials session, we were privileged to have high quality presentations, including the results of a prospective
A SUCCESSFUL ANNUAL MEETING
randomised controlled trial. I encourage everyone to attend today’s Late Breaking Clinical Trials session at 12:15, which is an opportunity to hear the preliminary results of a first in human trial which could improve coronary artery bypass grafting.
New initiatives to support our members I am extremely humbled to be the new EACTS Secretary General. As a longstanding member of the organisation, past secretary of the EBCTS and Chair of the Acquired Cardiac Disease Domain, I know first-hand the influence that EACTS has through our publications, Academy programme, clinical practice guidelines, examinations and the many other facets of work. I want to build on these achievements and explore new ways to deliver value to our members whilst continuing to equip the cardiothoracic community with everything we need to improve outcomes for our patients.
A stronger surgical voice
Assessing the very latest clinical data and evidence in order to develop high quality clinical guidelines on specific procedures and techniques is an important part of our efforts to drive quality improvement in cardiothoracic surgery. However, we need to strengthen the surgical voice by taking a more active and earlier role in how the evidence is developed.
At this Annual Meeting we have been able to learn from experts running clinical trials and, given the numbers of submissions we received, we are able to hold two late breaking clinical trials sessions as well. These sessions encourage us all to assess and critically appraise the evidence available to us.
Running a clinical trial is a full-time job which requires specific expertise. We want to put the infrastructure in place to support more members gain the necessary skills and knowledge to design and run the clinical trials that will lead to surgical teams delivering even better outcomes for our patients. Other professions do this well and I am keen we do more to support in this area. As such, we are working with the University College London
Patrick Myers EACTS Secretary General
“Assessing the very latest clinical data and evidence in order to develop high quality clinical guidelines on specific procedures and techniques is an important part of our efforts to drive quality improvement in cardiothoracic surgery.”
WELCOME
Comprehensive Clinical Trials Unit and other trials units to develop this new service for our members.
Supercharging innovation Innovation in cardiothoracic surgery is critical as we seek new ways to improve patient outcomes. As surgeons we often have a lot of ideas, but we don’t always know how to turn these ideas into real world applications to use in everyday practice. The Techno-College Innovation Award at the Annual Meeting provides great exposure to innovations, and we want to create more opportunities to help get the most innovative ideas into practice.
We’re working with potential funders to get their input on how we can support the best start up ideas as well as creating a network of experts, including industry contacts, that we can harness within EACTS for the benefit of our most innovative members.
Quality improvement
Across all aspects of medicine, quality improvement is primed to make care better for our patients. EACTS has a fantastic quality improvement programme The EUROMACS registry is already considered the standard for Europe. With several countries having mandated reporting data to EUROMACS for any ventricular assist

devices. This is a great achievement, but we need to continue to develop our quality improvement databases and take them to the next level, expanding the Adult Cardiac surgery Databases (ACD) and renewing the QUIP committee. Several countries have national databases; we are taking the steps to regroup these into our ACD, to harness big data covering all of Europe. Over the coming months we will be exploring options such as recognising and accrediting those organisations that participate in the Adult Cardiac Database and are achieving outstanding outcomes.
Thank you Rafa
Finally, I would like to thank our outgoing Secretary General, Rafa Sádaba, for his wonderful leadership over the past few years, guiding the organisation through the challenge of a global pandemic whilst demonstrating an unwavering commitment to delivering value for our members. He has made a huge contribution to the growing success of the organisation and I am delighted that Rafa will continue as Chair of the Education Committee and as a member of EACTS Council.
We stand on the shoulders of giants, and I look forward to the support and guidance from all of our members in developing your Association further.
YOUR ANNUAL MEETING HIGHLIGHTS
Fatma Ashkanani, Kuwait


“It's ver y important for me as a young Resident to come to the Annual Meeting and learn interesting things from experts in cardiothoracic surgery and see new techniques we will be able to use in the future.
I am enjoying meeting other women in cardiac surgery. I am currently working in Ulm and there are no other women there so going to the women’s reception and catching up with other colleagues from other centres is important for me while I am here.
I'm originally from Kuwait and once I pass my exams I will be the first woman cardiac surgeon in Kuwait so I am very excited.
I hope I will be at EACTS in Vienna next year.”
Mohamed Elfiky, Egypt
“This is one of the biggest societies in the world. Milan is not far from Egypt and it’s a lot closer than going to the United States meetings. It covers all aspects of cardiac surgery so it’s a good way to keep on top of the subject.”
Ourania Preventza
“I am a Professor of Surgery in Texas and I am very glad to be here this year to see friends again and hear the latest in cardiothoracic surgery.
The Meeting is very vibrant and you see a lot of new faces and here in Europe we see all the latest and the greatest regarding innovation and technology so I really love it.
I have enjoyed the topics on minimally invasive valve surgery, robotic mitral valve and aortic valve repair
One of the highlights was the women in cardiothoracic surgery session - that was amazing. I am very glad that the association is attracting so many talented women.
If you haven't been to a Meeting before, this is the Meeting to come to. I'm looking forward to attending next year's meeting in 2023.”
Lorena Montes
“I am so pleased to travel all the way from Columbia - it was a seventeen hour flightbecause this is one of the largest meetings in the world. It’s my first time and I am very very excited to be here. I have been meeting incredible people here; all the Masters and the people that are admired in cardiovascular surgery are here.

In Latin America, LVADs is a growing area right now, but it has been dominated by male surgeons. Two weeks ago I was the first woman surgeon in Latin America to use the heartmate 3 in an adult patient.”
Pei Pei Chow, Singapore
“This is my first time in Milan and my first time attending EACTS. The conference is awesome and there are a lot of positive vibes. Everybody is happy to see one another and there is a lot of knowledge sharing. There’s a lot of new things and new technology that I’m seeing here.”


HIGHLIGHTS FROM FRIDAY
Embodied leadership
The Women in Cardiothoracic Surgery committee (WiCTS) hosted a stimulating workshop exploring the various ways of practicing personal power in order to achieve objectives.
Participants learnt the most common unwritten masculine and feminine rules in the game of power and leadership and discussed how these rules intersect with power of profiling and visibility and power of reflection.
Presidential address
Friedhelm Beyersdorf gave his highly anticipated Presidential Address in which he spoke about the need for surgeons to implement disruptive innovation in the near future in order to deliver new ways to improve patient outcomes and save lives.

Friedhelm says, “In my presidential address I have tried to explain a little bit of the so-called untreatable diseases and what can be done to date. I highlighted a few examples but there are many more.
“These are not only ideas and thoughts. There are already basic science papers and even clinical papers out that show that a completely new therapeutic option exists. Of course, there need to be further development. But for the future I see many opportunities and for the young people in our field this is the perfect time to start cardiothoracic surgery.”
Late Breaking Clinical Trials
Due to the number of outstanding submissions to the Late Breaking Clinical Trials session there are two ses sions taking place this year. The first session on Friday included a presentation on the CAST-HF which could possibly change the way we do CABG in patients with ischemic cardiomyopathy.

The STICH3 trial asks questions about whether we should do things differently. This is one of the first trials where we have a significant point estimate using shockwave therapy. There was also outstanding data presented from the SWEDEHEART registry looking out over 17,000 patients undergoing CABG.

EACTS GENERAL ASSEMBLY 2022
We are delighted to welcome new Officers and Councillors to the EACTS Council following yesterday’s EACTS General Assembly. The following positions were announced
Franca Melfi Vice President"For me it is a great honour to become Vice President of this society. EACTS was the first scientific society that I joined - back in 1998. I am looking forward to promoting EACTS membership, including to thoracic surgeons, to highlight the importance of supporting women and men into leadership roles, and making EACTS a home for technological advances and innovation."
 Rafa Sádaba Education Chair
Rafa Sádaba Education Chair

"Education is at the heart of our work and, as Chair of the Education Committee, I am focused on delivering meaningful learning opportunities for our members that enhance skills and expertise to improve clinical practice. EACTS offers our members the very latest science, hands on training and high quality learning from global experts."
Filip Casselman Acquired Cardiac Disease Domain Chair




"I am delighted to be leading the Acquired Cardiac Disease Domain and to have the privilege of working with a huge array of experts. It’s an enormous domain with multiple task forces all working to push the boundaries in our specialty as we strive to always improve outcomes for our patients."


