

INNOVATIVE RESEARCH PAGE 48 How Duke’s Moon Helps Civilians Orbit Earth PAGE 4 FACULTY SPOTLIGHT with Elizabeth B. Malinzak, MD PAGE 34 PERIOPERATIVE MEDICINE FORGING the PATH to Surgery and Recovery p28




















D U KE AN E S T H E SIO L O GY | 2 What We Do Changes The World M I SS I ON : E x tra o r din ar y care t h ro ugh a uniqu e c ul t u re of inn o v at i o n , e du cat ion , researc h , a nd p ro f ess i o n a l g ro w t h .
A1-Mediated Mitochondrial Protection to Ameliorate Surgical Kidney
Jamie Privratsky, MD,


Implementation of Community Co-Led Maternal Sepsis Care Practices to Reduce Morbidity
Mortality from Maternal Infection by Melissa E. Bauer,
Characterizing Blood-Brain Barrier Breakdown in Sleep Apnea and Postoperative Delirium by Michael Devinney, MD,

BLUE PRINT 2022 | 1 Contents FEATURE Volume 12 . 2022 2 Message from the Chair 10 Division Highlights DREAM CAMPAIGN 41 Donor Honor Roll 42 About DIG 44 2022 DREAM Innovation Grant Recipients INNOVATIVE RESEARCH 48 Annexin
Injury by
PhD 50 Large-Scale
and
DO 52
PhD GLOBAL HEALTH 54 Blogs from Abroad: Ghana RESIDENCY RECAP 60 Resident Spotlight 62 Alumni Shoutout ALUMNI NOTES 64 Q&A with Dr. Laura Niklason DEPARTMENTAL 68 Departmental Faculty 34 28 4 How Duke’s Moon Helps Civilians Orbit Earth FACULTY SPOTLIGHT with Elizabeth B. Malinzak, MD COVER | PERIOPERATIVE MEDICINE Forging the Path to Surgery and Recovery
BluePrint
VIEW ISSUES ONLINE:
PLEASE CONTACT US:
DUMC
EDITOR
Stacey
W
GRAPHIC
Lacey
CONTRIBUTING WRITERS
Jennifer Bringle
Stacey Hilton
Ratna Swaminathan
Duke Anesthesiology Faculty &

PROOFREADERS
Christopher Keith Melinda Macalino
John “Jack” Newman
Cheryl Stetson
CONTRIBUTING PHOTOGRAPHERS
John “Jack” Newman
Duke Anesthesiology Faculty & Staff
WEB ADMINISTRATOR
Christopher Keith
CONNECT WITH US: Anesthesiology.Duke.edu
hen is it going to end? I imagine most of us spent the last year wondering (perhaps fearful is a better word) when this pandemic will ever end? But is that really the only or even the right question?
If all we do is spend our time navigating away from our fears, will we ever get to the future we have always dreamed about? Too often we are so driven by our fears, perhaps even paralyzed by it, that we miss the many opportunities that are right in front of us. Rather than wondering when this will ever end, should we instead be asking what it is that we should be beginning?
As you read through this edition of BluePrint, I hope you will see the many ways that Duke Anesthesiology has advanced, despite the immense challenges we have faced. In all areas of our mission, our faculty, trainees, nurses, and staff have moved beyond fear and chosen to be courageous. In the pages that follow, you will read of all their new “beginnings.” And while we are immensely proud of all the people and their accomplishments, much work remains. For example, the greatest harm from the pandemic may be the loss of community, augmented by virtual platforms that increased convenience but at the cost of depersonalization. Thus, we must work tirelessly to reestablish the relationships that are the very core of our existence. Equally important is demonstrating our care for those around us. Let us therefore choose to be compassionate, because it is only then we will heal…and thrive. The wounds are deep and the pain is great but let us take these first steps and above all, let hope abound. In this season of uncertainty, remember that whatever we fear will establish the boundaries of our freedom. It is clear that even the courageous experience fear, so if both the courageous and the cowardly experience fear, why not choose to be courageous? What then should you be running to instead of running from?
MESSAGE FROM THE CHAIR
is published once a year by Duke Anesthesiology. This issue was published in August 2022. Your comments, ideas and letters are welcome.
BluePrint.DUHS.Duke.edu
Duke Anesthesiology BluePrint Magazine
3094 Durham, NC 27710 blueprint@duke.edu
IN CHIEF
Hilton CREATIVE DIRECTOR Stacey Hilton
DESIGNER
Chylack, phase5creative.com
Staff
Sincerely,
Joseph P. Mathew MD, MHSc, MBA
In all areas of our mission, our faculty, trainees, nurses, and staff have moved beyond fear and chosen to be courageous.
MARCH
30, 2022 2 | DUKE ANESTHESIOLOGY




BLUE PRINT 2022 | 3

How Duke’s Moon Helps Civilians Orbit Earth
BY JENNIFER BRINGLE
With civilian space travel now occurring on a seemingly regular basis—seven rockets with civilian crews and passengers launched in 2021 alone— the expertise of Dr. Richard Moon is uniquely in demand. Moon serves as medical director of the Duke Center for Hyperbaric Medicine and Environmental Physiology (CHMEP), as well as director of the Anesthesiology, Surgery, and Environmental Physiology Study Program (ASEP) at Duke. His knowledge is sought after to ensure that civilian crews can safely enter and conduct a mission in space.
“We are one of the few facilities that can do this,” Moon said. “We have altitude capability, we have an active lab, we have recompression facilities—we’ve been in the business for a long time.”
The Duke Center for Hyperbaric Medicine and Environmental Physiology is a critical care-oriented, hyperbaric facility and the Southeast’s regional referral center for hyperbaric medicine. It is the only civilian hyperbaric facility in the United States certified by the US Navy.
The facility is internationally recognized for its research in the areas of carbon monoxide poisoning, diving physiology, decompression sickness, oxygen toxicity, and altitude physiology. Moon has been with the center since 1979, specializing in the study of cardiorespiratory function in humans exposed to
environmental conditions ranging from 2,250 feet of seawater depth to high altitude. His work also touches on gas exchange during diving, the pathophysiology of immersion pulmonary edema, the effect of anesthesia and postoperative analgesia on pulmonary function, and monitoring tissue oxygenation.
“I have always been interested in the physiology of extreme environments—hypoxia, altitude, diving,” he said. “I came to Duke because of the work that the university had been doing and because of the lab facility—Duke was a natural fit for me.”
The combination of Duke’s facilities and Moon’s expertise makes the center the right fit for space crew training exercises, as well, specifically hyperbolic training that simulates the sensation of a loss of cabin pressure that could trigger hypoxia, or a lack of sufficient oxygen.
“We train for the possibility of a leak in the cabin, in which a space crew would experience a reduction in pressure - that could produce decompression sickness as well as hypoxia,” Moon said. “Symptoms of hypoxia often happen insidiously, and the danger is that people can be unaware of what’s going on.”
Hypoxia can cause unconsciousness, but before that happens, those suffering from the condition may experience symptoms such as shortness of breath and confusion. Loss of pressure in aircraft flying at high altitude has resulted in pilots losing consciousness
BLUE PRINT 2022 | 5 FEATURE
before they perceived any difficulty and could institute safety maneuvers. Moon refers back to 1980 when the LSU football coach, Bo Rein, was flying in a private aircraft from Shreveport, Louisiana to Baton Rouge, a 40 minute trip. However, inexplicably his aircraft climbed to 40,000 feet and headed east. The plane was eventually intercepted by an Air National Guard fighter aircraft over North Carolina at 41,600 feet—6,600 feet higher than its maximum certified ceiling. The military pilots could not see any sign of life in the cockpit and the aircraft continued to fly over the Atlantic and crashed when it ran out of fuel. Presumably, the pilot became hypoxic, failed to notice this, and did not begin breathing oxygen—a scenario that Moon’s training aims at helping civilian astronauts recognize and avoid.
During training of a crew, Moon will seal them in
Dr. Moon at the console of the Duke hyperbaric chamber.

the hyperbaric chamber and simulate being at an altitude of 25,000 feet. The astronauts may be asked to perform a series of tasks, from simple arithmetic to playing with a child’s toy that requires them to insert pieces of different shapes into their corresponding holes. Initially, Moon will have the crew breathe 100% oxygen via mask; each one then in turn removing their mask to initiate hypoxia for a brief period while they attempt the tasks. As the crew works, Moon will trigger hypoxia by having them remove their masks to breathe air.
“When at sea level, crews can typically accomplish these tasks in just a few seconds,” he said. “But when they become hypoxic, it becomes quite evident that they aren’t doing so well.”

6 | DUKE ANESTHESIOLOGY
“We train for the possibility of a leak in the cabin, in which a space crew would experience a reduction in pressure - that could produce decompression sickness as well as hypoxia.”
Moon’s exercises are designed to familiarize crews with the symptoms of hypoxia so they can react and supplement their oxygen supply before losing consciousness.
“It’s important that people recognize that hypoxia is occurring and start some measures to alleviate it,” Moon said. “It’s critical that they feel what it’s like.”
Moon can also subject crews to the effects of hypercapnia—excessive carbon dioxide in the bloodstream—during training sessions in the hyperbaric chamber. While the effects of hypercapnia are less noticeable—sluggishness, headache and shortness of breath—the condition can be dangerous if it persists.
“A rise in carbon dioxide is not as bad because it would happen much more slowly,” he said. “In an enclosed environment like a space capsule, carbon dioxide is scrubbed using absorbent materials like the ones used in firefighters’ gear and closed-circuit scuba divers. But if the carbon dioxide scrubber stops working or the system that pumps air in stops working, then carbon dioxide will accumulate.”
Extreme situations like space travel and diving aren’t the only scenarios where hypoxia and hypercapnia can occur. In clinical environments, patients suffering from conditions that inhibit breathing can trigger oxygen reduction and increased carbon dioxide in the body.
“People develop hypoxia for many reasons—such as
KEY LESSON of EXTREME TRAINING:
Subjective and objective effects of exposure to low oxygen and high carbon dioxide
CIVILIAN ASTRONAUT TRAINING
• Instruction on altitude decompression sickness, hypoxia and hypercapnia
• Exposure to high levels of carbon dioxide using a lab instrument
• Breath carbon dioxide up to 9% while doing “pencil-andpaper” testing to provide a sense of symptoms and effect on performance
• Gradually increase carbon dioxide by using a rebreather technique
• Neurocognitive performance at 25,000 feet simulated altitude in the hypobaric chamber

• Pre-breathe 100% oxygen at ground level for at least 30 minutes to reduce the risk of decompression sickness
• Crew members remove oxygen mask and perform neurocognitive testing, including calculations, number sequences, drawing, and shape matching
ONGOING HYPOXIA/ALTITUDE RESEARCH PROJECTS at the CHMEP
• Studying an experimental drug that is believed to enhance the diffusion of oxygen from lung to blood and blood to tissue
• Studying this drug with volunteers exercising at their VO2 max while measuring oxygen consumption and arterial blood gases
• Studying diving decompression procedures at altitude with volunteers at 8,000 - 12,000 feet
• Studying the possible effect of a short period of hyperoxia on recurrence of acute mountain sickness in altitude-acclimatized volunteers
• Studying epigenetic factors that may govern altitude tolerance by comparing experienced, high-altitude guides with lowland residents, in collaboration with University of Southampton, UK
• Studied the effect on exercise performance at altitude of a drug (riociguat) used to treat pulmonary hypertension
• Studying the effectiveness of perfluoromethane as a breathing gas to reduce decompression sickness during decompression from helium dives
• Studying the effectiveness of carbon monoxide breathing to enhance respiratory muscle training and its effect on diaphragm structure and function
BLUE PRINT 2022 | 7
FEATURE
NASACOLLABORA T I NO
The physiologist after whom Duke’s Frank Gregory Hall Environmental Laboratory is named, helped develop the pressure suits that NASA astronauts use today
2NASACOLLABORA
T I NO
CHMEP was instrumental in developing decompression tables, enabling construction of the International Space Station (ISS)

3NASACOLLABORA T I NO
The Duke flag has flown aboard the ISS in recognition of CHMEP researchers who have honed the procedures for proper suit decompression so astronauts can safely participate in extravehicular activity
4NASACOLLABORA T I NO
Regular consultant regarding NASA study protocols
FEATURE 1
istock
pneumonia and COVID,” he said. “High carbon dioxide occurs in illness because the lungs aren’t working normally, or breathing is insufficient to get rid of the carbon dioxide that body tissues are making.”
While astronauts—who are generally healthy and in peak physical condition— would likely only need supplemental oxygen to overcome hypoxia or hypercapnia, in a clinical setting, more extensive remedies are generally employed.