Nabil Hussein Resident Chair
"It's a great honour and privilege to be part of the Residents Committee. I never thought when I joined a few years ago that I would be in this position. The position comes with great responsibility, but I am blessed to be working with such a great team. We are driving towards increasing the exposure Residents get in EACTS - something that EACTS are supporting us with. Looking to the future, we will be supporting Residents from all over the world, including them in EACTS and demonstrating that we are there for them, we are there to support their training and are open to their ideas."
After three successful years Rafa Sádaba stepped down as Secretary General and handed over to EACTS’ new Secretary General, Patrick Myers. In addition, at the Presidential Dinner on Friday evening, Friedhelm Beyersdorf passed on the Presidential chain to EACTS’ new President Patrick Perier.
EACTS Council is the decision-making body of EACTS. The Council is responsible for ensuring EACTS complies with its governing document, relevant legislation and best practice guidelines. Members of the EACTS Council have an active role in providing strategic direction to EACTS and setting overall policy and targets. Councillors serve a set term (normally of up to three years).
WITH THANKS
We would like to thank the following outgoing Officers and Councillors for their hard work and valued contribution to our organisation.
Mark Hazekamp Alicja ZientaraEACTS AWARDS
CELEBRATING TRAINING AND RESEARCH EXCELLENCE
Each year
Annual Meeting.
Abstract No.
T. Langenaeken, Leuven, Belgium
In vivo performance of a trileaflet heart valve
in an ovine model
THORACIC WINNER

Abstract
W. Woo,
Predictive
of

Abstract No. 132
D. Aronowitz, Philadelphia, USA
Early impairment of Cerebral Bioenergetics after Cardiopulmonary Bypass in Neonatal Swine
EACTS/STS AWARD 2022 WINNER


Abstract No. 000111
M. Luehr, Cologne, Germany
Acute Type A aortic dissection in adolescents and young adults under 30 years of age: incidence, etiology and postoperative outcomes of
cases from a large multi centre cohort of
patients
HANS G BORST ANNUAL AWARD FOR THORACIC AORTIC SURGERY WINNERS
This Award, in honour of the late Professor H G Borst, leading European surgeon of thoracic aortic surgery and one of the founders of the EACTS, aims to stimulate advanced clinical or experimental research in this field by young investigators as documented by an outstanding presentation during this year’s Annual Meeting.

Abstract No. 000459
F. Irace, Rome, Italy
20 year follow up of aortic valve reimplantation using the Valsalva graft

Abstract No. 001051
A. Iyengar, Philadelphia, USA
Mitral regurgitation in Acute Type A dissection: management and outcomes

EACTS/GJC-PASCATS Excellence Award WINNER
EACTS and the Pan-African Society for Cardio-Thoracic Surgery, are proud to announce a new prize for the best presentation on “Rheumatic Heart Valve Repair and Aortic Reconstruction”, presented during the annual Joint EACTS/PASCaTS session at this year’s Annual Meeting.

E. Girdauskas, Augsburg, Germany
Standardized subannular repair in type IIIb mitral regurgitation: 1-year results from REFORM-MR Registry


MARKO TURINA AWARD FOR BEST MMCTS RESIDENTS’ TUTORIAL
The Marko Turina Award is presented in recognition of the best core skills video tutorial. This follows a competition, launched earlier this year by EACTS and TSRA (Thoracic Surgery Residents Association) to recognise the best core skills video tutorial with a specific focus on technical quality, surgical skills and educational clarity.
WINNER
Veronica Lorenz
How to perform a direct axillary artery cannulation

“I am very grateful and honoured to win this prize. MMCTS is an important resource and a stimulus for Residents because it allows us to directly update ourselves on surgical skills and interventions.
“I decided to do a video about axillary artery cannulation after one of my resident colleagues and friend expressed her concern about performing the isolation of the axillary artery by herself. I therefore decided to make the video simple and intuitive, hoping to be of help to other residents like me and my colleague.”
EACTS LEARNING LAB
IN THE EACTS LEARNING LAB
Learn specialist techniques and draw on the knowledge of some of the world’s most experienced and expert surgeons with the EACTS Learning Lab training sessions. These ‘hands-on’ workshops include wet and dry labs and other small practice sessions. These can only be purchased upon registering for the 36th EACTS Annual Meeting and are available to book now.


SATURDAY 8 OCTOBER
Coronary Surgery
Learn how to perform coronary anastomoses and the techniques for proximal and distal anastomoses, sequential and composite grafts. Techniques and devices for conduit harvesting and methods for intraoperative graft assessment will also be presented.


"During the summer we played in some preliminary rounds. It's been a long process and I am very happy that my partner and I were lucky enough to win. In January we will cross the pond to the STS and compete against the American winners. It's a great motivation to study and try and beat them in their own territory."
Sam Heuts
We went in with an open mind and we got lucky to play the final. Winning the European final feels great. We are looking forward to the world finals - it's a great opportunity to meet our colleagues the other side of the ocean. We will participate on 22 January and have to defend the honour of the EACTS and European societies. We can beat everyone!"
Jules OlsthoornThey will now go on to compete against the winning North American team at the STS Annual Meeting in 2023 where the CT Surgery Masters World Champions will be crowned.

















HANS GEORG BORST, MD A EUROPEAN SURGEON
Axel HaverichDr Hans Georg Borst died on 8 September 2022, aged 94. As President of EACTS in 1995, he addressed the Annual Meeting in Paris on the topic: “A European surgeon´s odyssey”1 . This characterises both his academic life and his devotion to his mother continent. It also reflects Hans´ intense desire for international partnership, far beyond cardiothoracic surgery. Like Odysseus, he did not trust in travelling alone. To strengthen his new discipline, cardiothoracic surgery, he founded two scientific societies together with peers: the German DGTHG in 1971, and EACTS in 1986. To enhance scientific communication, both societies launched their own journal and Hans became the editor-in-chief for both.
Becoming a cardiothoracic surgeon
Hans Borst was born on October 17 in 1927 as the son of Max Borst, late Professor of Pathology at Munich university. In early 1945, he was drafted into the Luftwaffe, the German Air Force, and subsequently spent six months in a British POW-camp. Upon returning home, he continued his studies and graduated in 1947. As a requirement before starting medical training at Munich university, Hans Borst had to work for six months as a construction labourer. After completing his preclinical training, he was granted a stipend to study at Harvard Medical School in the US, where he graduated in 1953.
Supported by Frank Gerbode, a pre-war assistant in his father´s institute in Munich, he became an intern in the Department of Surgery at the old Stanford Hospital in San Francisco, before completing a two-year fellowship at the Department of Physiology, Harvard School of Public Health in Boston.
Returning to Germany in 1956, he moved to Rudolf Zenker’s clinic in Marburg and was given responsibility for operating the heart-lung-machine, including the first time it was used successfully to close an atrial septal defect in Germany on 18th February 1958.
In 1968, he was appointed Professor of Surgery at the Hannover Medical School. This was the time when Christian Barnard hit the headlines internationally with the world’s first heart transplant operation. Borst visited the Groote Schuur Hospital in Cape Town with a Munich delegation to familiarise himself with Barnard's surgical procedures and treatment protocols. Not least because of this experience, Hans Borst saw a future surgical field in organ transplantation.

Science based innovations
Borst was constantly devising techniques and important surgical innovations to improve patient outcomes. Inspired at congresses, read in magazines or born out of his own creativity, Hans Borst always had the urge and courage to design and carry out better interventions. For some procedures, the risk halved during his time as a surgeon, for others, such as bilateral lung transplantation, it fell to a fifth.
His spirit and innovative strength were transferred to his younger colleagues. He constantly encouraged dedicated assistants to examine this and test that, or to visit other centres.
Surgical teacher and mentor
He entrusted inexperienced co-workers with graduated steps of the surgical procedure under his supervision and left the responsibility to younger ones if he left the operating table early. Whether through impatience or by design, that concept worked.
Loss of a leader
With the death of Hans Georg Borst, his students have lost a charismatic teacher and a role model whose uncompromising responsibility for the wellbeing of individual patients in clinics and research are written in letters of gold. His tireless commitment to the medical and academic advancement of his staff has given many the opportunity to adopt his high standards for their own surgical work.


With Hans Georg Borst we are all losing a leading figure in European surgery of the last century.
For the community of surgeons, even during his lifetime, he was a monument at a special time.

As the possibilities offered by heart surgery unfolded, Hans became convinced about the enormous potential of heart surgery for the treatment of conditions such as coronary artery disease and the management of heart attacks, which were the most common causes of death in western countries even at that time.
Hans, we will not forget you, we will keep the memory of you and your legacy with honour.
Q. Where did you carry out your training?
• Cardiac surgery residency at University of Milano, Italy
• Cardiac Surgery fellowship at Cleveland Clinic, Cleveland, Ohio, USA.
Q. What are your main areas of interest within cardiothoracic surgery?
To promote and provide unbiased, critical and unconflicted evidence in cardiovascular medicine. Mentoring, Advanced statistical models, Biomarkers and translational medicine, Coronary and valve diseases and Residents training.
Q. What are your interests outside of your work?
Biking, swimming, playing piano.
What have we learnt?
The never-ending debate about the optimal treatment of triple-vessel coronary disease has been recently heated by the publication of the FAME 3 trial results, designed to test the noninferiority of PCI when target lesions are identified by FFR compared to standard coronary artery bypass grafting.
In FAME-3 non-inferiority trial 1500 patients were randomly assigned to undergo standard CABG or FFR-guided PCI; the hypothesis was that being fractional flow reserve a possible way to improve outcomes of PCIs this would have


led to equivalence between CABG and FFR in the complex scenario of triple vessel disease. Lesions with a pressure-wire FFR of 0.80 or less were stented and those with higher FFR readings were deferred.
Although the one-year hazard ratio (HR) for the primary endpoint – a composite of death from any cause, myocardial infarction (MI), stroke, or repeat revascularisation – did not reach the criteria of inferiority, the pre-specified choice of noninferiority margin has raised several concerns, as it defines non-inferior a hazard of composite endpoint higher up to 65%. Moreover the 1.65 noninferiority margin has been increased from a prespecified 1.45 value during the trial enrolment. Is it acceptable that a treatment with an observed 50% higher risk of composite endpoint at one year (HR 1.5, 95% CI 1.1 - 2.2) is considered non inferior to the control?
“In the session “What should we learn from FAME 3?” a panel of experts in statistic, cardiology and cardiac surgery will discuss all the strengths and flaws of FAME 3, including the trial design, the results and their interpretations”, says Fabio Barili, the Head of the EACTS Research and Methodology Task Force.
The in-depth analysis of the FAME 3 trial suggests that the non-inferiority of FFR-guided PCI might instead emphasise the superiority of CABG for triple-vessel coronary disease. A deep knowledge of this trial is of paramount importance for the practice of surgeons and cardiologists, and this session is a good chance to improve knowledge on this topic.
“The in-depth analysis of the FAME 3 trial suggests that the non-inferiority of FFR-guided PCI might instead emphasise the superiority of CABG for triplevessel coronary disease.”
Alessandro Parolari / University of Milano, Dept. of Universitary Cardiac Surgery, Policlinico San Donato IRCCS
Stroke after aortic arch surgery: results and risk factors from 2095 patients
G. Murana, Bologna, D. Levine, New York, NY, T. Hiroo, New York, P. A. Kurlansky, New York, Y. Ning, New York, A. Costantino, Bologna, L. Di Marco, Bologna, D. Pacini, Bologna. Giacomo Murana 1 MD, PhD