“Giving oxygen is one way to treat it, and mechanical ventilation is another,” Moon said. “In the hospital, you give small amounts of oxygen, and if that doesn’t work, you administer increasing concentrations. If that isn’t sufficient, you can give them CPAP, which works for some people, but a lot of people require mechanical ventilation after inserting a tube into the trachea.”
Duke’s CHMEP is the nation’s first and largest civilian hyperbaric chamber.
Over the four decades that Moon has been at Duke, he has seen significant advances in the understanding, prevention and treatment of hypoxia, both in extreme environmental and clinical scenarios. And with altitude-related hypoxia, Moon said one of the big questions his work aims to answer is how can humans adapt to high altitude conditions without experiencing adverse consequences of hypoxia.
“We know if you take someone to 29,000 feet they lose consciousness within a minute or two, and yet people have actually climbed Mount Everest at 29,000 feet without oxygen, so how does that happen?” he said.
According to Moon, one of the instances that may hold answers to that question is the rapid adaptation process that happens to babies at birth. While in utero, babies live in a hypoxic environment, but upon birth, their bodies quickly adapt to the oxygen-rich environment outside the womb.
“They lose that adaptation very rapidly,” he said. “We’re still working on how that happens and ways to reverse it, to bring back hypoxic adaptation.”
Moon said unlocking how that adaptation process works could not only help humans better adjust to altitude, but it also could positively impact patient care in clinical settings.
“Imagine the therapeutic advantages of being able to administer a drug to a hypoxic patient in order to induce tolerance to hypoxia,” he said. “That would have huge implications for critical care medicine.”
That intersection between the critical care arena and extreme environmental applications continues to drive Moon’s work. And while uncovering those potentially life-saving clinical developments continues to be the ultimate goal, opportunities like contributing to civilian space missions reminds Moon that his work has far-reaching implications.
“While studying extreme environments like diving and altitude may seem like niche activities, it’s surprising how often the observations help us take care of patients.” BP
BLUE PRINT 2022 | 9 FEATURE
Dr. Moon outside G chamber observing an experiment.
A State-of-the-Art Clinical Pathway and Collaboration

Improved patient experience, novel care pathways, collaboration, and enhanced outcome are ambulatory division goals since its inception at the North Pavilion. When the Duke Ambulatory Surgery Center Arringdon opened, the division applied these strategies to lead a multidisciplinary team performing joint arthroplasties at Arringdon. Traditionally done in the hospital with extended stay, Arringdon offers a state-of-the-art, sameday pathway for patients and surgeons. The Duke Ambulatory Surgery Center Arringdon has completed more than 4,250 cases and more than 200 same-day total joint arthroplasty procedures, since opening in August 2021. This success was propelled by a collaboration of nursing, administration, physical therapy, patient education, finance, marketing, anesthesiology, and orthopaedic surgery. Extensive planning was critical to ensure the safe transition of procedures from the traditional inpatient hospital stay to Arringdon. Inpatient metrics were reviewed, specific opportunities were identified and measures to address those opportunities were targeted. Specialized patient pathways were created, detailing patient assessment, preparation and optimization for same-day surgery. Treatment plans and protocols were developed, ensuring optimal patient care, safety, satisfaction, and outcome. Open lines of communication fosters ongoing evaluation of the program.
CARDIOTHORACIC ANESTHESIOLOGY
Duke Anesthesiology and Duke Orthopaedic Surgery continually collaborate to appraise patient selection criteria and patient management protocols maximizing same-day surgery success. Physical therapy provides pre-habilitation prior to surgery and facilitates safe same-day rehabilitation and discharge. Nursing staff have taken on additional roles as total joint patient coordinators, guiding patients through the perioperative process. As coordinators, nurses lead preoperative patient education classes, provide open access for patient communication, and perform patient follow-up after surgery. During this followup, data is collected for an anesthesiology designed REDCap database, an important tool to promote patient-centered care. The teamwork of the Arringdon Total Joint Arthroplasty Program was brought to the forefront during the second wave of the COVID pandemic. The center was tasked with providing care to the backlog of total joint patients initially scheduled for the main hospital. This challenge was accomplished without compromise. Utilizing expertise in both ambulatory and regional anesthesia, the Ambulatory Anesthesiology Division has played a critical role in the design and implementation of the Arringdon Total Joint Arthroplasty Program.

Advancing the CTA Learning Health Unit and Sustaining our Growth
The division’s Cardiothoracic Anesthesiology (CTA) Learning Health Unit is focused on the strategic goal of improving datadriven approaches (specific, measurable and actionable data), data liquidity and analytics infrastructure to systematically integrate internal data and experience with external evidence in a feedback cycle for learning and improvement. The unit aims to deliver the highest quality, safest, most efficient, and most up-to-date care to Duke cardiothoracic surgical and critically ill patients and their families (patient-centric, family-centric), make the division the best place to work (faculty-centric, teamwork and equity), and empower its academic missions of education and research. Highlights of cross-functional leadership teams and initiatives include: 1) improving Cardiothoracic Operating Room efficiency (team leader, Dr. Negmeldeen Mamoun) – clarifying preoperative to OR timeline, transparency and accuracy of delay reasons, visible in real-time, multistakeholder engagement, implementation of turnover timer and concept of parallel processing (outcome – improved divisional first case on-time starts and turnover time); 2) multidisciplinary cardiothoracic performance improvement initiatives (team leaders, Drs. Mamoun, Ian Welsby and Mihai Podgoreanu) for prolonged
mechanical ventilation, acute kidney injury, wound infection, reoperation, stroke, mortality, and thoracic transplant outcomes (team leader, Dr. Brandi Bottiger) (outcome – The Society of Thoracic Surgeons 3-star performance ratings across all major cardiac surgical domains); 3) divisional culture of continuous learning and improvement supported by state-of-the-art learning management infrastructure to systematically disseminate, adapt, adopt, and apply evidence – using the innovative Duke Sakai system for its Adult Cardiothoracic Anesthesiology Fellowship educational curriculum (team leaders, Drs. Bottiger, Anne Cherry, Nazish Hashmi, Rebecca Klinger and Angela Pollak), perioperative echocardiography education portfolio (team leaders, Drs. Alina Nicoara and Pollak), and complemented by departmental-wide faculty development resources for teaching and learning (Drs. Ashley Grantham and Mark Stafford-Smith); 4) evolving from patient monitoring to clinical surveillance through Project Symphony, which entails streaming and integrating medical device data combined with predictive analytics and condition-specific algorithms to detect emergent clinically actionable events (physician champion, Dr. Podgoreanu).
10 | DUKE ANESTHESIOLOGY DIVISION HIGHLIGHTS AMBULATORY ANESTHESIOLOGY
Davis Ambulatory Surgery Center
Duke Fertility Center
Duke Raleigh
Duke Regional
Holly Springs Surgery Center
Johnston Health
MedCenter Mebane
Specialty Hospital
Orthopaedics Surgery Center
CRITICAL CARE MEDICINE
New Leadership Roles, A Flourishing Division
Despite the COVID-19 pandemic, the division continued to push forward its mission of improving the lives of critically ill patients at Duke and worldwide in all domains (clinical care, education and research). In September 2021, Dr. Raquel Bartz assumed a new leadership position outside of Duke, and Dr. Vijay Krishnamoorthy was appointed chief of the Critical Care Medicine (CCM) Division in February. In the clinical domain, division faculty continued to provide outstanding clinical care to critically ill patients across its six intensive care units, including weathering several COVID-19 surges (Delta and Omicron variants) and staffing shortages. Dr. Kathleen Claus was appointed associate medical director for the Duke Regional Hospital Critical Care Unit, Dr. Nitin Mehdiratta was appointed co-medical director for the Duke University Hospital Surgical Intensive Care Unit, and Dr. John Lemm was appointed chair of the Critical Care Committee at the Durham VA Medical Center. In the education domain, Dr. Nazish Hashmi was appointed program director for the Critical Care Medicine Fellowship Program. She implemented and led a re-vamped education program primarily on a virtual platform, as well as enhanced collaboration with other CCM fellowship programs across the health system. Dr. Yuriy Bronshteyn continued to innovate in ultrasound education, including the creation of an educational echocardiography program, which also supported operations


at the Durham VA Medical Center. In the research domain, the CCM Division’s research program continued to flourish, despite the operational challenges imposed by the pandemic. The division continued to build programs in basic science, clinical/translational research, and population health; and faculty published their work in several high-impact journals, including The New England Journal of Medicine and The Lancet. The Critical Care and Perioperative Population Health Research (CAPER) Unit surpassed $1.2 million in industry support and presented 14 abstracts at the Society of Critical Care Anesthesiologists and the International Anesthesia Research Society national meetings. Multiple new federal grants were awarded to divisional investigators, including Drs. Paul Wischmeyer (NIH R01$4,059,863 – “Remotely Monitored, Mobile Health-Supported High Intensity Interval Training After COVID-19 Critical Illness”), Jamie Privratsky (NIH R01 - $1,610,000 – “Novel Mitochondrial Protective Properties of Annexin A1” - see
), and Michael Devinney (NIH R03 GEMSSTAR - $322,000 – “The Association of Blood-Brain Barrier Breakdown with Sleep Apnea and Postoperative Delirium”
BLUE PRINT 2022 | 11 DIVISION HIGHLIGHTS
page 48
- see page 52). COMMUNITY
NC
Triangle
8,240 383 21,429 12,858 2,379 11,062 3,110 8,714 2,808 CASE TOTAL: 70,983 Dr. Vijay Krishnamoorthy
Making Progress: Ending the “Silent Epidemic” of Perioperative Malnutrition
Poor nutritional status during the perioperative period continues to be a globally acknowledged “silent epidemic,” as it is often unrecognized and untreated, and is associated with significant adverse postoperative outcomes. Dr. David Williams, one of the few nutritionally-focused and Perioperative Medicine Fellowship trained anesthesiologists in the nation, is making great clinical strides in the nutrition subspecialty. He serves on the Duke University Hospital’s Total Parenteral Nutrition (TPN)/ Nutrition Support Service where he oversees a multidisciplinary team of dietitians and pharmacists who provide nutrition support for nutritionally-impaired hospitalized patients. This year, the team was awarded the American Society for Parenteral and Enteral Nutrition (ASPEN) Clinical Nutrition Team of Distinction Award – one of ASPEN’s highest achievements. It recognizes excellence in interdisciplinary clinical nutrition practice in institutions; clinical nutrition teams that receive this designation demonstrate the highest care to their patients. Williams also conducts preoperative assessment and medical optimization of high-risk patients undergoing elective noncardiac surgery in the department’s novel Preoperative Anesthesia

and Surgical Screening (PASS) Clinic. Recognizing the importance of optimizing nutrition status as far upstream from surgery as possible, Williams, his mentor, Dr. Paul Wischmeyer, and the POET nutrition team have worked to develop and validate a new preoperative nutrition screening tool to detect patients who are at risk for malnutrition and poor postoperative outcomes. This work was published in the Journal of Parenteral and Enteral Nutrition. Having completed a research fellowship at the Duke Clinical Research Institute and the Nestlé Nutrition Institute Clinical Nutrition Fellowship for Physicians in 2019 (the first anesthesiologist in the nation to do so), Williams is also interested in narrowing the gap in nutrition health inequality, through an ASPEN Rhoads Research Foundation grant. He is currently collaborating with the department’s Critical Care and Perioperative Population Health Research (CAPER) Unit to investigate the role of malnutrition and nutrition delivery on surgical outcomes in underserved patients.
Dr. David Williams
NEUROANESTHESIOLOGY, OTOLARYNGOLOGY & OFFSITE ANESTHESIOLOGY
International Leadership and Scientific Discoveries
Divisional faculty, Dr. Michael “Luke” James, was appointed to two Duke leadership roles: 1) the assistant vice chancellor for Duke-NUS Research in which he assists the vice chancellor of Duke-NUS Affairs by providing support and oversight for building research partnerships and collaborations with DukeNUS, and 2) a coordinate appointment as assistant dean in the Duke-NUS Office of Academic and Clinical Development, in which he oversees joint activities between Duke-NUS and SingHealth. James is working with the vice chancellor for DukeNUS Affairs to identify areas of key strategic overlap between Duke Health and the SingHealth Duke-NUS Academic Medical Center; construct specific, collaborative platforms for building alignment; and create programs to support, resource and execute these new collaborative efforts.
Two major scientific discoveries also came from a faculty in this division, Dr. Miles Berger. He led a study, published in February in the Annals of Clinical & Translational Neurology, that revealed cognitive changes post non-neurologic and noncardiac surgery were not associated with changes in Alzheimer’s disease-related biomarkers in older patients. This finding could help ease concerns that Alzheimer’s disease risk might be increased by major surgeries and/or general anesthesia.* Another
 Dr. Michael “Luke” James
Dr. Miles Berger
Dr. Michael “Luke” James
Dr. Miles Berger
study, published in the British Journal of Anaesthesia with Berger as senior author, revealed that individuals who carry the most common genetic risk factor for late onset Alzheimer’s disease (APOE4) have similar cognitive trajectories within one to two months after non-cardiac surgery as patients who do not carry this genetic risk factor. However, older patients who have the APOE4 allele have a pattern of functional brain hyperconnectivity prior to surgery (as compared to non-carriers), and this hyperconnectivity pattern is selectively reduced after surgery in APOE4 carriers - which could represent a mechanism that leads to the greater long-term postoperative decline that has previously been observed in APOE4 carriers. Berger’s ongoing research includes the study of neuroinflammatory mechanisms in both perioperative neurocognitive disorders (using the recently completed INTUIT study data) and as a mechanism for synapse loss and cognitive decline in APOE4 carriers.

12 | DUKE ANESTHESIOLOGY DIVISION HIGHLIGHTS
GENERAL, VASCULAR & TRANSPLANT ANESTHESIOLOGY
ORTHOPAEDICS, PLASTICS & REGIONAL ANESTHESIOLOGY
A Year of Clinical Innovation
The regional division has continued to build on a legacy of clinical innovation on multiple fronts. Dr. Michael Bullock and team published a landmark paper shedding light on the mechanism of ischemic tourniquet hypertension with their description of a novel “femoral artery block” or FAB. This technique targets the sympathetic nerve fibers surrounding the femoral artery and was shown to significantly decrease the incidence of tourniquet hypertensive response under anesthesia, garnering praise from other researchers in the field. Similarly, the division described an approach to blocking genicular nerves for knee replacement
PAIN MEDICINE
A Focus on Patient Safety and Outcomes
The division has focused on several patient safety initiatives with the target of improving patient outcomes. To optimize patient safety related to procedural care, a clinic safety curriculum was created for the Duke Pain Medicine Clinic with the assistance of Drs. Ankeet Udani and Brad Taicher. In addition to creating a standard workflow for periprocedural care, the group (including all physicians, nurses and staff) participated in a safe cultures workshop led by the Duke Patient Safety Office. Additionally, two separate patient simulation sessions were led by Udani in the Duke Human Simulation and Patient Safety Center with a focus on periprocedural workflows, communication among team members, and disclosure of adverse events to patients and their families. The curriculum was created in a fashion to allow adaptation to other procedural areas across Duke Health. Coordinated with these efforts, the pain medicine fellows’ quality improvement project focused on creation of a separate presentation and discussion regarding local anesthetic systemic toxicity assessment and treatment. They demonstrated that all nursing team members were able identify the correct bolus and maintenance infusion dose of intralipid for standard management compared with only 33% prior to the sessions. These findings were presented at the American Society of Regional Anesthesia and Pain Medicine (ASRA) Meeting and the Duke Health Quality and Safety
and in a randomized controlled trial against sham block, demonstrated a 60% reduction in opioid consumption on the first postoperative day. This technique has since gained traction in the regional world and has been implemented at multiple centers throughout the country, as well as Europe, Australasia and Latin America. The division also worked with neurosurgeon Dr. Mohammad Abd-El-Barr to pioneer a new approach to awake spine surgery, utilizing spinal anesthesia and ultrasound-guided erector spinae plane blocks.

Conference and have been submitted for publication. Dr. Padma Gulur’s PROMIS Lab has also focused on patient safety outcomes related to opioid stewardship as well as neuromodulation procedures. The data indicates lower complication rates for both intrathecal pump and spinal cord stimulator implants, compared with previously reported studies. Six posters on related content were presented to the American Society of Anesthesiologists and ASRA. Additionally, the division has seen continued clinical growth at its Wake County practices. Dr. Daniela Vivaldi joined the orofacial pain program in September of 2020, partnering with Dr. Aurelio Alonso, to expand and strengthen the program.

BLUE PRINT 2022 | 13 DIVISION HIGHLIGHTS
PEDIATRIC ANESTHESIOLOGY

Growth, Excellence and Leadership
The division continues to excel locally and nationally, including the mentorship of trainees at national meetings where Duke has been a top leader of research awards. Drs. Brad Taicher and Mayumi Homi mentored Dr. Lori Jones to a first place John J. Downes Resident Research Award at the Society for Pediatric Anesthesia (SPA) conference. Since stepping down as division chief, Dr. Allison Ross has been appointed as the department’s director of professional development which allows her to use her coaching skills and experience to assist with career growth. She has also served as a co-champion in the Duke Children’s strategic planning on health disparities and diversity, equity and inclusion initiatives and continues to be a site reviewer for the American College of Surgeons Children’s Surgery Verification. Dr. Lisa Einhorn joined the Acute Pain Service team and is a co-champion for Duke Children’s strategic plan for pain. Taicher has expanded his departmental leadership position in quality nationally with his appointment as the associate vice chair of the SPA Quality and Safety Committee. His organizational and leadership strengths are being further utilized in his new roles as the assistant director of Anesthesia Perioperative Services and medical director of Pediatric Perioperative Services. Dr. John Eck was elected president of the Association of Anesthesiology Subspecialty Program Directors, a two-year position leading more than 350 anesthesiology fellowship program directors. Dr. Guy Dear is making sure the division is kept updated with its electronic
health record as a member of the pediatric anesthesia subspecialty steering board for mobile applications and co-chair for NORA implementation at EPIC headquarters. Dr. Annie Udani is leading the group in a multidisciplinary initiative with the general surgical team using ERAS in pediatrics for novel procedures. Dr. Wads Ames is on the national Congenital Cardiac Anesthesia Society (CCAS)-Society of Thoracic Surgeons (STS) Data Committee and represents Duke in the Hemostasis Interest Group. He is also the new clinical director for pediatric cardiac anesthesia and is bringing a new energy and new research in AKI and regional anesthesia to the pediatric cardiac group.
Division Expands Access to Procedural Therapy for Post-Traumatic Stress Disorder


Post-traumatic stress disorder (PTSD) is a mental health condition that may occur in people who have experienced or witnessed a traumatic event, such as war or combat. PTSD affects up to 30% of veterans and has severe negative impacts on their lives, including early mortality, decreased quality of life, and increased health care utilization. Treatment for this disease is difficult and requires years of intensive psychiatric and psychological care.
Veterans in the Durham VA Health Care System experiencing the debilitating effects of PTSD now have expanded access to a novel therapy that promises to better manage their symptoms. Stellate ganglion blocks (SGB) have been used as a pain therapy since the 1920s. Over the past 10 years, physicians have started using stellate ganglion blocks to treat the symptoms of PTSD and other psychiatric conditions. Using a small needle and real-time ultrasound guidance, the nerves of the stellate ganglion are blocked. These
nerves project to the amygdala, the emotional center of the brain.
Temporarily blocking these nerves can result in significant improvement in the hyperarousal, anger, hypervigilance, and heightened startle reflex symptoms that are typical in PTSD patients. In collaboration with Dr. Bruce Capehart of Duke Psychiatry and the Durham VA PTSD clinic, Duke Anesthesiology’s Drs. Thomas Van de Ven and Lance Roy are providing expanded access to stellate ganglion blocks in both the Durham VA pain clinic and operating suites. Van de Ven and Roy are planning for expansion of the SGB program to include research to study ways to optimize patient selection and outcomes.
14 | DUKE ANESTHESIOLOGY DIVISION HIGHLIGHTS
VETERANS AFFAIRS ANESTHESIOLOGY SERVICE
Dr. Thomas Van de Ven Dr. Lance Roy
WOMEN’S ANESTHESIOLOGY
Training Expansion and Global Learning
The division’s Obstetric Anesthesiology Fellowship Program continues to thrive under the leadership of Dr. Jennifer Dominguez. In the first year following the expansion of the fellowship to two positions, the fellows were awarded first place in the best paper of the meeting and the Gertie Marx competitions at the 2021 annual meeting of the Society for Obstetric Anesthesia and Perinatology. The program continues to attract strong applicants and will welcome two future fellows who will complete dual fellowships in obstetric anesthesia and cardiothoracic anesthesia (Dr. Lilian Earnest, 2023-2025) and obstetric anesthesia and critical care medicine (Dr. Rebecca Himmelwright, 2024-2026).
Divisional faculty were successful in securing several grants. Dr. Melissa Bauer was awarded a two-year, $1,575,463 NIH UG3 grant for her project titled, “Large-Scale Implementation of Community Co-led Maternal Sepsis Care Practices to Reduce Morbidity and Mortality from Maternal Infection” (see page 50). Dr. Marie-Louise Meng received a Duke/UNC CTSA Consortium Collaborative Project Award for a project

 Dr. Marie-Louise Meng Dr. Adeyemi Olufolabi Dr. Jennifer Dominguez
Dr. Marie-Louise Meng Dr. Adeyemi Olufolabi Dr. Jennifer Dominguez
titled, “Maternal Morbidity at Duke and UNC: A Multicenter Examination of Risks Factors and Trends of Pregnancy Related Morbidity” and a Mentored Research Training Grant from the Foundation for Anesthesia Education and Research for her project titled, “Cardiovascular Risk Prediction for Improved Maternal Health.”
Dr. Adeyemi Olufolabi continues his global health work in Africa, engaging Duke Anesthesiology residents and faculty. In January 2022, residents Drs. Lori Jones and Savion Johnson, together with divisional faculty member, Dr. Cameron Taylor, joined Olufolabi in Ghana for clinical and didactic teaching (see page 54).

CENTER FOR PERIOPERATIVE ORGAN PROTECTION
The Center for Perioperative Organ Protection (CPOP) continues to strive in improving the standard of perioperative care through innovative research as published in the most prestigious journals. Dr. Luis Ulloa, director of CPOP, was invited by Nature to write an article about the new advances on nerve stimulation as a promising emerging field to control metabolism, inflammation and organ function.* Regarding clinical research, Dr. Miles Berger and collaborators reported in the British Journal of Anaesthesia that APOE4 carriers have greater postoperative decrease in functional connectivity in key Alzheimer’s disease-risk regions via Aβ-independent mechanisms.**
2021-2022 has been a successful year for CPOP investigators receiving new funding from the National Institutes of Health (NIH). Dr. Wei Yang received two NIH R01 grant awards; one

project focuses on “The Unfolded Protein Response in Ischemic Stroke” to study whether the activation of the unfolded protein response (UPR) improves the outcome after stroke. The second project, titled “Immunosuppression

After Cardiac Arrest and Resuscitation,” aims to find novel immunomodulatory targets that can be exploited to advance post-resuscitation care and improve cardiac arrest prognosis. The CPOP has also strived in mentoring new investigators to receive NIH funding; Dr. Jorn Karhausen earned his first NIH R01 to study “Platelet-Mast Cell Interactions as Determinants of the Vascular Pathology in Septic Shock” and Dr. Jamie Privratsky received his first NIH R01 (in collaboration with Dr. Hagir Suliman and Ulloa) to study “Novel Mitochondrial Protective Properties of Annexin A1.”*** The CPOP is also forming multidisciplinary clinical and basic science teams of competitive investigators for NIH proposals, including program project grants. Karhausen, Yang and Ulloa earned a funded score to study “Vagal Control of Tissue SUMOylation as a Novel Anti-Inflammatory Target in Inflammatory Bowel Disease.” Dr. Karthik Raghunathan and Ulloa acquired a score on a $3.8M NIH/NCCIH application for “Clinical and Experimental Analyses of Music Medicine in Perioperative Settings.”
*Ulloa L. Nature 598, 573-574. (2021).
**Browndyke et al. Br J Anaesth 127, 917-928. (2021).
***Suliman, et al. Front Physiol 12, 683098. (2021).
BLUE PRINT 2022 | 15
DIVISION | CENTERS & PROGRAMS | HIGHLIGHTS
Physician-scientists
striving to understand molecular, cellular and organ system interactions during acute injury and recovery in the perioperative period across the aging spectrum, using a multidisciplinary research approach to make new discoveries.
Dr. Wei Yang
CENTER FOR TRANSLATIONAL PAIN MEDICINE
STING Immunotherapy: A Complementary Approach to Treating Bone Cancer Pain
Cancer is a leading cause of death in North America. Many common cancers, including lung, prostate and breast, metastasize to bone as the disease progresses, resulting in tumor growth and destruction. This process is often very painful; more than 75% of patients with advanced-stage bone cancer report moderate to severe pain – pain that is often refractory to medications, including opioids.
Two new studies give hope that patients may one day find relief through targeting of a novel immune regulator called STING. Research led by Dr. Ru-Rong Ji, director of the Center for Translational Pain Medicine, reveals that the activation of STING




produces an immune response capable of both reducing bone tumor progression and pain through a complementary mechanism that acts directly on the primary sensory neurons that innervate the bone. Thus, STING activation could produce relief for patients and is also immediately translatable.
Source: Harding, Erika. “STING Immunotherapy: A Complementary Approach to Treating Bone Cancer Pain.” Pain Research Forum, 17 Dec. 2021.
“STING Controls Nociception via Type I Interferon Signalling in Sensory Neurons.” Donnelly CR, Jiang C, Andriessen AS, Wang K, Wang Z, Ding H, Zhao J, Luo X, Lee MS, Lei YL, Maixner W, Ko MC, Ji RR. Nature. 2021 Mar; 591(7849):275-280.
“STING Suppresses Bone Cancer Pain via Immune and Neuronal Modulation.” Wang K, Donnelly CR, Jiang C, Liao Y, Luo X, Tao X, Bang S, McGinnis A, Lee M, Hilton MJ, Ji RR. Nat Commun. 2021 Jul 27; 12(1):4558.
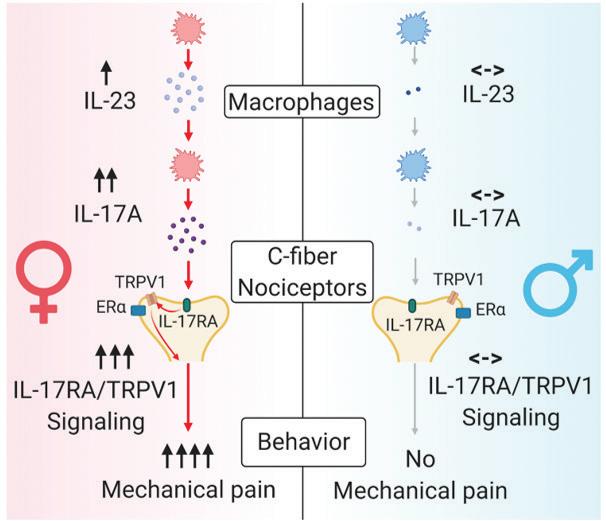
Although female patients have high incidence of developing chronic pain, the majority of preclinical studies have been conducted in male animals. Investigators at the Center for Translational Pain Medicine study sex dimorphism in pain and have revealed novel signaling mechanisms that control pain in males and females.
The Pain Research Forum’s most popular news story of 2021 examined the discovery of a sex-specific pain mechanism from Dr. Ru-Rong Ji’s Sensory Plasticity and Pain Research Laboratory.
“IL-23/IL-17A/TRPV1 Axis Produces Mechanical Pain via Macrophage-Sensory Neuron Crosstalk in Female Mice.” Luo X, Chen O, Wang Z, Bang S, Ji J, Lee SH, Huh Y, Furutani K, He Q, Tao X, Ko MC, Bortsov A, Donnelly CR, Chen Y, Nackley A, Berta T, Ji RR. Neuron. 2021 Sep 1; 109(17):2691-2706.
Recent work from Dr. Andrea Nackley’s Translational Pain Research Laboratory has demonstrated that male animals are more sensitive to the inhibitor of HSP90, a heat shock protein. By contrast, a much higher dose of the inhibitor is required to achieve analgesic and antiinflammatory effects in females.