1 Division of Cardiac Surgery, IRCCS, Azienda Ospedaliero-Universitaria di Bologna, Alma Mater Studiorum – University of Bologna, Italy.
Despite the development of effective cerebral protection techniques, stroke is a major complication of aortic arch surgery, with a multi-centric analysis reporting a 5.7% and 3.3% incidence of focal permanent or transient neurological defects respectively1.
Open questions are that cerebral protection strategies are still vastly heterogenous among centres and endovascular techniques are gaining much popularity on proximal arch pathologies.
Our study aims to better understand the preoperative and intraoperative factors linked to stroke. It includes an exceptionally vast casuistry, combining the experience of two aortic centres: Bologna Alma Mater Studiorum (ITA) and the Columbia University (US). Population was 2095 patients who underwent aortic arch surgery over a 20-year-span, from 2000 to 2021.
The only preoperative characteristics significantly linked to post-operative stroke were diabetes, age and acute type-A dissection.
More surprisingly, stroke wasn’t associated with the site of arterial cannulation if antegrade cerebral perfusion was assured, but only to longer cardio-pulmonary bypass time and lower temperatures (DHCA vs ACP OR 2.79). Also, the extent of arch replacement, including the trunk procedure, wasn’t a risk factor and the addition of aortic root replacement was linked to lower stroke rates.
Stroke proved to be crucial, influencing both the short-term prognosis of the patients, associated with renal and respiratory failure, longer hospital stays and higher in-hospital mortality, as well as long-term prognosis. During our follow up, stroke was linked to lower one, five and ten-year survival with a 3.17 hazard ratio for late death.
As our data points out, the extension of the surgery both with ET and FET and aortic root substitution doesn’t lead to higher incidence of stroke given effective cerebral protection is achieved, therefore it should always be practiced when indicated.
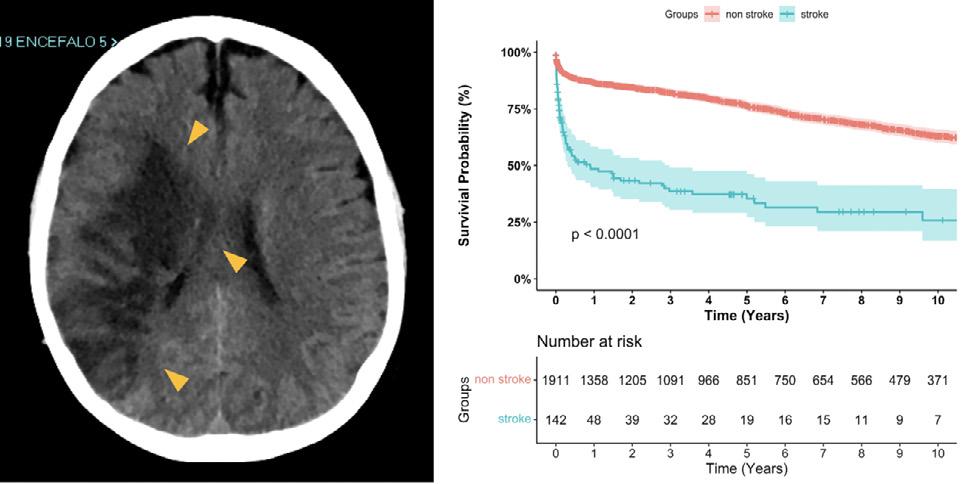
On the contrary, two main factors play a central role: patient selection and antegrade cerebral perfusion. First, oculate patient selection is key for clinical success, as highlighted by the most recent guidelines on aortic arch treatment 2 , which denounced the lack of specific clinical prediction models. Second, moderate hypothermia and selective cerebral perfusion proved to be superior to deep hypothermic circulatory arrest in preventing stroke and confirmed themselves to be the gold-
CARDIAC SURGERY INTERSOCIETY ALLIANCE
EACTS is proud to support the Cardiac Surgery Intersociety Alliance (CSIA) to promote the need for cardiac surgery for people living in low incomes countries. Too many people are dying unnecessarily in parts of Africa and elsewhere because they cannot access cardiac surgery services. Now in Mozambique and Rwanda, two pilots have been established which are in the early stages of bringing vital cardiac care to people in need. The CSIA is campaigning to ensure developing countries have cardiac surgery services that can be sustained for the long term. The CSIA is grateful to Artivion which has donated 50 heart valves to support this vital work. The CSIA is supported by EACTS, AATS, ASCVTS, STS and WHF.

Giacomo Murana / Division of Cardiac Surgery, IRCCS, Azienda OspedalieroUniversitaria di Bologna, Alma Mater Studiorum - University of Bologna, ItalyFigure 1: Survival probability of post-operative stroke after aortic arch surgery
Are

leaking aortic valves repairable?
 Ruggero De Paulis / Cardiac Surgery Dept. European Hospital, Unicamillus University, Rome, Italy
Ruggero De Paulis / Cardiac Surgery Dept. European Hospital, Unicamillus University, Rome, Italy

Auditorium
-
Leaflet prolapse and normal root in tricuspid aortic valve: is it worthy to repair?



It is certainly very much more frequent to encounter a prolapsing bicuspid aortic valve in a normal root configuration. This is the typical case of young men, frequently between the 20 and 30 years of age, where the conjoined cusp (more frequently in the R/L configuration) or both leaflets are widely prolapsing into the left ventricular outflow tract because of their intrinsic pathological anatomy associated with a progressive annular dilation. In these cases, the leaflet prolapses of one of both leaflets usually require an extensive plication, sometimes leaflet resection always associated with a robust annular reduction.
In the case of tricuspid aortic valve, the anatomical situation is completely different, the leaflet prolapse is usually more difficult to identify, and the amount of leaflet plication, when necessary, is much more limited.

What are the conditions where we are faced with an aortic valve insufficiency due to a prolapsing leaflet and a root of normal dimension? This condition is usually associated with an isolated dilatation of the sino-tubular (ST) junction, an isolated dilation of the annulus, or both together. When considering the aortic regurgitation frequently caused by an isolated dilatation of the ST junction, it is well known that a good symmetric remodeling of the ST junction can restore a good valve competence without the need for any additional maneuvers on the leaflets. However, in some instances the dilatation of the ST junction might asymmetrically alter the distance between the commissures causing a different stress on each leaflet. A leaflet overstretched for a long period of time might elongate and therefore prolapse once the ST junction is being reduced and remodelled. Alternatively, there are some instances where the aortic valve has leaflet of different sizes (with
the left most frequently being the smallest) and a symmetric ST junction dilatation will have different effects on each leaflet.
It is therefore of paramount importance to verify the good level of coaptation of the three leaflets immediately after ST junction remodeling to spot any leaflet prolapse that needs to be corrected.
To the same extent an isolated annular dilatation (infrequent in tricuspid aortic valve) might overstretch the leaflets and cause their prolapse.
Similarly, in the case of tricuspid valve, it is paramount to respect the correct ration between the diameter of the annulus and that of the ST junction.
The normal ratio annulus/St junction is usually 1:1.3.
In any case, spotting a residual prolapse in tricuspid valve can be more difficult if compared with bicuspid valves but its correction remains very important to avoid residual eccentric jets that will invariably negatively affect the long-term stability of the result. Eyeballing has been universally used for a long time, but a correct judgement is strictly dependent on the surgeon's experience and the chance of incorrect evaluation is always possible.
In the literature enough data are now available showing that a calibrated evaluation of the level of coaptation (effective height) and the amount of coaptation (coaptation length) improve the results and the surgeon satisfaction.
In conclusion, it is not only worthwhile but mandatory to repair a prolapsing leaflet in a tricuspid configuration. When there is more than one prolapsing leaflet the evaluation and the repair can be more difficult but still possible. Only lack of tissue needs be spotted and not confused for excessive tension on the free margin of the involved leaflet.
MOVING TOWARDS INTEGRITTY