“Expression of Ectopic Heat Shock Protein 90 in Male and Female Primary Afferent Nociceptors Regulates Inflammatory Pain.” Wang Y, Scarneo SA, Kim SH, Zhang X, Chen J, Yang KW, Hughes P, Haystead T, Nackley AG. Pain. 2021 Oct 12. Wang et al., 2021, Pain (cover story).

16 | DUKE ANESTHESIOLOGY
HIGHLIGHTS | CENTERS & PROGRAMS
Dr. Ru-Rong Ji
Dr. Kaiyuan Wang
Dr. Christopher Donnelly
Dr. Xin Luo
Dr. Andrea Nackley Dr. Yaomin Wang
Improving Perioperative Outcomes for Patients Through POET

The department’s PeriOperative Enhancement Team’s (POET) anemia team played a central role in getting patients to surgery safely during COVID-related critical blood shortages. The identification and treatment of preoperative anemia is now imperative, not optional. The POET anemia team has continued to experience both overall growth, as well as expansion into the postoperative period to treat patients with anemia after cardiac surgery. Dr. Nicole Guinn and her team (Aime Grimsley, NP; Cindy Cellura, PA; Ivette Alvarez, PA; and perioperative medicine fellow, Dr. Mrugesh Thakkar) have treated more than 1,000 patients with anemia this past year. Guinn’s work on reducing blood transfusion and length of stay was recently published in the journal, Transfusion
The POET nutrition team treats an average of 57 patients per month, helping them to achieve their indi vidualized goals, whether that is to improve their nutrition intake or lose weight prior to surgery. Patients are now treated for a median of 15 days prior to surgery, with most achieving clinically-relevant goals. Drs. David Williams and Paul Wischmeyer, along with their team, continue to innovate in this field. Their work on the development and validation of a new screening tool to detect patients who are at risk for malnutrition and poor postoperative outcomes was published in the Journal of Parenteral and Enteral Nutrition
The POET sleep apnea team persevered in spite of COVID-related challenges that impacted workflow - including a recall on certain CPAP machines and supply chain shortages. These challenges inspired us to widen the focus of the POET program to include patients with diagnosed sleep apnea who do not use their CPAP therapy. Thakkar performed a quality improvement study to better understand the most common factors associated with CPAP non-adherence in the perioperative period and whether they may be modifiable. The results of this work were presented at the national Perioperative Medicine Summit.
In order to increase access and provide optimization services to as many patients as possible, we have developed a tiered approach to preoperative glycemic control. The result of a close
collaboration between the PASS clinic and POET diabetes team, led by Drs. Tracy Setji and Beatrice Hong, was the integration of e-consults into our workflow. E-consults allow for virtual communication and collaboration between the PASS clinician and diabetes clinician to confirm the best optimization plan while offering “one-stop shopping” for the patient. This novel approach to preoperative glycemic control has resulted in an increase in lead time between POET appointment and surgery (14 days). Furthermore, patients treated preoperatively by the POET diabetes team continue to sustain a lower A1C level for two years post POET intervention.
A revision to our scheduling template improved patient ac cess to preoperative allergy testing and oral penicillin challenge. This past year, 71 patients reported an allergy to penicillin and were referred to the POET allergy team. All of them were determined to no longer be penicillin-allergic and the diagnosis was removed from their chart - resulting in each patient receiving access to the best antibiotic for prevention of surgical site infection. The template revision has allowed the POET team to support ongoing quality initiatives on appropriate perioperative antibiotic administra tion within the departments of anesthesiology and surgery.
There is now compelling evidence that the most effective to bacco treatment includes individualized pharmacotherapy and intensive behavioral treatment. The POET smoking cessation team includes individualized evidence-based pharmacotherapy, provided by Emily Walter, NP, who specializes in tobacco treat ment, and multimodal intensive behavioral therapy provided by Andrea Pratt, LCSW. Both in-person and telemedicine-based services are now offered; the success rate for both formats (34% and 28% respectively) remains three-times as high as the success rate for patients using a quit-line or attempt to quit on their own. Our team continued to successfully support patients with novel approaches throughout the FDA voluntary recall of va renicline this past year. Furthermore, 89% of patients remained abstinent from tobacco three months postoperatively.
(Learn more about this unique perioperative and population health program in the cover story - page 28)
BLUE PRINT 2022 | 17 PROGRAM | HIGHLIGHTS
Duke Anesthesiology
NOTEWORTHY STATS Duk e A n e sth e siolo g y B Y T H E N U MB ER S J U LY 1, 2 0 20 - J U N E 3 0, 2 0 21 590 PUBLICATIONS CASES OR CASES: 145,710 OTHER SERVICES: 69,560 19 , 087 G E N E R A L , VA S C U L A R A N D T R A N S P L A N T ANESTHESIOLOGY VETERANS AFFAIRS A N E S T H E S I O L O G Y S E R V I C E 6,989 N E U R OA N E S T H E S I O L O G Y 4,951 W O M E N ’ S ANESTHESIOLOGY 9,529 C A R D I O T H O R A CI C ANESTHESIOLOGY 7,878 505 PA I N M E D I C IN E A M B U L AT O R Y ANESTHESIOLOGY 7,739 8,572 O RT H O PA E D I C S , P L A S T I C S A N D R E G I O NA L A N E S T H E S I O L O G Y 70,983 CO M M U N I T Y 9 , 477 PE D I AT R I C ANESTHESIOLOGY C R I T I C A L C A R E 19,008 PAIN VISITS 35,145 ACUTE PAIN SERVICE VISITS 15,407 18 | DUKE ANESTHESIOLOGY CARDIOTHORACIC ANESTHESIOLOGY 129 GENERAL, VASCULAR AND TRANSPLANT ANESTHESIOLOGY 75 CRITICAL CARE MEDICINE 72 CENTER FOR TRANSLATIONAL PAIN MEDICINE 63 WOMEN’S ANESTHESIOLOGY 57 NEUROANESTHESIOLOGY 48 CENTER FOR PERIOPERATIVE ORGAN PROTECTION 41 VA ANESTHESIOLOGY SERVICE 33 PAIN MEDICINE 24 ORTHOPAEDICS, PLASTICS & REGIONAL ANESTHESIOLOGY 21 PEDIATRIC ANESTHESIOLOGY 18 AMBULATORY ANESTHESIOLOGY 9 BY THE NUMBERS
July 1, 2020 - June 30, 2021
million
BASIC SCIENCES
$1,267,292
WOMEN’S ANESTHESIOLOGY 3 $1,201,948
GENERAL, VASCULAR AND TRANSPLANT ANESTHESIOLOGY 4 $1,056,396
CRITICAL CARE MEDICINE 4 $973,536
CARDIOTHORACIC ANESTHESIOLOGY 8 $603,652
ANESTHESIOLOGY SERVICE 3 $412,978
ORTHOPAEDICS, PLASTICS AND REGIONAL ANESTHESIOLOGY 1 $401,904 PEDIATRIC ANESTHESIOLOGY 1 $105,258
HYPERBARIC MEDICINE 2 $102,272
NEUROANESTHESIOLOGY 1 $99,820 PAIN MEDICINE 2 $10,082
Translational
1 6 R E S E A R C H L A B O R A T O R I E S $ 5.5 m illio n 182 C U RR E N T ACTIVE RESEARCH GRANTS TO TA L O F 18 NO N - C O M P E T IN G C O N T I NU I N G G R A N T S C hem ic a l Sens i ng, Pa i n an d In fl ammat i on R esea rc h L a b o r ato r y S ven-Er ic J o r dt, P h D H uman Pha r ma c o l ogy an d Phys i o l ogy L a b o r ato r y David MacLeod, MB BS Mo l e c u l a r Pha r ma c o l ogy L a b o r ato r y Madan Kwatra, PhD Pain Relief and Opioid Mitigation Innovation Science (PROMIS) Laboratory Padma Gulur, MD Duke Multi-Disciplinary Metabolic and Body Composition Assessment Team (MCAT) Laboratory Paul Wischmeyer, MD Laboratory of Mechanistic and Clinical Pharmacology Evan Kharasch, MD, PhD Multidisciplinary Brain Protection Program Wei Yang, PhD Peri-Operative Neurocognitive Research Team (PORT) Laboratory Miles Berger, MD, PhD F G H a ll Env ir onmenta l L a b o r ato r y Richard Moon, MD, CM, MSc, FRCP(C), FACP, FCCP Laboratory of Neuromodulation Luis Ulloa, PhD, MS N e r ve In j u r y an d Pa i n Me c han i s m L a b o r ato r y Thomas Van de Ven, MD, PhD Senso r y P l ast ici ty an d Pa i n R esea rc h L a b o r ato r y Ru-Rong Ji, PhD Human Affect and Pain Neuroscience Laboratory Katherine Martucci, PhD Mo l e c u l a r N eu r o bi o l ogy L a b o r ato r y Wei Yang, PhD N eu r o i n fl ammat i on an d C ogn i t i v e O ut c omes L a b o r ato r y Niccolò Terrando, PhD
Pain Research Laboratory Andrea Nackley, PhD 38 NEW GRANTS totaling $6.2
9
VA
BLUE PRINT 2022 | 19
MILES BERGER, MD, PHD DUKE ANESTHESIOLOGY
HONORSOCIETY
Departmental Research $100,000+
July 1, 2020—June 30, 2021
BASIC SCIENCES (CPOP/CTPM)
Satya Achanta
Interventional AnalgesiX, Inc.: $147,100
Intraganglionic Analgesic Adeno-Associated Virus (AAV) Gene Vector Optimization in Large Animals
Niccolò Terrando
Exalys Therapeutics, Inc.: $200,479
Test the Efficacy of Exalys Ep4 Antagonist to Prevent Neuroinflammation and Delirium in a Preclinical Model
National Institutes of Health: $322,620 Neurovascular Dysfunction in Delirium Superimposed on Dementia
David S. Warner
National Institutes of Health: $342,852 Integrated Training in Anesthesiology Research
CARDIOTHORACIC ANESTHESIOLOGY
Madhav Swaminathan
Sentien Biotechnologies, Inc.
Sentien SBI-101-02
Quark Pharmaceuticals, Inc. Quark 509
CRITICAL CARE MEDICINE
Paul Wischmeyer
Baxter Healthcare Corporation: $557,112
The PASTDUe Nutrition EcoSystem Project
Society of Critical Care Medicine: $100,000
REmotely Monitored, Mobile-Health High Intensity Interval Training After Critical Care (REMM-HIIT)
Fresenius Kabi AG: $130,000
Impact of SMOF Lipid on Clinical Outcomes Among Patients Receiving Total Parenteral Nutrition: An Interrupted Time Series Analysis
Raquel R. Bartz Blade Therapeutics BLADE
GENERAL, VASCULAR & TRANSPLANT ANESTHESIOLOGY
Heath G. Gasier
Office of Naval Research: $227,954
Effects of HBO2 on Skeletal Muscle Calcium Regulation and Mitochondrial Function
Richard Moon
Office of Naval Research: $414,169 Integrated Diaphragmatic Function, Chemosensitivity, Erythrocyte Gas Transport and Endurance in Exercising Divers
Naval Sea Systems Command: $361,919 Perfluoromethane to Reduce Decompression Sickness
PEDIATRIC ANESTHESIOLOGY
Brad M. Taicher
Medtronic, Inc. MDT20032 BTIGER
REGIONAL ANESTHESIOLOGY
David B. MacLeod
Medtronic, Inc.: $401,904 Medtronic Oliver Study
VETERANS AFFAIRS
ANESTHESIOLOGY SERVICE
Karthik Raghunathan
Merck & Co., Inc.: $362,121 Sugammadex versus Neostigmine in Laparoscopic Cholecystectomy
WOMEN’S ANESTHESIOLOGY
Ashraf S. Habib
Haisco-USA Pharmaceuticals, Inc. Covance HSK3486-304
Heron Therapeutics, Inc. Heron HTX-019-203
Heron Therapeutics, Inc. Heron HTX-011
Dave Warner was a strong advocate of physician-scientists. He believed that we need anesthesiologists who could make a curious observation in the operating room and then take it back to the lab to study it in depth. He also had a broad vision for anesthesiologist-scientists: he rejected the idea that “anesthesia research” needed to be focused on anesthetic drugs, practices or procedures. Rather, he believed that “anesthesia research” should be defined by whatever research questions interest us as anesthesiologists. Dave’s love of neuroscience and brain physiology was incredibly selfless - advances in these fields will help patients avoid neurologic deficits and incurable disease.
ALLAN FRIEDMAN, MD DUKE NEUROSURGERY
As a former neurosurgical resident, David Warner always had a special bond with the Department of Neurosurgery. Dr. Warner was recognized as an extraordinarily thoughtful anesthesiologist whose patient care was always guided by his in-depth knowledge of physiology and pharmacology. He was the “go to” guy when we had a patient with special anesthesia needs. Dr. Warner was the consummate physician-scientist and many of the neurosurgical faculty and residents collaborated with him on laboratory and clinical projects. He had a special ability to find solutions to clinical problems by exploring them in the lab. As a good friend to so many of us, his premature passing is mourned by the entire department.
ULRIKE HOFFMANN, MD, PHD DUKE ANESTHESIOLOGY ALUMNA
Dr. Warner was a true physician-scientist and neuroanesthesiologist at heart. His dedication to serve patients with neurologic injuries was unparalleled and complemented by his neverending scientific curiosity and mindset; he was a master physician and deeply caring doctor, exemplary for the next generations of physicians which he taught with such passion. He will be missed and forever remembered.
MICHAEL HAGLUND, MD, PHD, MED DUKE NEUROBIOLOGY
David was the consummate physician, teacher, investigator, and mentor. I worked with David throughout my career as the surgical director of the epilepsy center at Duke. He was always gracious and worked with me on the most difficult awake brain mapping cases for the surgical treatment of epilepsy. If I had an awake mapping case, I always was reassured when David was my neuroanesthesiologist. He always stayed until my patient was done with surgery no matter how late
20 | DUKE ANESTHESIOLOGY DEPARTMENTAL RESEARCH
IN REMEMBRANCE
the hour. He provided me countless hours of mentorship and I valued his opinion highly. I was more than blessed to have him as a colleague and more importantly, a dear friend.
BRADLEY HINDMAN, MD UNIVERSITY OF IOWA
In July 1988, I was assigned a bench in the Iowa neuroanesthesia research lab shared by David Warner and Mike Todd. Sometime that summer or fall, John D. (“Jack”) Michenfelder—an icon and credited by many as the father of modern neuroanesthesiology—came to Iowa as a visiting professor. I remember sitting (quietly) at the lab conference table, listening while Warner, Todd and Michenfelder discussed, and sometimes contentiously debated, contemporary neuroscience. I remember thinking all three were independent thinkers and were true “heavyweights.” I suggest Dr. Warner could be viewed as Michenfelder’s “successor,” continuing and advancing our specialty’s contribution to laboratory-based neuroscience research. Thank you, Dr. Warner.
DANIEL LASKOWITZ, MD DUKE NEUROLOGY
Dave was a mentor and friend to me since the day he arrived at Duke, and in a sea of academic cynicism, he was always a beacon of integrity. His values of training the next generation and multidisciplinary collaboration were not just words or corporate logos to Dave, he lived them. One of the truly exceptional things about Dave is that, not only was he absolutely committed to mentoring, he was always non-parochial; people came before departments or institutions. Dave’s biggest impact to this institution was his selflessness and commitment to do the right thing with regard to training and translational research. He truly stood for the human values that make this institution great.
MICHAEL TODD, MD
UNIVERSITY OF MINNESOTA
I first met Dave in San Francisco during an ASA Meeting. It was one of those immediate connections—to paraphrase Rick from Casablanca, “this was the beginning of a beautiful friendship.” The realization that there was someone at Iowa who shared my passion for neuroanesthesia and neurophysiology was easily a deciding factor to move there. Dave and I worked literally side-by-side (our desks were adjacent) for the next eight years—and our collaborative work continued for the rest of his life. Our last joint paper [“A Beautiful Friendship—and a Lesson about Friends and Colleagues: A Classic Partnership Revisited” in Anesthesiology] was published just after his death.
David S. Warner, MD
It is with profound sadness that we share with you the passing of a beloved member of our Duke Anesthesiology family, David S. Warner, MD, distinguished professor of anesthesiology. He passed away on December 5, 2021 at the age of 68.

An eminent leader in our field, Dr. Warner was one of the world’s most respected neuroanesthesiologists. He will be remembered as an extraordinary academician, physician, scientist, and mentor who dedicated his career to training the next generation in our specialty and to multidisciplinary collaboration. His life’s work focused on understanding the biology of acute central nervous system injury, with a focus on the development of preclinical models of human disease and therapeutics.
It’s often said that “we stand on the shoulders of giants;” Dr. Warner was unequivocally one of those giants, and we have endless gratitude for his immense contributions.
Read more at bit.ly/DSWRemembrance
Preserve his legacy. Your gifts to the David S. Warner Fund will help establish a professorship in his name at the Duke University School of Medicine. Give at anesthesiology.duke.edu

BLUE PRINT 2022 | 21 IN REMEMBRANCE
To preserve Dr. Machovec’s legacy at this institution, Duke Anesthesiology formally established the Kelly Machovec Humanism Award. The recipient of this annual award will exemplify grace and compassion in their delivery of patientcentered care, reverence for patients, their loved ones and colleagues, ethical principles, and a continuous commitment to clinical excellence.
IN REMEMBRANCE

Kelly Ann Machovec, MD, MPH
It is with profound sadness that we share with you the passing of a beloved member of our Duke Anesthesiology family, Kelly Ann Machovec, MD, MPH, an esteemed pediatric cardiac anesthesiologist. She passed away on March 30, 2022 at the age of 43.
She will be remembered as an exceptional academician and physician who dedicated her career to improving the lives of children undergoing cardiothoracic or vascular surgery, and for her special impact that was palpable to her colleagues and patients throughout the Duke Children’s Heart Center. Dr. Machovec’s research primarily focused on the hemostasis management of children following open heart surgery performed on cardiopulmonary bypass. She also advocated for pediatric health care on a global scale by taking part in medical missions in India, the Philippines and Haiti. Read more at bit.ly/KAMRemembrance

IN REMEMBRANCE
22 | DUKE ANESTHESIOLOGY
LAURA A. DOWNEY, MD EMORY UNIVERSITY
I had the pleasure of getting to know Dr. Machovec through our work together in the Congenital Cardiac Anesthesia Society. Her passion and enthusiasm for life, family, friends, and improving the care of children undergoing cardiac surgery was evident to anyone who knew her. She inspired so many people and will be greatly missed.
EDMUND JOOSTE, MD DUKE ANESTHESIOLOGY
Kelly was a friend, advocate, mentor, and colleague who always gave her all. She gave her mind to improve the lives of children with heart disease, her passions and energies for those with little, and her love and attention to all those around her. I will miss her energy, sharp wit and never-failing optimism. Her physical absence leaves a hole in our lives, but her remarkable legacy sustains us.
ALLISON ROSS, MD DUKE ANESTHESIOLOGY

Kelly was an amazing individual who was universally loved and respected by all she touched. She was not only an excellent clinician, but she dedicated her career to “doing the right thing” by advocating on behalf of patient rights. In addition to her noteworthy career accomplishments, she was also consistently kind to her colleagues and made the time to help others---always. The field of pediatric cardiac anesthesia will miss her achievements, but those of us who knew her well will miss her wicked sense of humor, her bright smile, and her ability to make everyone feel special. Her legacy will live on at Duke, and her presence will live on in the hearts of her pediatric work family. Miss you, my friend.
JENNIFER L. TURI, MD DUKE PEDIATRICS
Kelly was an amazingly kind and caring person. She approached everything she did, whether it was advocating for patients, teaching fellows, supporting colleagues, or living life to its fullest, with tremendous spirit and dedication. I feel very fortunate to have been her colleague and her friend. I miss her greatly.
Morpheus Perioperative Medicine Fellowship





Available Online http://morpheusconsortium.org/#fellowship morpheusconsortium.org • An immersive learning and network building experience • Learn from world renowned researchers and expert practitioners in the field • Designed for the practicing clinician • Customize your learning experience with an array of elective courses • Transform your career
91
Poster Abstracts
2022 WINNERS
Post Doc Basic Science Research (David S. Warner Award) Ravikanth Velagapudi
Fellow Clinical Research (Dick Smith Award) Rose Tang
Resident Research (Bill White Award)
Benjamin Andrew
Medical Student Research
Jake Thomas
CRNA/DNP/Grad/Undergrad Research
Eden Deng
Case Report
Trung Pham
Quality Improvement
Henry Lather
Celebrating Thirty Years of ACADEMIC EVENING

After two years of observing scholarly activity and scientific excellence on a virtual platform due to the COVID-19 pandemic, members of Duke Anesthesiology returned to gathering in-person this year to celebrate a special 30th anniversary of Academic Evening. Three decades since its inception, science and discovery have progressed, but the goal of the event has remained constant—to advance anesthesia, critical care and pain management which ultimately enhances patient care.
This year, a near record-breaking 91 poster abstracts—ranging from basic science, clinical trials and case reports—were submitted and showcased by juniorlevel investigators and faculty at Duke Anesthesiology’s 30th Annual Academic Evening, which took place on May 10 at the Millennium Hotel Durham.
“We were thrilled to be back in person and to watch all of our brilliant, innovative and talented colleagues presenting their research,” says Dr. Jeffrey Gadsden, event chair and associate professor of anesthesiology. “It’s truly humbling and inspiring to see the sheer talent and ideas that our department produces. It was especially gratifying to see how much research was carried out by trainees—these are busy residents and fellows with often grueling clinical schedules, and the fact that they are
mentored to prioritize clinical and basic science investigation while training is simply amazing.”
With his family in attendance, the late Dr. David S. Warner (who served as former event chair and vice chair for research) was honored during the evening not only for his key role in the event, but for the integral role he played in mentoring numerous investigators and advancing both basic science and clinical research within the department for nearly 30 years. Duke Anesthesiology chairman, Dr. Joseph Mathew, opened the evening by announcing the newlynamed David S. Warner Award for post doc basic science research and then ringing Warner’s bell, signifying the beginning of presentations.
DR. GEORGE MASHOUR, chair of the Department of Anesthesiology at the University of Michigan School of Medicine, served as this year’s guest judge. “I was extremely impressed by the breadth and depth of the research accomplishments—


Duke is clearly a top-tier academic anesthesiology department making major contributions to the field,” says Mashour. “It is exciting to see such a vibrant and thriving community of scholars in anesthesiology.” BP

24 | DUKE ANESTHESIOLOGY EDUCATION
Dr. Mathew ringing Dr. Warner’s bell during a moment of silence.
Dr. Warner ringing his bell at Academic Evening in 2018.
CONGRATULATIONS
TO OUR 2022 ABLE SCHOLARS
Creating a culture of coaching in which every faculty member is invested and engaged in professional growth.
The ABLE Program is designed to accelerate career development for junior faculty in their chosen pathway by pairing them in a one-year program with a personal coach. The program involves training in aspects of career development that include strategies to build resilience, enhance professional skills, and learn the infrastructure that supports their chosen domain.
The Supporting Mentorship in Anesthesia Research through Training (SMART) Program, a Duke Anesthesiology faculty development initiative, is designed to enhance mentorship capacity in the department by developing necessary skills in mentors through evidence-based training methods. The program began October 1, 2020.