Today’s focus session ‘Moving fast towards INTEGRITTY’ brings together members of INTEGRITTY (INTernational Evidence Grading Research Initiative towards Transparency and data qualiTY), a multidisciplinary group of cardiac surgeons and cardiologists with a keen interest in scientific transparency to support better and optimised patient management.
Through the INTEGRITTY project, the group aims to promote and provide unbiased, critical and unconflicted evidence in cardiovascular medicine to help healthcare professionals make the best choices for their patients. In compliance with the mission of academic institutions and scientific societies to pursue consistency of knowledge and evidence-based decision-making, the group’s experts work to appraise and evaluate evidence and provide an independent description and interpretation.
Victor Dayan, President of the Latin American Association of Cardiac and Endovascular Surgery (LACES) and group member, says, “Recent events have questioned the transparency and role conflicts of interest in the reliability of important trials. These issues are critical to all aspects of evidence generation, from its conception, execution, analysis and ultimately the development of guidelines. We believe an independent group of investigators and professionals is needed to contribute to the transparency and real benefit of therapeutic interventions.”
Today’s session will provide an overview of the INTEGRITTY project, set out why the group was established and provide an update on the group’s current activities, which include several streams of work such as conflicts of interest, valvular heart disease and coronary revascularisation. In each of these streams the group aims to dissect methodological inconsistencies in trials and generation of evidence through the development of registries and systemic reviews.
“Today’s session will provide an overview of the INTEGRITTY project, set out why the group was established and provide an update on the group’s current activities, which include several streams of work such as conflicts of interest, valvular heart disease and coronary revascularisation.”
Saturday 8 October
12:15 - 13:45

Moving fast towards INTEGRITTY
Amber 4
SCTS
Thoracic Movies
Amber 3
12:15 - 13:45
Anna Minasyan / Coruña University Hospital, Spain
Q. Where did you carry out your training?
Currently, I’m a fith year Thoracic Surgery Trainee at Coruña University Hospital, Spain.
Q. What are your main areas of interest within cardiothoracic surgery?
Minimally invasive thoracic surgery (VATS, Robotic surgery) and artificial intelligence in healthcare.

Q. What are your interests outside of your work?
I enjoy outdoor activities such as hiking. Also, I practice yoga and meditation. As a result of growing up in a family of surgeons and artists, I do enjoy charcoal drawing, origami, and writing novels.
Uniportal RATS left lower sleeve lobectomy


Introduction: With the introduction of robotic platforms in thoracic surgery, it was just a matter of time before the first complex lung resections and reconstructions using robotic systems were performed in high-volume centres. In this videocase report, we will present the technique on how to perform left lower sleeve lobectomy by Uniportal RATS.
Case presentation: A 59-year-old patient was admitted to our hospital with centrally located adenocarcinoma of the left lower lobe that involved the left main bronchus. No other comorbidities, except smoking history and obesity.
The technique: Uniportal RATS LLL sleeve surgery was performed. A 3cm incision is placed on the 7th intercostal space. The interlobar fissure is divided, and the artery is dissected. Then we proceed with the dissection of the inferior pulmonary ligament and the inferior pulmonary vein section. Arteries of the basal and 6th segments are dissected and sectioned. In the next step, the secondary bronchial carina is sectioned, then the left main bronchus and left superior bronchus resection margins are widened. Specimen (LLL) is extracted. A barbed suture is used to perform the anastomosis of the LSL bronchus to the left main bronchus. No postoperative complications are observed, and the patient is successfully discharged on the third postoperative day.
Conclusions: Uniportal RATS is a minimally invasive technique that can be used in sleeve
resections and reconstructions. However, these complex procedures must only be performed by surgeons experienced with robotic surgery and uniportal VATS technique.
Thoracic Movies
Giant hydatid cyst and destroyed lung
Hydatid cysts are the most common parasitic disease of the lungs. They are a major health problem in agricultural countries that lack satisfactory preventive medicine, environmental health and veterinarian services. Hydatid disease is endemic in the eastern and southeastern European regions. Due to the elasticity and compliance of the lung parenchyma, hydatid cysts typically grow faster in the lung than in other organs. Therefore, larger cysts are more common in the lung, where they can grow from a few millimetres to five centimetres in one year. Furthermore, cysts appear to grow faster in young people than in elderly people. Pulmonary cysts can enlarge substantially without symptoms; but, in general, symptoms depend on the size and location of the cyst, on the amount of pressure the cyst exerts on surrounding tissues, and on whether or not the cyst is ruptured. Hydatid cysts of 10 cm or greater in diameter are called “giant” cysts and traditionally have been considered to be more difficult to treat surgically – often requiring pulmonary resection.
We present a case of a giant cyst in the right hemithorax and the successful management in a 27-year-old man who presented with blunt chest pain. History was free and a thoracic ultrasound revealed a large, homogeneous fluid collection, most likely a cystic lesion while chest CT scan confirmed the diagnosis of a well- circumscribed, thick-walled, homogenous cyst, attached to the right visceral pleura, causing a left mediastinal shift. The patient underwent right anterolateral thoracotomy, the operative field was protected with compresses soaked in hypertonic (20%) sodium chloride solution and the cyst was aspirated.

Kalliopi Athanassiadi / “EVANGELISMOS”

General Hospital, Athens, Greece
Q. Where did you carry out your training?
• Athens – Greece
• Hamburg – Germany
• Montreal – Canada
Once the cyst's pressure decreased, two Allis forceps were clamped to hold the pericystic layer and the pericyst was opened and the endocysts were removed. Bronchial leaks were checked and unfortunately, the right upper lobe was destroyed, so a lobectomy was performed. The perioperative course was uneventful.

In conclusion, careful en bloc removal of the intact cyst, or removal after needle aspiration, using parenchyma-preserving techniques, is the treatment of choice. Adjuvant pre- and postoperative chemotherapy with benzimidazoles reduces the risk of dissemination and subsequent recurrence by inactivating protoscolices. Only in cases of destruction of lung parenchyma a lung resection should be performed.
Q. What are your main areas of interest within cardiothoracic surgery?
Lung surgery, tracheal surgery, chest wall reconstruction, trauma, thymic pathology and surgery, minimal invasive techniques.
Q. What are your interests outside of your work?
Music, dancing, languages & reading. I play the piano, speak seven languages and I like ballet and reading.
“Due to the elasticity and compliance of the lung parenchyma, hydatid cysts typically grow faster in the lung than in other organs.”
Enhanced recovery in Cardiac Surgery
Work Smarter, Not Harder: Remote Monitoring & Enhanced Recovery
Combining technologies to improve data management and analytics, digital and telehealth tools, and ERAS efforts provide a transformational, once-in-a-lifetime opportunity.
The "Perfect Care" (PC) programme has recognised this opportunity and engaged > 850 patients with enhanced, perioperative remote monitoring. PC includes a digital health kit and an application for scheduling, biometric data tracking, patient reported outcomes, messaging, and audiovisual visits.
PC's four-year, multi-institutional experience demonstrates feasibility, scalability, enthusiastic engagement of patients and clinicians, as well as transformative impact on outcomes. In fact, the PC results demonstrate significantly shorter length of stay, reduced 30-day mortality + readmissions, and the commensurate financial impact.
Enhanced Recovery in Cardiac Surgery
Kevin W. Lobdell / Sanger Heart & Vascular Institute, Atrium Health, US

Q. Where did you carry out your training?
• General Surgery-University of Minnesota (Minneapolis, MN USA)
• Cardiac Surgery Research-Yale University (New Haven, CT USA)
• Cardiothoracic Surgery-Yale University (New Haven, CT USA)
• Congenital Cardiac Surgery-Children’s Hospital of Philadelphia (Philadelphia, PA USA)
• Congenital Cardiac Surgery-Royal Children’s Hospital (Melbourne, AUS)
• Surgical Critical Care-Wayne State UniversityDetroit Medical Center (Detroit, MI USA)
Q. What are your main areas of interest within cardiothoracic surgery?
• Perioperative & Critical Care
• Digital Health & Technology
• Performance
Q. What are your interests outside of your work?
Golf, hockey, hunting, auto racing, military history, literature, music and photography.
Q. Where did you carry out your training?
I received my cardiac surgical training in Turkey, England, and the Netherlands and worked as a clinical fellow in Heinrich Heine University in Dusseldorf-Germany and the Heart Institute of Japan. I also studied histology and embryology for three years and completed PhD in Tissue Engineering and Biomaterial Science at Tokyo University.
Q. What are your main areas of interest within cardiothoracic surgery?
I am interested in minimally invasive cardiac surgery and direct international scientific projects on clinical evaluation and biomaterial confirmation of novel cardiopulmonary bypass-related technologies based on the prevention of inflammatory response. I also lead many national/international projects on patient blood management and ERAS.