2021-2022 SMART Class
Aurelio A. Alonso, DDS, MS, PhD
Warwick A. Ames, MBBS
Jeanna D. Blitz, MD, FASA

W. Jonathan Dunkman, MD
Sarada Eleswarpu, MD
Heath Gasier, PhD
Nicole R. Guinn, MD


Michael L. Kent, MD, MSQM
Evan Kharasch, MD, PhD



Negmeldeen Mamoun, MD, PhD
Michael W. Manning, MD, PhD

Grace C. McCarthy, MD
Abigail H. Melnick, MD
Andrea G. Nackley, PhD
Angela Pollak, MD
Jamie R. Privratsky, MD, PhD
Karthik Raghunathan, MBBS, MPH
Kevin Vorenkamp, MD, FASA
Kerri M. Wahl, MD, FRCP(C)
BLUE PRINT 2022 | 25
EDUCATION
Sandy An, MD, PhD
Amanda Faulkner, MD
Jon Andrews, MD Eric A. JohnBull, MD, MPH
Rachael Mintz-Cole, MD, PhD
Cameron Taylor, MD
Jonathan Dunkman, MD
EDUCATION OPERATIONS
CLINICAL RESEARCH
October 2022
Dear Friends,
Greetings to all of you. We continue to navigate new phases of the pandemic and figure out how to live with intermittent surges in COVID-19 cases. We have learned so much over the past two and a half years and are in a much better place with tools to manage the disease. Incredible advances have been made in a remarkably short time, and exciting new discoveries continue to emerge.
Among those efforts is ongoing research by Duke scientists to develop a universal COVID vaccine. That work has yielded significant progress to date, as researchers in the Duke Human Vaccine Institute have developed a pan-coronavirus vaccine that demonstrates protection against the current COVID-19 virus as well as variants and related coronaviruses in animal models. Clinical trials to further study the vaccine are expected to begin later this year or early in 2023. There has never been a time in our lives when the importance of biomedical science has been more clearly illustrated.
The COVID pandemic presented challenges unlike anything our school and our world have ever faced or anticipated. Here at Duke, our commitment to scientific discovery and patient care - addressing a broad spectrum of illnesses – never wavered and continues to play out in labs and clinics across our medical campus and beyond. And at every turn, Duke and School of Medicine faculty, students and staff have met the challenges with enormous skill and perseverance, as we continue to fulfill our missions of research, care, and education.
This year, the School of Medicine once again has been recognized nationally for our excellence. In February, we were ranked third for federal medical
research funding, with 10 of our departments ranked among the top 10 (Anesthesiology ranked 8th), as determined by the Blue Ridge Institute for Medical Research. And in March, we were ranked sixth among medical schools for research by U.S. News & World Report — with seven of our specialty programs placing in the top 10 (Anesthesiology ranked 3rd). These standings are a testament to the dedication and innovation of our faculty, staff, trainees, and students.
And the commitment of our physicians, providers and staff to work together to advance patient care has never been stronger. With innovation and collaboration, we are working to ensure that Duke Health will continue to provide the most advanced and accessible care for patients as well as provide sustained, long-term support for our academic mission, which includes educating our future health care providers and leading in scientific innovation and discovery – all of which are key priorities for all leading academic medical centers.
I am proud of the efforts of our entire School of Medicine community. As providers caring for patients, as researchers generating breakthrough discoveries, as innovators bringing new ideas to the health care market, and as educators passing knowledge and experience on to new generations, all are making a difference in the lives of our patients, our community members, and people throughout our nation and world.
With warm wishes,
Mary E. Klotman, MD
Dean, Duke University School of Medicine Vice Chancellor for Health Affairs, Duke University Chief Academic Officer, Duke University Health System

SCHOOL OF MEDICINE 2023 US News & World Report Rankings Best Medical Schools: Research DUKE UNIVERSITY SCHOOL OF MEDICINE Best Medical Schools: Anesthesiology DUKE ANESTHESIOLOGY #6 10 #3
26 | DUKE ANESTHESIOLOGY
Dr. Machovec Honored with Distinguished School of Medicine Awards

In March, a distinguished faculty committee at Duke selected Kelly Machovec, MD, MPH, as a recipient of the Leonard Tow Humanism in Medicine Award, recognizing her compassion in the delivery of care, respect for patients, their families and health care colleagues, as well as clinical excellence. The late Machovec (“In Remembrance,” page 22) was an esteemed pediatric cardiac anesthesiologist at the Duke Children’s Heart Center who joined Duke Anesthesiology faculty in 2013. Dr. Eddie Jooste, chief of the Pediatric Anesthesiology Division says, “Kelly led with her heart and was a fierce advocate for child-centered health care policies and her patients, whether they were here at Duke or on a mission trip.” “Everyone at Duke who had been touched by Kelly’s kindness,

ESTABLISHMENT of the William Maixner Professorship
fairness and unwavering ethics knows that there was no one more deserving of this honor,” says Dr. Allison Ross, former chief of the Pediatric Anesthesiology Division.
Before her passing, Machovec also received the Duke Pediatric and Congenital Heart Center Impact Award, recognizing her exceptional impact on the clinical practice around hemostasis, on both a local and national level. She is credited for discontinuing preoperative blood testing in children to prevent them from having painful, unnecessary blood draws in the preoperative clinic, which revolutionized the way blood products are ordered for children with congenital heart disease at Duke. Machovec also wrote the handbook of coagulation management for children coming off cardiopulmonary bypass. This led to her founding the Hemostasis Interest Group, a committee within the Congenital Cardiac Anesthesia Society.
This year, Duke Anesthesiology formally established the William Maixner Professorship at the Duke University School of Medicine. This highly-coveted, permanently named memorial preserves the legacy of the late Dr. William “Bill” Maixner, the Joannes H. Karis, MD, Professor of Anesthesiology – a world-renowned pioneer in pain research and one of the department’s most beloved and distinguished faculty. Maixner dedicated his life-long career to unraveling the mysteries of chronic pain and was committed to translating basic discoveries into novel diagnostics and treatments to positively impact research, education and patient care. This professorship honors his exceptional achievements, fuels scientific discovery, and invests in teaching and mentoring the next generation of leaders.
Duke Anesthesiology chairman, Dr. Joseph Mathew, announced in February that Dr. Ru-Rong Ji has been named the William Maixner Professor of Anesthesiology, recognizing his extraordinary scholarship in advancing science and improving human health. Ji serves as director of the Center for Translational Pain Medicine –internationally-recognized as a best-in-class translational pain medicine program, founded by Maixner.
Ji is one of:
Duke scientists named to the 2021 list, which includes
from more than
countries.
Dr. Ru-Rong Ji has once again been named among the most “Highly Cited Researchers” in the world. These pioneers in their fields represent the most influential researchers who have published multiple papers frequently cited by their peers that rank in the top one percent of citations for field and year in the Web of Science.

Duke Anesthesiology colleagues and members of the Maixner family gather for the William Maixner Professorship Dinner on February 11; right, Drs. Joseph Mathew and Ru-Rong Ji


BLUE PRINT 2022 | 27 SCHOOL OF MEDICINE
38
6,602 researchers
70

28 | DUKE ANESTHESIOLOGY
Dr. Jeanna Blitz Medical Director, Duke PASS Clinic
Forging the Path to Surgery and Recovery

PASS and POET’s Comprehensive Approach to Patient Preparation and Population Health
By JENNIFER BRINGLE and DR. JEANNA BLITZ
The weeks and months leading to surgery or an invasive procedure can be a pivotal time for many patients. Facing a new diagnosis and navigating multi ple health appointments can create additional demands upon a patient’s lifestyle that can feel overwhelming. Yet, achieving the best possible outcome often requires preparation that begins long before the day of surgery, and continues after it ends. Similar to the training required to succeed climbing a mountain, recovering from surgery requires physical and mental resilience and resource planning.
tions,” says Dr. Jeanna Blitz , medical director of the Duke PASS clinic. “We look to ensure each patient is ready for what they’re about to undertake—not just medically, but physically and psychologically, and we consider the impact that socioeconomic factors have upon patients’ outcomes.”
Led by a team of anesthesiologists, the Duke PASS clinic is the foundation for this comprehensive patient preparation program. The approach to chronic conditions within the perioperative period differs from the approach used in other clinical settings due to anticipated physiologic
Understanding the preoperative preparation each patient needs is the first step—and that’s the mission of the Duke Preoperative Anesthesia and Surgical Screening (PASS) clinic and its PeriOperative Enhancement Team (POET) Together, they form a unique perioperative and population health program, serving as a model for value-based, high-quality care both at Duke and on a national scale. The PASS-POET model, founded by Dr. Solomon Aronson, Duke Anesthesiology professor emeritus, has expanded the role of the anesthesiologist, fostering their increased involvement in care outside of the operating room.
“We take a holistic approach—we consider more than just the patients’ chronic condi
changes induced by surgery and anesthesia, the need for stricter therapeutic targets for glucose control, anemia, etc., and the accelerated time frame between initiation of the intervention and surgery. While other preoperative optimization clinics exist, they serve far fewer patients each year than are served by the PASS and POET programs, and often lack a population health-fo cused approach.
“When we’re thinking about this from the perioperative perspective, it’s often through a different lens that’s informed by our best specialists, but overlaid with our experience as the anesthesi ologist within the perioperative world,” says Blitz.
Established in 2018, the PASS clinic evaluates patients scheduled for surgery—both elective and
COVER STORY
BLUE PRINT 2022 | 29 ”You haven’t climbed the mountain until you’ve come back down.” PERIOPERATIVE MEDICINE:
time-sensitive procedures— to determine readiness for procedures that require anesthesia and pain manage ment. In a typical hospital setting, patients undergo a brief pre-admission testing (PAT) screening and are then advised to see a primary care doctor for medical “clearance” if a concern is identified. It’s a fragmented process in which delays may arise with either seeing the primary care provider, or the PAT clinic receiving the results of the consult. In this classic PAT model, once the patient receives “clearance” for their medical con ditions, they’re sent to surgery; thus, care coordination and post-discharge planning may be lacking or siloed. By contrast, the PASS and POET teams take a sys tems-based, collaborative and coordinated approach. Instead of viewing a medical clearance to proceed with surgery as the endpoint, they address and plan for the entire continuum of perioperative care from diagnosis to recovery, all within one patient-centered framework.
“You haven’t climbed the mountain until you’ve come back down,” says Blitz. “At Duke, our perioperative goals are different—it’s not enough to simply get the patient safely through surgery. Instead, we aim to achieve the best perioperative outcomes possible and to impact patients’ long-term health trajectories.”

PASS patients receive assessments via three channels, depending upon their perioperative needs: nurse phone screens, telehealth visits and inperson consultations. For more than half of the clinic’s patients—the healthiest individuals having low- to moderate risk procedures—the phone consultation is often the only step needed in the preoperative assessment process. But some patients, due to risk factors that can increase vulnerability to perioperative stress, require a more hands-on approach through an in-person consultation, which can include screening for frailty syndrome, cognitive assessment, lab work, and physical examination.
The PASS team also engages patients in shared decision-making conversations to explore the patient’s primary health goals for surgery and beyond. Given the increasing number of older adults and frail, medically complex patients undergoing surgery each year, these conversations are particularly important. This past year alone, the PASS clinic evaluated more than 20,000 patients age 65 years and older, performing cognitive screening on more than 8,500 of these older adults. Brain health is an important aspect of the anesthetic plan, which can impact risk of postoperative delirium and the development of neurocognitive disorders.
30 | DUKE ANESTHESIOLOGY
COVER STORY ANEMIA DIABETES NUTRITION REDESIGN of PASS CLINIC PENICILLIN ALLERGY 2015 2016 2016 2018 2018 PASS & POET Growth and Development PASS Clinic Data: 3 Pathways >50,000 assessments/year | >95% of all planned surgeries and procedures Telehealth In-Person ConsultNurse Phone Screen 23% 55% 22%
Of the more than 50,000 patients served by the PASS clinic each year, a subset of patients meet criteria for additional optimization programs, known as POET, designed to address at least one chronic medical condition prior to surgery. These interventions are provided by Duke’s multidisciplinary POET teams who, when combined, form a comprehensive preoperative optimization and population health program.
The Duke POET teams are condition-specific programs, tailored to support patients with achieving specific health goals to improve recovery and long-term health. These include quitting smoking, managing diabetes, and optimizing nutritional intake before surgery, among others. POET’s mission is to provide rapid access to Duke clinicians who are able to provide medical interventions within the accelerated timeframe of the preoperative period to achieve the best possible surgical outcomes—an approach requiring a distinct set of therapeutic goals and a specialized skillset.
“The overall model is a hub and spoke, where the hub is PASS, and the spokes are these optimization entities that branch off from it,” says Dr. Annemarie Thompson, professor of anesthesiology.

“The POET concept differentiates the preoperative care that we provide from most other top hospitals in the country,” says Blitz.
Since POET’s inception in 2015, Duke Anesthesiology has been the pioneer of population health interventions in the perioperative space. The first optimization clinic launch focused on anemia, with clinics supporting patients with diabetes, malnutrition, smoking cessation, allergy testing, pain, and sleep apnea soon following, and mental health
and pre-habilitation clinics planned for 2022.
The POET program has experienced growth year over year with regard to the number of distinct patients served, program expansion and the advent of new programs. To date, more than 11,000 distinct patients have been referred to at least one POET optimization team. While therapeutic goals differ by POET service, increasing the optimization window is a goal that’s shared program-wide.
Despite COVID-related changes to surgical workflows, the lead time between POET interventions and surgery has increased. Most patients are now receiving optimization interventions more than two weeks before surgery—an improvement due in part to a new approach by the POET nurse navigator, who proactively identifies potential POET candidates earlier in the preoperative process and follows patients through their care plans. POET services also allow for a more expedited process for surgical patients to receive preoperative care.
“It’s not your typical referral, because if you try to schedule a neurology appointment, you might have to wait three months, and that’s not keeping with the surgical timeline,” says Dr. Padma Gulur, director of pain management strategy and opioid surveillance at Duke University Health System. “So what we’ve created through these optimization clinics is more immediate access to care.”
Another way Duke takes a different approach
BLUE PRINT 2022 | 31 COVER STORY
The PASS-POET model has expanded the role of the anesthesiologist, fostering their increased involvement in care outside of the operating room.
SMOKING CESSATION SLEEP APNEA STRESS MANAGEMENT PREHABILITATION HEALTH DISPARITIES 2018 2019 2022 2022 2022
to preoperative patient preparation is with regard to scale. At Duke, the PASS clinic is the primary pipeline to all of the operating rooms and procedural suites, and provides the majority of all patient assessment and optimization services, serving more than 50,000 patients each year. There are many benefits of this approach to preoperative assessment, including the ability to streamline the patient preparation process to get patients from diagnosis to surgery date as efficiently as possible. It also allows for a standardized, equitable, and evidence-based approach to how medical conditions are managed preoperatively. Each day, the clinic provides around 250 assessments to patients from a variety of locations and backgrounds. Eighty-eight percent of PASS patients come from
period that we do face-to-face.” Thompson says the added benefit with expanded telehealth availability is the ability to reach patients sooner while also some times providing the bonus of affording a look into their home environment.
“Because we have a wide service radius of patients who come from far away to have their care specifically at Duke, telehealth allows us to reach them sooner than we would if they had to make the trip,” she says. “And when we see them on video, we get a sense of how they live, giving us a better snapshot into the en vironment they’re going home to after surgery, which can be very valuable.”
Telehealth, which has become more popular in general since the onset of the pandemic, has made a significant impact on appointment attendance for the PASS clinic. Since the addition of the telehealth track, the clinic’s no-show rate has dropped from 9.47 percent to 5.76 percent.
across the state of North Carolina— and 12 percent of patients come from out of state. Patients of all ages, genders, races, ethnicities, and socioeconomic backgrounds are represented in the PASS and POET populations (see graphic).
Since the onset of the COVID-19 pandemic, the PASS clinic’s tele health option has become more popular among patients. Telehealth consultations make up 22 percent of PASS assessments—offering a virtual look at factors such as physical and mental preparation for procedures, patient expectations and health goals, and support at home.
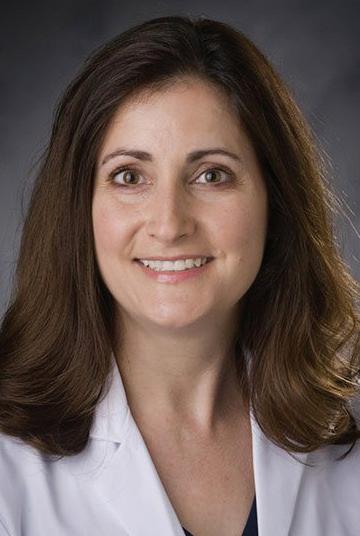
“There were a lot of opportunities in response to the pandemic that allowed us to greatly expand our telehealth option,” says Thompson. “The virtual visits are done as a consultation visit meant to address the same type of vulnerabilities within the perioperative
Telehealth has also helped the PASS team reach patients sooner—patients are scheduled for their PASS assessment within 24 hours of surgical case posting, compared to 3.5 days in 2019. The wait time for an appointment has dropped significantly, from 21 days in 2019 to six days in 2022. In spite of the addition of more elements of risk assessment to the evaluation, clinic efficiency has also improved— most patients complete their consultation in under an hour.


Additionally, telehealth has helped streamline the POET optimization process for some patients. With the accelerated expansion of telehealth, completed appointments increased from 1,736 in 2019 to 3,913 in 2021 with 60 percent of visits conducted via tele medicine platforms. Smoking cessation, nutrition, and diabetes programs saw the greatest telehealth-related growth.
According to Thompson, the penicillin allergy clinic has become an important part of POET’s mission to approach patient care from a population health perspective. She cites the prevalence of patients
32 | DUKE ANESTHESIOLOGY COVER STORY
Since POET’s inception, Duke Anesthesiology has been the pioneer of population health interventions in the perioperative space.
Dr. Padma Gulur
Dr. Annemarie Thompson
PASS Clinic Patient

who believe they have penicillin allergies learning they actually can tolerate the drug once they go through the allergy testing process prior to surgery. That can make a powerful tool in fighting infection suddenly available for that patient, which can reduce the risk of postop erative infection and avoid the use of other antibiotics during and after surgery.
“The more you use an antibiotic, the more likely you are to have community resistance when these organ isms emerge,” she says. “So there’s a compelling reason to know whether someone has a penicillin allergy for instance, because it’s a matter of using antibiotics wisely, and not using antibiotics that might generally be reserved for resistant infections. It’s about good antibiotic stewardship.”

The work of PASS and POET contributes to Duke’s overall population health-focused mission in the cost arena as well. Because preoperative care can reduce the amount of acute care and recovery time needed for many patients, it reduces both personal costs and the costs to the health system.
“The hospital is looking to move cases away from the use of acute care resources,” says Gulur. “That gets patients to recovery faster, leading to better outcomes and also reducing health care costs overall for both the patient and society as a whole.”
Over the years, PASS and POET have become a col laborative effort within the Duke Health system, with buy-in from not only anesthesia, but from surgery and nursing as well. Gulur says that willingness to work together across departments will allow the programs to continue to grow.
“There’s just so much potential to innovate in this space, to offer patients a chance to be their best before and after surgery, which is going to support better outcomes,” she says.

And looking back at how far they’ve come over the past seven years, Thompson says the team is not only excited for what’s to come, but also seeing the level of positive change they’ve achieved thus far.
“None of us ever want to go back to the time where you’d see a patient for the first time the night before or morning of surgery,” she says. “Being so rushed, you don’t get the whole picture or all the information you need that could potentially endanger the patient, or lead to a less than desirable outcome. So it’s important that people really understand the critical role that a highly functioning perioperative system plays in patient care.”
BLUE PRINT 2022 | 33
BP Caucasian 4% Not Reported 2.6% Asian
Demographics: 0.1% Unknown 45.1% Male 54.9% Female GENDER: LOCATION: ETHNICITY: 64% 23.6% African American 4.72% Hispanic 0.72% Native American/ Alaskan Native 0.11% Hawaiian/Pacific Islander 88% across North Carolina 12% out of state COVER STORY Demographics as of June 2022
FACULTY SPOTLIGHT
Whenever opportunity knocks, she says “yes” and opens the door. Elizabeth B. Malinzak, MD, says opportunity is everywhere, one just needs the vision to recognize it and the courage to go after it.
RATNA SWAMINATHAN
Her first recollection of aspiring to be a doctor goes back to age 3. Born and raised in Greensboro, NC, Malinzak grew up in an unconditionally supportive family, including a cardiac surgeon dad as a role model, a homemaker mom and two older brothers. They presented her with opportunities and hard work was not optional. After graduating in bioengineering magna cum laude at Rice University in Houston, Texas, she joined medical school at Duke University.
Her second-year anesthesiology rotation clinched her decision to work in an acute care setting. She found the specialty very procedural and hands-on, and loved the physiology and pharmacology aspects of it. She felt anesthesiologists were the “coolest and smartest doctors who knew the most about medicine and surgery.” After acquiring her MD in 2009, a residency in anesthesiology followed at Duke and pediatrics became Malinzak’s favorite subspecialty.
“It’s always a privilege to look after someone else’s child,” says Malinzak. She completed a pediatric anesthesiology fellowship at the University of North Carolina and returned to Duke in 2014 as an assistant professor in the Division of General, Vascular, and Transplant Anesthesiology, and joined the Division of Pediatric Anesthesiology in 2019.

34 | DUKE ANESTHESIOLOGY FACULTY SPOTLIGHT
SHAPING THE FUTURE OF ANESTHESIOLOGY

Her passionate advocacy in the diversity, equity and inclusion (DEI) sphere emerged from personal circumstance. When she became a mother during her CA-2 year, Malinzak realized that young physician mothers faced unique challenges as they sought to balance their professional and personal lives. Health care systems were structured in a manner that did not readily accommodate issues that young mothers faced. These challenges, she felt, either limited career advancement for some women, or placed a disproportionate burden on them for equivalent opportunities.

This dissonance in her orbit compelled her to educate herself on principles of gender equity and inclusion. Through networking with other anesthesiology moms across the country with similar experiences, Malinzak started advocacy efforts to address systemic biases and promote gender equity in professional organizations. She joined national societies, attended conferences, and developed several mentorship relationships nationally, in order to explore topics such as microaggressions and imposter syndromes.
There is something to be said about being in the right place at the right time. As part of the American
36 | DUKE ANESTHESIOLOGY
“In order to make our specialty engaging, we need to be a specialty that is inclusive and open to new ideas. We need to change the job description of the traditional anesthesiologist to capture the interest of the new generations in medicine.”
FACULTY SPOTLIGHT
Strategies for Advancing Advocacy
Determine your objective
Know your audience
your research
of compensation in starting positions, differentials in advancement criteria, and how cases are assigned in private practice.”
She also feels that Duke has an inspiring history of promoting women to leadership roles. At one point, seven of ten of the university’s deans were women. Furthermore, Malinzak takes pride in belonging to a department that has consistently recruited and supported women in medicine. “In the last five years, Drs. Joseph Mathew and Madhav Swaminathan have encouraged individual women in the department to seek out leadership development, apply for leadership positions and promotions, nominate for awards, and overall encourage them to their full potential. It’s great to see our leadership investing in women,” says Malinzak.
Focus on building relationships
Develop a strategy or plan
Be prepared to negotiate and revise, but don’t give up
“If you can see it, you can be it,” she explains how visibility in leadership is important to motivate junior and mid-career women. “Our department has women in leadership positions, including Cathy Kuhn as a designated institutional official, Nancy Knudsen as associate dean in the School of Medicine, Padma Gulur as executive vice chair, Annemarie Thompson as residency program director, Allison Ross as director of program development (and previous division chief), Miriam Treggiari as the vice chair for research, and several women as fellowship program directors (Brandi Bottiger, Jennifer Dominquez, Colleen Naglee).”
Society of Anesthesiologists’ (ASA) Committee on Women Anesthesiologists, Malinzak took on some high-profile steps to study pay parity. She was part of a workgroup that designed and deployed an extensive survey to assess racial and gender differences in compensation among anesthesiologists. The group’s findings of an 8% gender pay gap were published in Anesthesia and Analgesia in 2021.
Malinzak feels that people may have trouble understanding this difference in compensation. “A lot of biases start early on, such as pushing women into lower compensated subspecialties, differential levels

Malinzak has her finger firmly on the pulse of the younger generation of physicians and advocates for work-life equilibrium. “I think this generation really values work and life equally.” This is quite in contrast to mid to senior career anesthesiologists who had an “I work in order to live” philosophy, she observes. “It’s more about promoting wellness to have a more motivated workforce and not have them burn out,” she adds. “My message to get a good work-life balance is to recognize its fluidity and set priorities.”
Opportunely, in 2018 as vice chair of the Committee of Young Physicians, Malinzak co-authored the ASA “Statement on Personal Leave.” “Up until then, the ASA was the only medical specialty society without a statement on parental leave,” she informs.
BLUE PRINT 2022 | 37 FACULTY SPOTLIGHT
Do
How to Tailor Medical Education to the New Generations:
Ensure clear objectives and expectations:
• On personality questionnaires, they score high on perfectionism and rule-consciousness
• They expect specific performance standards and are goal-oriented to obtain these
Focus on personalized and experiential learning:
• They can listen or watch a recorded video lecture or podcast to learn traditional didactic information, and like to do so on their own schedule and in a place of their choosing
• When they attend in-person educational activities, they expect interactive and experiential learning through team and group-oriented approaches in order to apply the concepts of knowledge; otherwise it is not an efficient use of their time
Use technology:
• Millennials and the iGen have grown-up “tech-savvy” and are consumers of media
• They expect innovative technology, such as videos, podcasts, learning management systems, apps, social media, and simulators, to be used in their learning experience
Provide frequent assessment and feedback:
• They are used to frequent and multiple assessment, rather than a high-stakes end of unit exam, in order to gauge their progress
• They desire constant and immediate feedback on their performance to know they are on the right track
Provide coaching and mentoring:
• Consistent with the desire to assess their progress, they have lower self-reliance scores on personality questionnaires than previous generations
• They look to other people to help guide them along their path to their goals, such as coaches and mentors
The ASA-endorsed statement now supports six weeks of paid parental leave and recommends leave for medical and family issues to promote health and well-being of both women and men anesthesiologists at their workplaces and homes.
In 2020, Malinzak found herself fortuitously placed as chair of the Committee of Young Physicians to address another issue that had social media buzzing. It was a Facebook post about an anesthesiologist assistant whose job was threatened because she was pumping in the operating room. Then ASA president, Mary Dale Peterson, sought clarity on this important women’s issue and Malinzak and her team volunteered to gather evidence and develop an official statement on lactation.
“It was a tough road, some even thought it was gross to discuss lactation, but ultimately it was awesome when the ASA passed the ‘Statement on Lactation’ in 2021, making it the first medical society to have an official statement supporting lactation-related needs of women, including physicians, in the perioperative environment,” adds Malinzak.
Meanwhile, her efforts to extend outreach to promote a culture of inclusivity and diversity have gained national traction. “I am big on social media, especially Twitter, and have been able to make connections and collaborate,” says Malinzak.
Malinzak is the current president of Women in Anesthesiology (WIA), a national volunteer organization banding together to promote the professional and personal development of women anesthesiologists since 2015. “We can accomplish things through grassroots efforts in terms of advocacy,” informs Malinzak. In 2021, the ASA invited her to speak on the impact of COVID-19 on women anesthesiologists in North America at the World Congress of
38 | DUKE ANESTHESIOLOGY FACULTY SPOTLIGHT
Anesthesiologists, in which she addressed how the pandemic has exposed a flawed work-life dynamic that they experience.
At Duke, Malinzak brings her expertise and DEI message home to a diverse generation of medical students, residents and fellows. There is a push to encourage medical students, especially those underrepresented in medicine, to become more involved in anesthesiology, says Malinzak. “As a department, we hold skills workshops, promote shadowing by medical students and have a scholarship for visiting students.” Students shadowing or on a rotation are matched with advisors with whom they can identify and form a mentoring relationship. Malinzak spearheads a diversity initiative for the North Carolina Society of Anesthesiologists and is part of the American Board of Anesthesiology task force to examine the content outlines of exams to insure DEI principles are included.