Q. What are your interests outside of your work?
I am interested in theatre and acting. I am also a marathon runner.
Optimising an ERAS Patient Blood Management Program
Solidification of a Patient Blood Management Program Via Enhanced Recovery After Cardiac Surgery: Saving Millions Without Spending Billions

Enhanced recovery after surgery (ERAS) is a term encompassing a set of strategies and practices aimed at reducing the surgical stress response and optimising patient recovery through an evidencebased, multidisciplinary approach.
Standardised multidisciplinary processes contain 22-actions including mainly preoperative patient education, carbohydrate loading, anemia treatment, multimodal opioid-sparing analgesia, goal-directed fluid/perfusion and a rigorous bowel regimen. Initial large-scale studies based on systematic application of ERACS principles with reduced opioid use and length of stay and improved patient and staff satisfaction.
The central tenet of patient blood management (PBM) is the use of every appropriate measure to protect and manage a patient’s own blood, in a manner that is tailored to the needs of the individual patient. It addresses the problems of anemia, blood loss and coagulopathy. It is a patientcentered, systematic, evidence-based approach to improve patient outcomes by managing a patient’s own blood through diagnosis and etiology-specific treatment of anemia and preserving the patient’s own blood by minimising blood loss and bleeding, while promoting patient safety and empowerment.
It reduces the utilisation of health care resources as well as expenditures, transfusion dependency, and the risks and complications of transfusion.
The Ankara City Hospital is the largest hospital in Turkey. The previous practice with the use of more than 100,000 units of blood and blood products in one year necessitated the need for a PBM programme. We have implemented the ERACS programme focusing on PBM and managed up to 30% decrease with excellent clinical results within three years.
Although ERACS is relatively new to cardiac surgery, these programmes can benefit from guidelines as they develop protocols to decrease unnecessary variation and improve quality, safety, and value for their patients. Patient and caregiver education and systemwide engagement are necessary to implement best practices. The cardiac surgical team is under increasing pressure to reduce complications and costs while providing the best-possible patient experience. A welldesigned and implemented ERACS program can assist in achieving the goals.
1.
2.
Prof Serdar Gunaydin / Department of Cardiovascular Surgery University of Health Sciences, Ankara City Hospital Campus, TurkeyFigure 1: ERAS/PBM protocol (minimally invasive surgery, minimally invasive circuitry, nutritional components and Ankara City Hospital
Thoracic Oncology
Patients and Methods: This prospective trial started in 2003. Patients with a tumor 2 cm or smaller in maximum dimension and tumor disappearance ratio (TDR) 0.5 or greater, diagnosed or suspected as a clinical T1N0M0 (UICC-TNM 6th edition) carcinoma in the lung periphery based on thin-slice CT were enrolled. Clinical and pathological stages of all tumors were reclassified according to the 8th edition.
lung cancer may require a long-term follow-up of 10 years instead of five years.
Q. Where did you carry out your training?
Yokohama City University, The Cancer Institute Hospital, Japan.
Q. What are your main areas of interest within cardiothoracic surgery?
Lung cancer, minimally invasive thoracic surgery.
Q. What are your interests outside of your work?
My family.
Background: Previous study in our institute suggested all eligible <20 mm GGO tumors might have been radically managed with only limited resection (Yoshida J, et al. JTCVS 2005). The purpose of our trial is to validate limited resection for ragiological less invasive lung cancer.
Results: In total, 100 patients were enrolled. The median follow-up period was 10.1 years. The five year and 10-year RFS were 99.0% and 96.1%. The five year and 10-year OS were 99.0% and 96.1%. Two patients of cut end recurrence after wedge resection were observed. A 51-year-old man underwent wedge resection (pStage IA2 adenocarcinoma). A nodule near the staple line gradually enlarged (Figure 1), and a biopsy was performed to obtain a diagnosis of adenocarcinoma. Ten years after initial surgery, completion right lower lobectomy was performed. A 66-year-old woman underwent wedge resection (pStage IA2 adenocarcinoma). A nodule near the staple line gradually enlarged (Figure 2), and a biopsy was performed to obtain a diagnosis of adenocarcinoma 11 years after initial surgery. Since bone metastases were identified at the same time, administration of osimertinib was started.
Conclusion: Limited resection provided a satisfactory prognosis for patients with ragiological less invasive lung cancer. On the other hand, after a long-term follow-up of 10 years, two patients had cut end recurrence after wedge resection. A sufficient surgical margin is mandatory for limited resection. Also, early-stage

Thoracic Oncology
Brown 1 12:15 -
Tomohiro Miyoshi / Division of Thoracic Surgery, National Cancer Center Hospital East, Japan


Q. Where did you carry out your training?
A general surgery residency program of Mitsui Memorial Hospital, Tokyo, Japan.
Q. What are your main areas of interest within cardiothoracic surgery?
Thoracic oncology.
Q. What are your interests outside of your work?
Cancer treatment in developing countries.
Risk Factors of Loss of Pulmonary Function after Wedge Resection for Peripheral Groundglass Opacity (GGO) Dominant Lung Cancer: Secondary Analysis of a Single-arm Study Tomohiro Miyoshi, Hiroyuki Ito, Kenji Suzuki, Tomoko Kataoka, Masashi Wakabayashi, Ichiro Yoshino, Masahiro Tsuboi, Shun-Ichi Watanabe


Background: The Japan Clinical Oncology Group (JCOG) – Lung Cancer Surgical Study Group has defined nodules of ≤2 cm and a C/T ratio (consolidation/tumor ratio) of ≤0.25 as radiologically non-invasive cancers. Subsequently, JCOG0804/WJOG4507L, a single-
arm confirmatory phase III study to evaluate surgical resection for radiologically non-invasive cancers, concluded that partial or segmental resection was the first-choice treatment for them. In JCOG0804/WJOG4507L, the median change in FEV1.0 before and after surgery was -5%, but the range was widely distributed from -37% to +49%. We aimed to investigate the risk factors of respiratory functional deterioration after wedge resection as a secondary analysis of JCOG0804/ WJOG4507L.
Patients and Methods: In JCOG0804/ WJOG4507L, a total of 314 patients from 51 institutions between May 2009 and April 2011 underwent sublober resection. We excluded 56 patients who underwent segmentectomy and 21 patients with data missing of respiratory function, and the analysis population is the remaining 237 patients with both preoperative and one year postoperative FEV1.0 data. We calculated the change of respiratory function in a year as follows; (postoperative FEV1.0 – preoperative FEV1.0)/ preoperative FEV1.0. We divided the patients into two groups with the cutoff value of -0.1 in perioperative FEV1.0 change (<= -0.1, severely reduced group; > -0.1, normal group). We compared the background of the two groups and conducted logistic regression analysis to identify risk factors. We investigated the correlation between postoperative adverse events (>=Grade 2, CTCAE) and pulmonary function.

Results: Thirty-seven patients (16%) severely reduced FEV1.0 in a year. In the multivariable analysis, pleural indentation was an independent predictive factor of post-operative pulmonary functional deterioration (OR 2.67; 95% CI 1.08–6.55; p=0·031). Smoking and total tumor size (>= 1 cm) were marginally significant (OR 1.90; 95% CI 0.90–4.01; p=0·093, and OR 2.95; 95% CI 0.99–8.81; p=0·053, respectively). Post-operative
complications including lung-related ones did not differ between patients with and without reducing of FEV1.0.
Conclusion: Sixteen percent of the fit patients with wedge resection for early-stage lung cancer suffered >10% reduction of FEV1.0 in a year, which reduction was equivalent to lobectomy.
Chronological







Joji Samejima / Division of Thoracic Surgery, National Cancer Center Hospital East , Kashiwa, Japan
Thoracic Oncology
VATS Anatomical Segmentectomy versus Lobectomy in Stage IA Non-Small Cell Lung Cancer: A Systematic Review and Meta-Analysis
Luca Bertolaccini, MD PhD FCCP1, Elena Prisciandaro, MD1, Claudia Bardoni, MD1, Andrea Cara, MD, Lara Girelli, MD PhD1, Lorenzo Spaggiari MD PhD1,2
1. Department of Thoracic Surgery, IEO, European Institute of Oncology IRCCS, Milan, Italy.


2. Department of Oncology and Hemato-Oncology, University of Milan, Milan, Italy.
Background: The Japanese randomised control trial JCOG0802/ WJOG4607L was the first phase 3 study to show the benefits of segmentectomy versus lobectomy on patient overall survival (OS), suggesting that segmentectomy should become the standard surgical treatment for early-stage non-small cell lung cancer (NSCLC). Nonetheless, various controversies still exist regarding the extent of curative lung resection. A systematic review and meta-analysis was performed to determine differences in disease-free survival (DFS), OS, and perioperative outcomes in patients with stage IA NSCLC treated with Video-Assisted Thoracic Surgery (VATS) anatomical segmentectomy or lobectomy.
Methods: This systematic review and meta-analysis was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRIMA) guideline. A systematic search of EMBASE (through Ovid), MEDLINE (via PubMed), and Cochrane CENTRAL was conducted. Two researchers independently reviewed each eligible study that included patients with stage IA NSCLC treated with minimally invasive anatomical segmentectomy and lobectomy and compared the perioperative and/or survival outcomes of patients.
Results: A total of 887 publications were identified. Of these, 13 articles met our eligibility criteria (Figure 1). The mean difference in the number of harvested lymph nodes was statistically significantly lower in the VATS segmentectomy group. Postoperative complication rate, DFS (Figure 2) and OS (Figure 3) were not significantly different between the two groups. Postoperative hospital stay was shorter for the patients who underwent minimally invasive segmentectomy.
Conclusions: Minimally invasive lobectomy and segmentectomy showed comparable short-term and long-term outcomes for treating stage I NSCLC. Postoperative complication rates were similar. Minimally invasive segmentectomies are associated with a higher number of harvested lymph nodes and a shorter length of hospital stay. Extensive randomised clinical studies with accurate pulmonary function, detailed stage data on complications, and long-term surgical follow-up are required.
NEW EACTS GROUP HOSTS NURSES AND ALLIED HEALTH SESSIONS
Cardiac surgery requires a multidisciplinary team effort to improve outcomes for patients. Nurses and allied health professionals play a vital role providing critical preand post-operative care, ensuring patients have the best possible chance of recovery after surgery.
The Nurses and Allied Health Group has been established to create a platform for high quality research and collaboration by nurses and other healthcare professionals in cardiac surgery. As Dr Richard Van Valen, a Nurse Practitioner and Researcher at Erasmus MC and Chair of the Group explains, “Our group is conducting vital research that, although is not always directly surgical related, provides an important contribution to ensuring patients have a high quality and safe pathway before and after cardiac surgery. Nurses are working very hard, not just on the wards, but also on developing scientific output.” The group is also keen to support the development of preand post-operative guidelines.
The Nurses and Allied Health Group has organised two important focus sessions at this year’s Annual Meeting. The first session ‘Improving patient care and pathways ’, taking place today at 08.30, highlights the critical work of nurses and others who work in the field of cardiac surgery. Featuring high quality abstract submissions, the session will explore mental health and wellbeing post-COVID, a nurse-led quality improvement project for the prevention of cardiac surgery complications and dietary intervention to reduce Metabolic Syndrome risk in heart transplanted patients.
Virtual reality training tool to improve CPR techniques
The role of technology to support training in CPR after cardiac surgery is explored in today’s second session at 10.30 organised by the Nurses and Allied Health Group. ‘Training for the Worst; Using Virtual Reality a Training Tool for ALS after


Cardiac Surgery ’ showcases the use of virtual reality to teach and train residents and nurse practitioners on critical procedures such as CPR after cardiac surgery, which require a completely different protocol.


Chair of this session, Dr Edris Mahtab, a cardiothoracic surgeon at Erasmus MC, who has been involved in the development of this VR technology, says, “Simulators are essential for healthcare professionals who are doing this type of procedure with patients every day. These procedures require good communication and a good understanding of the algorithm. Training with virtual reality helps teach the different steps. This means that nurses and residents, for example, can take action much faster and will feel less stressed when resuscitating a patient. Time is critical when undertaking CPR after cardiac surgery, so this technology has huge potential to improve patient safety.”
The results of randomised controlled trials in the Netherlands have been very positive. Eighty-five per cent of users of the virtual reality simulator say they are very happy for the simulator to be applied in regular training.
CPR training can be expensive and timeconsuming, with a minimum group of six people required for the training. Training in virtual reality means people don’t need to come together in one place. The whole algorithm can be learnt by one individual.
A smart portfolio system has also been developed to help evaluate the trainee during training with the virtual reality simulator.
Participants in this session will have an opportunity to get hands-on with the virtual reality technology and experience training with the simulator.
Saturday
October
patient care and pathways
Training for the Worst; Using Virtual Reality a Training Tool for ALS after Cardiac Surgery





3-D Matrix A04
Abbott B12
ABIOMED B10
Advancis Surgical C06
American Association for Thoracic Surgery (AATS) A30
AMT Medical B.V. C32
Andocor NV B24
AngioDynamics A16
Artivion EMEA GmbH B14
Artivion EMEA GmbH - Learning Lab C03a
Asanus Medizintechnik GmbH C13
AtriCure Europe B.V. B16
AtriCure Europe B.V. - Learning Lab B02
BD Interventional - Becton Dickinson A09 & A11
BioCer Entwicklungs-GmbH C18
Bio Sud Medical Systems Srl A03bis
Cardia Innovation AB A23
Cardio Medical GmbH C20
CARL. B20
CARMAT A10
Chalice Medical Ltd B26
Cook Medical Europe LTD B07
Corcym S.r.l. B08
CTSNet.org A28
CUI INTERNATIONAL LIMTED A06
CytoSorbents Europe GmbH B21 & B23 & B25
Delacroix-Chevalier C22&C24
Dendrite Clinical Systems Ltd A25
Dr. Franz Koehler Chemie GmbH C15 & C28
EACTS - The European Association For Cardio-Thoracic Surgery C13
EACTS - Learning Lab C01
EACTS - TV Studio A17
Edwards Lifesciences C09
EpiHeart Oy C34
Eurosets s.r.l. C07
Exstent Limited B31
Fehling Instruments GmbH & Co KG C21 & C23
FIAB Spa B27 & B29
Foldax, Inc. A21
GEISTER Medizintechnik GmbH B06
Genesee BioMedical Inc A15
HAART- Aortic Valve Repair Technologies by BioStable Science & Engineering C17 Hemonart Medikal Sistemler Sanayi Ticaret A.S. A12
ISMICS/HVS (International Society for Minimally Invasive Cardiothoracic Surgery & Heart Valve Society) A01 & A03
Jafron Biomedical Co., Ltd. A07BIS Jarvik Heart Inc C19
Johnson & Johnson Medical Devices Companies A14 Kapp Surgical Instrument, Inc. A05bis
KLS Martin Group A08 & B09 LifeTec Group A19 LSI Solutions A18 & A20 Medela AG B05 Medistim ASA B04
Medtronic International Trading SÁRL C05 Medtronic International Trading SÁRL - Learning Lab C03 Meril Endo Surgery Pvt Ltd C02 & C04
NEOS SURGERY C30
Osypka AG B03
Oxford University Press B33
Peters Surgical B04a PHOENIX s.r.l. B11
POSTHORAX ltd. B01 Qualiteam s.r.l. B19
REDAX Spa B15 & B17
Scanlan International, Inc C08 & C10 & C12 & C14
STS-The Society Of Thoracic Surgeons A27 Sunoptic Technologies A02
Terumo Aortic & Terumo Europe N.V. B18
Thompson Surgical Instruments, Inc.
tisgenx, Inc.
Transonic Systems, Inc. A05&A07
Conduits are key to CABG success: a video masterclass

Amber 1 & 2
14:00 - 15:30
Harvesting the RA open
In 2018, ESC/EACTS guidelines on myocardial revascularisation the radial artery (RA) is a class I indication as the second preferred conduit in coronary artery graft bypass (CABG). Long-term results showed higher patency rates when compared with other conduits. Key points for its use are patient selection and a meticulous harvesting technique.
We avoid RA in patients with vasculitis, prior surgery/trauma and advanced renal failure with a potential need to arteriovenous fistula.
The first step is to have palpable radial and ulnar pulses and a negative modified Allen test. Ultrasound can confirm correct RA diameter (≥2.0 mm) and absence of calcification. We prefer the non-dominant RA with no prior catheterisation. In selected cases we consider RA after three months from transradial access.
We use a curvilinear incision from 1 cm proximal to the wrist to 2 cm distal to the elbow, following the brachioradialis muscle. We divide superficial tissues with electrocautery, preserving superficial veins when possible. We open the brachioradialis and the flexor carpi radialis fascia and expose the RA with a retractor. We harvest the RA as a pedicle. Without directly touching the artery we dissect all the collateral branches with a Metzenbaum scissor, clipping and dividing them. We extend the dissection to the lateral antebrachial cutaneous nerve and the recurrent radial artery, that we preserve. Distally we extend the dissection proximal to the superficial palmar artery. The RA ends are then tied, clipped and divided with 15 blade.
“We use a curvilinear incision from 1 cm proximal to the wrist to 2 cm distal to the elbow, following the brachioradialis muscle.”
Due to potential spasm, we use papaverine at 3mg/mL in a saline warm bath before and after harvesting the RA. While the proximal end is open with Potts scissor we flush the RA with warm saline solution and periadventitially with papaverine. We then store it in the warm papaverine solution.
Valentina Mescola / Navarra University Hospital , Spain
Q. Where did you carry out your training?
In 2012 I became an intern student in the Cardiac Surgery department in Padua, and in 2013 I graduated in Medicine and Surgery from the University of Padua, Italy, Magna Cum Laude, with a thesis about the use of ECMO in primary cardiogenic shock.
After the degree I decided to move to Spain to pursue the residency in Cardiovascular Surgery at Sant Pau Hospital, in Barcelona, one of the principal hospitals of the second most populated area of the country, with more than 650 major surgeries per year.
After the residency program I moved to Pamplona, where I’m currently working.
Q. What are your main areas of interest within cardiothoracic surgery?
During my training I renewed and expanded my interest in the treatment of advanced heart failure with mechanical circulatory support, aortic valve and root surgery and total arterial revascularization. I had the chance to learn up close from experts in the off-pump technique, in addition to the conventional on-pump setting, and to become familiar with the routine use of the readial artery as the second preferred conduit.
Q. What are your interests outside of your work?
In my spare time I’m an experienced scuba diver and I love to explore life under the sea. I'm also a passionate reader and a huge lover of food, as a customer and as a cook.
The forearm is closed after a meticulous hemostasis. We leave the fascia open and close in layers with 2/0 absorbable suture. We do not routinely leave a drain. The skin is closed with 3/0 monofilament absorbable running suture. A mild compressive bandage is placed. Low dose Calcium blockers are indicated during the first postoperative year when not contraindicated.


Q. Where did you carry out your training?
I studied a joint degree in Technical Medicine at the Technical University of Delft, Erasmus MC, Rotterdam, and Leiden University Medical Center.

Q. What are your main areas of interest within cardiothoracic surgery?


Surgical planning and navigation, ex-vivo lung perfusion, lung/oncologic surgery, lung and heart transplantation, and congenital surgery.




Q. What are your interests outside of your work?
I enjoy playing sports, such as road cycling, tennis, and volleyball. I also like cooking dinners with friends.
Optimised preoperative planning of double outlet right ventricle patients by 3D printing and virtual reality: a pilot study
Objectives: In complex double outlet right ventricle (DORV) patients, the optimal surgical approach may be difficult to assess based on conventional two-dimensional (2D) ultrasound (US) and computed tomography (CT) imaging. The aim of this study is to assess the added value of 3D printed and 3D Virtual Reality (VR) models of the heart used for surgical planning in DORV patients, supplementary to the gold standard 2D imaging modalities.
Methods: Five patients with different DORVsubtypes and high-quality CT scans were selected retrospectively. 3D prints and 3D-VR models were created. Twelve congenital cardiac surgeons and pediatric cardiologists, from three different hospitals, were shown 2D-CT first, after which they assessed the 3D print and 3D-VR models in random order. After each imaging method, a questionnaire was filled in on the visibility of essential structures and the surgical plan.
Results: Spatial relationships were generally better visualised using 3D methods (3D printing/3DVR) than in 2D. The feasibility of VSD patch closure could be determined best using 3D-VR reconstructions (3D-VR 92%, 3D print 66%, and US/CT 46%, P<.01). The percentage of proposed surgical plans corresponding to the performed surgical approach was 72% for plans based on US/ CT, 85% for plans based on 3D printing, and 87% for plans based on 3D-VR visualisation.
Conclusions: This study shows that both 3D printing and 3D-VR have additional value for cardiac surgeons and cardiologists over 2D imaging, because of better visualisation of spatial relationships. As a result, the proposed surgical plans based on the 3D visualisations matched the actual performed surgery to a greater extent.
“In complex double outlet right ventricle (DORV) patients, the optimal surgical approach may be difficult to assess based on conventional two-dimensional (2D) ultrasound (US) and computed tomography (CT) imaging.”
EACTS MEMBERSHIP
EACTS MEMBERSHIP
The EACTS global community continues to grow. This year we are delighted to welcome 285 new members. Their applications were approved at yesterday’s General Assembly.
Why become an EACTS member?
EACTS membership is available for residents, active surgeons, allied health members, industry representatives and the cardiothoracic community from low-income countries. And there is even a category for retired members.
All members have an exciting opportunity to play a key role in EACTS and our ongoing commitment to raising standards and improving outcomes for patients in the field of cardiac, thoracic and vascular interventions.
The EACTS Council is the governing, decision-making body of EACTS. Each Councillor serves a set term. Any EACTS member can nominate a fellow member for a specified role on Council.
Our Domains and Committees are member led groups working across the four EACTS Domains - Acquired Cardiac, Congenital Heart, Thoracic and Vascular. These committees play an instrumental role across a range of projects and meetings, from clinical guidelines and quality improvement to women in cardiothoracic surgery and education.
There are many other compelling reasons to join EACTS, including unrivalled access to a range of education, content and networking opportunities.
HIGH QUALITY EDUCATION
EACTS Academy
The EACTS Academy offers a superb programme of courses to suit your level of experience, whether you are an experienced surgeon or still in training. Our courses are well attended, helping you improve outcomes for patients and supporting your career progression.
Francis Fontan Fund
The prestigious Francis Fontan Fund for Education offers an exciting opportunity to advance surgical education, foster professional development and learn from the highest standards of cardiothoracic care at some of the most prestigious institutions around the world. The Fund is open to EACTS members from all countries and currently supports several different Fellowship schemes specialising in a breadth of cardiothoracic techniques.
IMPROVING CLINICAL OUTCOMES
Clinical Guidelines
EACTS works alongside sister organisations and partners to develop high quality clinical guidelines on specific procedures and techniques. Our committees take a whole heart team approach, assessing the very latest clinical data and evidence to prepare clear clinical guidelines that support clinicians in their constant drive to improve outcomes for patients.
Quality Improvement Programme (QUIP)
EACTS has also established a Quality Improvement Programme (QUIP) to encourage the improvement of clinical outcomes for patients and to promote the importance of integrating quality improvement initiatives into daily clinical practice.
EACTS Quality Improvement Programme includes two international databases - the Adult Cardiac Database (ACD) and EUROMACS – the European Registry for Patients with Mechanical Circulatory Support.
PROMOTING RESEARCH AND INNOVATION
EACTS Journals
The EACTS publications portfolio includes two leading, high-quality online journals, publishing the latest research across the field of cardiac, thoracic and vascular interventions.
• Subscription based European Journal of Cardio-Thoracic Surgery (EJCTS) publishes original scientific reports documenting significant clinical and experimental advances relating to surgery of the heart, the great vessels and the chest.
• Interactive CardioVascular and Thoracic Surgery (ICVTS) is an openaccess journal publishing scientific contributions in the field of cardiac, vascular, and thoracic surgery. In 2023 ICVTS changes to Interdisciplinary CardioVascular and Thoracic Surgery
Submissions are subject to rigorous peer-review by members of the journals’ Editorial and Advisory Board and by other independent reviewers. Both journals have growing Impact Factors and are indexed in Pubmed.
In addition, EACTS publishes The Multimedia Manual of Cardio-Thoracic Surgery (MMCTS), the premier online video manual for cardiac, vascular, and thoracic surgical procedures. It features step-by-step narrated videos demonstrating how to perform a comprehensive range of different surgeries. Each video tutorial is accompanied by detailed how-to descriptive text, and illustrations where relevant.
Shaping the future of cardiothoracic surgery
EACTS Residents Committee is devoted to representing the views and interests of cardiothoracic surgery residents and helping to facilitate education and identify training needs. The committee organises EACTS educational events, including the resident activities at the EACTS Annual Meeting and works with the EACTS Education Committee to assist in developing educational curriculums.
It is important to ensure the voice of Resident surgeons is heard and has an impact on all aspects of our governance and practice.
EACTS Annual Meeting
And of course, there is our flagship event, the Annual Meeting. The EACTS Annual Meeting is THE event in the cardiothoracic calendar. Every year colleagues from around the world come together to experience world-class education and science. The meeting provides a myriad of opportunities to network with peers and colleagues from around the world.
NEW EACTS MEMBERS 2022
Bledar Hodo Albania
Artan Jahollari Albania
Anurag Agarwal Australia
Asen Ivanov Australia
Justin Ren Australia
Misté RongHui Chia Australia
Vignesh Ratnaraj Australia
Michael Zhu Australia
Fabian Seeber Austria
Stephan Holzinger Austria
Sepideh Mostofi Austria
Frieda-Maria Kainz Austria
Felix Nägele Austria
Paimann Nawrozi Austria
Natig Mirzayev Azerbaijan
Saikat Dasgupta Bangladesh
Md Kamrul Hasan Bangladesh
Sultan Parvez Bangladesh
Alena Kurlianskaya Belarus
Youry Ostrovsky Belarus
Liana Shestakova Belarus
Samuel Bruls Belgium
Quentin Desiron Belgium
Marc Detroux Belgium
Loren Packlé Belgium
Ivan Eltsov Belgium
Joeri Van Puyvelde Belgium
Germano Dan Brazil
Andre Lupp Brazil
Ralf Stuermer Brazil
Osami Honjo Canada
Alla Alghamedi Canada
Fadi Hage Canada
Alex Nantsios Canada
Junichi Shimamura Canada
Roxanne St-Louis Canada
Keerit Tauh Canada
Vishnu Vasanthan Canada
Pablo Salazar Chile Wei Huang China
Qiang Zhao China
Lorena Montes Colombia
Hector Olaya Colombia
Filip Štembal Croatia
Tomislav Tokic Croatia
Andreas Paschalis Cyprus
Peter Ivák Czech Republic
Petr Kacer Czech Republic
Vitalii Rizov Czech Republic
Petr Smolák Czech Republic
Lin Huang Denmark
Louise Rasmussen Denmark
Lissette Mota Dominican Republic
Daylen Marti Perez Ecuador
Carlos Emilio Bernal Rodriguez Ecuador
Mohammed Abdellatif Egypt
Jari Räsänen Finland
Henri Haapanen Finland
Tommi Järvinen Finland
Nelli Nurminen Finland
Jean Porterie France
Charlotte Bouaziz France
Mohammed Alghamdi France
Lasha Basiladze Georgia
Kakhaber Latsuzbaia Georgia Robert Balan Germany Nicolai Bayer Germany
Stephane Collaud Germany Mahmoud Diab Germany
Volker Düsterhöft Germany Joerg Ender Germany Anna Flo Forner Germany Kambiz Hassan Germany Jamila Kremer Germany Mohamed Quader Germany Bassam Redwan Germany
Diyar Saeed Germany Carolyn Weber Germany Eyad Al Masri Germany Florian Bölke Germany Ralph Götz Germany
Michael Voigtlaender Germany Karen Abeln Germany Tim Berger Germany Martin Beyer Germany Ramon Chaila Germany Agunda Chekhoeva Germany Juan De Glee Romera Germany Tomasz Dziodzio Germany Ibrahim Gadelkarim Germany Chirstopher Gaisendrees Germany Jagdip Kang Germany
Eslam Mohamed Germany Roya Ostovar Germany
Jawad Salman Germany Guillermo Stöger Germany
Zulfugar Taghiyev Germany Konstantinos Archontis Tselonis Germany Sam Varghese Germany
Katharina Wehrmann Germany
Nikolaos Schizas Greece
Crystallia Batsis Greece
José Miguel Arriola Navas Guatemala
Gábor Bari Hungary
Devender Singh India
Varuna Varma India
Navy Laksmono Indonesia
Widya Suwatri Indonesia
Saoud Al-Neaimy Iraq
Jack Whooley Ireland
Reut Shavit Israel
Guido Baietto Italy
Michele Celiento Italy
Giovanni Alfonso Chiariello Italy
Giovanni Comacchio Italy
Gabriele Di Giammarco Italy
Antonella Galeone Italy
Tommaso Hinna Danesi Italy
Marco Mammana Italy
Salvatore Scianna Italy
Petar Soso Italy
Vasileios Tsiopoulos Italy
Vladimiro Vida Italy
Annalisa Bernabei Italy
Nunzio De Manna Italy
Antonio D'Errico Ramirez Italy
Alessandra Francica Italy
Marco Gemelli Italy
Lorenzo Longinotti Italy
Matteo Petroncini Italy
Federico Soma Italy
Kosuke Fujii Japan
Hiroki Hata Japan
Yochun Jung Korea, South
Taeyeon Lee Korea, South
Dainius Karciauskas Lithuania
Gediminas Kitra Lithuania
Sashko Jovev Macedonia
Vasil Papestiev Macedonia
Adli Azam Mohammad Razi Malaysia
Muhammad Ibrahim Azmi Malaysia
Benigno Ferreira Mexico
Frida Rivera Mexico
Elmehdi Maidi Morocco
Win Win Kyaw Myanmar (Burma)
Kadir Caliskan Netherlands
Riccardo Cocchieri Netherlands
Kevin Damman Netherlands
Meike Haverkamp Netherlands
Wouter Markus Netherlands
Wouter Bakhuis Netherlands
Emile Farag Netherlands
Nimrat Grewal Netherlands
Romy Hegeman Netherlands
Selma Kaffka Genaamd Dengler Netherlands
Sohrab Khadjeh Netherlands
Coert Kok Netherlands
Jules Olsthoorn Netherlands
Herman Tolboom Netherlands
Emma Van Der Weijde Netherlands
Maurits Zegel Netherlands
Raul Correia New Zealand
Per Lingaas Norway
Aiman Tariq Pakistan
Firas Abu Akar Palestinian Territory, occupied
Luis Zavaleta Peru Pedro Rojas Sanchez Peru
Aldrix Josue Sisniegas Razón Peru Cristian Yepez Calderon Peru
Justyna MalyszekTumidajewicz Poland Anna Kedziora Poland
Maciej Suchnicki Poland
Catarina Novo Portugal
Laith Tbishat Qatar
Roxana Geana Romania Nayyerani Reza Romania
Vagram Balanyan Russian Federation Dmitry Khvan Russian Federation
Abdulelah Alamri Saudi Arabia
Azzahra Edrees Saudi Arabia
Stevan Čičić Serbia and Montenegro
Matija Jelenc Slovenia Tomaž Štupnik Slovenia Miguel Piñón Spain
Facundo Machado Fernández Spain
Carlos Martin Spain
Lourdes Montero Cruces Spain Anna Minasyan Spain
Alexander Morales Linares Spain Iddagoda
Hewage Don Saman Pradeep Sri Lanka
Peter Svenarud Sweden
Ida Axelsson Sweden
Sigurthor Halldorsson Sweden
Philine Isabel Fleckenstein Switzerland
Diana Sandra Reser Switzerland
Nikola Cesarovic Switzerland
Thorald Stolte Switzerland
Birgit Mueller Switzerland
Lilly Ilcheva Switzerland
Alecsandra Tudor Switzerland
Pisanuwach Charoenpachara porn Thailand
Angsu Chartrungsan Thailand Sopita Comerungsee Thailand
Jenvit Jangjit Thailand Siam Khajarern Thailand Chanapong Kittayarak Thailand Kornkan Mahasawas Thailand Ekarat Nitiyarom Thailand
Phassakorn Noiniyom Thailand Amarit Phothikun Thailand Pramote Porapakkham Thailand Phuripong Rodneam Thailand Sasitorn Sakkarat Thailand
Yuttasint Vongsangcom Thailand Sitichok Wachirasrisirikul Thailand Surin Woragidpoonpol Thailand Cemal Kutlu Turkey Kamile Ozeren-Topcu Turkey Pinar Tezer Turkey Ahmet Can Topçu Turkey Recep Caliskan Turkey Halit Er Turkey


Safa Ozcelik Turkey Ivan Budzan Ukraine Kostiantyn Chyzh Ukraine
Volodymyr Gutovskiy Ukraine Mykhailo Ishchenko Ukraine
Hanna Koltunova Ukraine Dmytro Kosovan Ukraine Oleksandr Kulbachnyi Ukraine Oleksandr Luchynets Ukraine Oleksandr Senko Ukraine Barno Sobirov Ukraine Mariia Tregubova Ukraine Viktoriia Tymoshenko Ukraine Yurii Vitkovskyi Ukraine
Viacheslav Zinchenko Ukraine Viktor Tytiuk Ukraine Tarek Alameddine United Kingdom
Faraz Baig United Kingdom Fabio De Robertis United Kingdom
Simon Duggan United Kingdom Mikel Kamami United Kingdom
Jacie Jiaqi Law United Kingdom
Mahmoud Loubani United Kingdom
Paul Modi United Kingdom
Eltayeb Mohamed Ahmed United Kingdom
Alessandro Montecalvo United Kingdom
Alessia Rossi United Kingdom
Luigi Ventura United Kingdom
Una Maria Ahearn United Kingdom
Rishab Makam United Kingdom
Ahmed Mandisha United Kingdom
Mauro Cosimetti United Kingdom
James Veitch United Kingdom
Ian Cummings United Kingdom
Francesca Gatta United Kingdom
Arthika Surendran United Kingdom
Shagorika Talukder United Kingdom
Charlene Tennyson United Kingdom
Myat Soe Thet United Kingdom
Sara Ugolini United Kingdom
Alex Visan United Kingdom
Samuel Pollock United States
Frank Baciewicz United States
Nakai Chikashi United States
William Deschner United States
John Hance United States
Melissa Levack United States
Ioannis Loumiotis United States
Michael Mitchell United States
Steve Motes United States
Syed Peer United States
Mahesh Ramchandani United States


Elyan Ruiz Solano United States
Randall Wolf United States
Deborah Adams United States
Salah Eldien Altarabsheh United States
Martin Martinez United States
Jennifer Perri United States
Benjamin Shou United States
Maximiliano Hernandez Uruguay
Nodir Ibragimov Uzbekistan
Kambarali Khaydarov Uzbekistan
Bobur Turaev Uzbekistan
ANNULOPLASTY FOR AORTIC VALVE REPAIR: A PRACTICAL APPROACH

An EACTS technical course on aortic valve repair; March 22-24, 2023, Paris, France
 Emmanuel Lansac / Course Director; La Pitié Salpétrière
Emmanuel Lansac / Course Director; La Pitié Salpétrière

This Level 3 EACTS course offers attendees a deep dive into a standardised and reproducible approach to aortic valve repair. This will include the rationale, physiological sizing and insertion techniques for incorporating an external aortic annuloplasty ring as part of any repair procedure.
The course will provide in-depth training of aortic valve repair from valve-sparing root replacement (for root aneurysms) to isolated aortic valve repair (for isolated aortic insufficiency) (fig 1). Repair techniques for tricuspid, bicuspid and unicuspid valves will be covered in step-by-step detail. A combination of technical lectures combined with four full live surgeries and further pre-recorded live-in-a-box video sessions on different lesion sets will teach attendees how to repair different valve morphologies and aortic phenotypes. Further lectures on echocardiographic assessment of the aortic valve and root, evidence for aortic valve repair, guidelines and indications, repair in aortic dissections, paediatric aortic valve repair, and alternatives to repair including the Ross procedure will be covered by an esteemed international faculty.
The programme will also include a ‘failure session’, in which attendees will discuss cases all the way from echo analysis to surgical repair, learning how to identify predictors of repair failure as well as the bailout techniques available to them when such situations arise. Lectures on how to set up a new aortic valve repair programme will also be given.
The third day of the course will provide wet lab training, allowing attendees to practice what they have learned on cadaveric hearts within the historical laboratory of anatomy in Paris, du Fer à Moulin. There will be an international faculty to supervise, support and provide hands-on teaching during this session.
As this course reflects the multi-disciplinary aspect of aortic valve repair, course delegates could include cardiac surgeons and echocardiographers (cardiologists and anaesthetists) who are willing to start, or are already part of, a valve-sparing aortic root replacement and aortic valve repair programme. Advanced residents interested in the field of valve repair are also welcomed.
The 2021 ESC/EACTS guidelines for heart valve disease recommend valve-sparing aortic root replacement with aortic root dilatation irrespective of the degree of AI (Class IB evidence), with aortic valve repair considered in selected patients. However, despite increasing evidence that aortic valve repair leads to better survival, fewer adverse valve-related events and better quality of life when compared to prosthetic valve replacement,
uptake among surgeons is still low. This brings into question a lack of standardisation of aortic valve repair techniques. This EACTS course aims to tackle this problem by teaching a step-by-step standardised and reproducible technique to help surgeons and physicians interested in starting or improving an aortic valve repair programme.