As the director of Medical Student Education, Malinzak notes that the younger generation really likes interactive, experiential learning through actual case scenarios, clinical experiences, and with technology incorporated for attention. She says, “When they go to a lecture, they don’t want to be lectured to but want a discussion. I like teaching them in a way that they feel engaged and motivated. I want to give them the building blocks and then I want to see them make the skyscraper.”
Interestingly, Malinzak is known to have taken ‘hands on’ teaching to another level when she offered her own hand for a medical student to practice inserting an IV. Until recently, she was the course director of Maintenance of Certification in Anesthesiology, a simulation training course in anesthesia crisis management offered to physician anesthesiologists nationwide; she continues to teach medical students and residents principles of anesthesiology and crisis resource management through regular simulation using state-of-the-art technologies at the Duke Human Simulation and Patient Safety Center. “It’s a really good way of experiential learning in medical education and I believe exposure to it is very important for the progression of our trainees.”
Malinzak feels strongly about giving forward what she has abundantly received, namely mentorship from advisors, including Drs. Nancy Knudsen, Mark Stafford-Smith, Annemarie Thompson, Madhav Swaminathan, Edmund Jooste, Allison Ross, Padma Gulur and Joseph Mathew. “So, having someone who makes you believe you can do more is really big.
And if you fail, they’re the ones who can recognize that it wasn’t such a big deal.”
But it’s not all work and no play for Malinzak as she makes time for downtime with family. This spin-cycling neo-convert enjoys a good workout as much as she likes to regale her children, Patrick, 10, and Annette, 6, with stories about her being Sammy the Owl, mascot of Rice University. “They are my life, and I love shopping with them, going to their games, playing Nintendo Switch, or watching Star Wars together.” But come Saturday afternoon, it’s her tradition to dedicate two hours to nap time during which even their cute Cavachon puppy, Remy (short for remifentanil), lies low!
It’s true. Malinzak always say “yes” to opportunity, even if it means catching a few winks to refresh and recharge. It enables her to awaken to new possibilities. “There is always something exciting that can happen, so why not get up and enjoy that. Even when failure happens, I try to use that to make something better,” she says optimistically.
BP
BLUE PRINT 2022 | 39
“I want to give them the building blocks and then I want to see them make the skyscraper.”
By encouraging the entrepreneurial spirit, unfettered imagination, and unchecked ambition, the DREAM Campaign inspires Duke Anesthesiology faculty and provides them with the wherewithal to achieve the impossible. Together with our supporters, we are transforming the future of patient care.


Help us continue to train the leaders of tomorrow, develop the careers of our faculty, and protect quality of life for years to come.

Thank you to our valued 2021 donors
DREAM CAMPAIGN | ESTABLISHMENT of the WILLIAM MAIXNER PROFESSORSHIP | ESTABLISHMENT of the PAUL G. BARASH PROFESSORSHIP ESTABLISHMENT of the DAVID S. WARNER PROFESSORSHIP
Lauren Aguirre
Aurelio Alonso Warwick Ames Claire Anderson Adelle Anthony-Williams Debra Asai Laura Ashkin
Chakib Ayoub David Barash Jed Barash Norma Barash Karsten Bartels Verna Baughman Ashley Bell Jennifer Bennick Miles Berger Michael Berman Michael Block Marnee Bloomfield Richard Boortz-Marx John Borrelli Zeljko Bosnjak Clifford Breslow Randall Brewer Judi Bruckman Sorin Brull Benjamin Bunney James Bush, Jr. Marianne Cahalan Robert Calabrese
Lisbeysi Calo Daniel Carr James Caruso Emma Cataldi Anne Cherry Martin Cobern Jennifer Cohen Shaari Cohen Alexander Crean David Cullen Fellery De Lange Jennifer DiGiuseppe Lindsey Dimattina John Dombrowski David Donielson Christopher Donnelly
Joseph Donovan, III James Doughton Mahboubeh Eghbali-Webb Burton Epstein
Laura Evans Reine Fahed
James Feix
Jeffrey Feldman Cynthia Ferris Renee Flam Manuel Fontes
Elisabeth Fox Benevity Fund Pat Furman Gerald Gafka Francesca Galeffi Josephine Gambardella Brenda Gerhardt Jay Gewolb Ellen Goldberg
A. M. Goldkrand Robert Goldstein Sherry Gravatt William Greeley Stephen Greenberg Myrna Gross Enid Groves Padma Gulur Dhanesh Gupta Ashraf Habib Donna Hamilton Stephen Harris Jennifer Hauck
Lawrence Haynes
Ashley Hemmersbach James Taylor Herbert Donna Hersh
Roberta Hines
Fern Hosfeld Gloria Howard Richard Ing Denis Jablonka
Madeleine Jacobs
Michael “Lucas” James Ru-Rong Ji Christopher Jones
Edmund Jooste
Sven-Eric Jordt Ellen Kaiden
Zeev Kain
Tamara Kim Kathryn King David Klein Jordan Kornberg Jeff Kroes Stephen Kushins Donald Kuty Linda Kuty Arthur Lam Betty Laskowski William Lell Renee Lerner Robert Lesser Annie Liau Carl Lindskog William Locke Amanda Lodato AnneMarie Loftus David Louwsma Andrew Lutz John Lynch Kelly Machovec G. Burkhard Mackensen Nicholas Maginot Jean Maixner
Paul Maixner
Viravan Maixner Elizabeth Malinzak Negmeldeen Mamoun Inna Maranets
Michael Margolies Jonathan Mark Roberta Marowitz Daniel Martin Gavin Martin Benjamin Maslin Joseph Mathew David McDonagh Mary McDonnell Kathryn McGoldrick Stephanie McGuire James McKittrick
Deborah Meland
Abigail Melnick Blannie Miller Wendell Minor Jane Moon Richard Moon
Thomas Moore, II Cheryl Mulder Barbara Myers Andrea Nackley New Haven Neurosurgical Associates, P.C. Mark Newman Alina Nicoara Philip Noto
Robert Outtrim, Jr. Stephen Packer Chanannait Paisansathan Asit Patel Helen Pavilonis Dionne Peacher Max Perlmutt Patricia Petrozza Vincent Phillips Robin Pinsker Mihai Podgoreanu Jamie Privratsky Francis Quinn, Jr. Pamela Reis Christina Reiter
Teodulo Remandaban Linda Rice Jay Rinehouse Mary Rohe Leonardo Rosenfeld Jesse Rosenstein Allison Ross Cynthia Ryan Henry Samson Krista Sandt Sara Sapire Rebecca Schroeder Peter Schwartz Law Offices of David Seidman, P.C. Joseph Semo John Setaro
Richard Shaw
Leslie Sherwin
Bernard Siegel
Sheldon Silver Ellen Skinner Craig Sobolewski
Pardeep Sood Adam Sornchai Julie Sramcik
Mark Stafford-Smith Allison Stahl
Richard Stahl
Thomas Stanley, III Stanley Research Foundation Stephen Stein Sandra Stern Elsa Stone Kenneth Stone Shepard Stone Robert Strehlow Mike Su
Cephas Swamidoss Mahmood Tabatabai Jean Tabbal Don Tamis
Annemarie Thompson Matthew Thran Brian Titus Jo Travis
Jeffrey Wagner Carolyn Wallgren Willard Wallgren Barry Wallis
Shu-Ming Wang
Deryl Warner Rose Warner
Seth Warner Richard Watson
John Williams
Jessica Wolin
Richard Wolman
Wolters Kluwer Health Sandra Yee-Benedetto Francine Yudkowitz Erin Zenilman Abraham Zuskin

14 YEARS OF GIVING: DREAMCAMPAIGN.DUHS.DUKE.EDU
The Duke DREAM Campaign was established to support Duke Anesthesiology’s research programs and initiatives. As implied by our motto, we empower great minds to turn dreams into reality.
The DREAM Innovation Grant (DIG) supports innovative high-risk and potentially high-reward investigations to accelerate anesthesia and pain management research.

Duke DREAM Campaign Goals
Establish Endowed Professorships to invest in world-class faculty who would, in turn, secure extramural funding. Interest dollars from these endowments are to be used to support investigator salaries and provide them with the time and resources necessary to develop research programs.
Raise Funds to support research through the DREAM Innovation Grant, known as DIG.

Establish Philanthropic
Support as a long-term mechanism of limiting the adverse consequences of cyclical federal funding.
CAMPAIGN UPDATE
Chances are our research program has positively impacted your life.

$17M
of the DREAM Campaign and . . .
in DREAM Innovation Grants have led to more than . . .
in extramural funding received to-date
Read more about the campaign and make a gift! Visit:
42 | DUKE ANESTHESIOLOGY DREAM CAMPAIGN
$982,37414 Years
dreamcampaign.duhs.duke.edu
> >
INNOVATION GRANT
What is “DIG?”
The concept behind the DREAM Innovation Grant (DIG) – first launched in 2010 – is simple, yet brilliant. An annual competition is held among early to mid-career faculty members within Duke Anesthesiology, who do not have established NIH funding (past or present). Competitors submit their most innovative research ideas to a panel of judges for review. Proposals that demonstrate the perfect blend of ingenuity and practicality are selected, and winners are announced at the department’s annual alumni reception. DIG recipients can receive up to $40,000 in seed money for their innovative pilot studies, which ultimately help them apply for and obtain extramural funding. None of the funds awarded are to pay for faculty salary or overhead expenses. This grant creates an avenue for healthy competition among faculty, inspires ingenuity, promotes the careers of young physician investigators, enhances donor communication, and furthers the department’s academic mission. DIGs help to bridge the gap between training and progression to independent investigator status.
ELIGIBILITY:
Early to mid-career faculty members within Duke Anesthesiology, who do not have established NIH funding (past or present), are eligible to apply. One of the grants will be reserved to support a beginning scientist (within five years of completion of residency or fellowship or a PhD) by encouraging and adequately funding projects that can contribute to bridging the gap between training and progression to independent investigator status. The other award(s) will be used as a seed grant to help investigators obtain preliminary data to support a new application to the National Institutes of Health.

DIG IMPACT:
“The Dream Innovation Grant provided a unique opportunity for me to collaborate with surgeons in the Division of Metabolic and Weight Loss Surgery on a highrisk project to elucidate molecular mechanisms underlying comorbid chronic pain and obesity. This has been an incredibly productive partnership that yielded data for follow-on funding and represents a new, exciting direction for my research program.”
ANDREA NACKLEY, PHD: 2019 DIG RECIPIENT
DREAM INNOVATION GRANTS ARE FUNDED THROUGH A COMBINATION OF: Alumni Faculty Private Companies Private Donors

2021 TOP DONOR: Stanley Research Foundation:
$15K
DIG IMPACT:
“The DREAM Innovation Grant (DIG) played a crucial role in allowing our group to expand our research into cerebrospinal fluid (CSF) proteomics, a technique that is now a major focus of one of our current foundation grants and an additional NIH grant under review. ‘Omics technologies (ie, genomics, metabolomics, proteomics, etc.) are powerful ways to understand the biology underlying human disease, but one often needs preliminary ‘omics data using one of these methods in order to successfully get funded for a larger ‘omics study. This creates a chicken and egg situation – our DIG helped us move past this impasse by providing the funding we needed to gather the preliminary data to justify other grants.”
BLUE PRINT 2022 | 43
DREAM
MILES BERGER, MD, PHD: 2014 DIG RECIPIENT
Dr. Lisa M. Einhorn

BACKGROUND
MD: University of Maryland
Residency: Duke University
Fellowship: Pediatric Anesthesiology: Duke University
PILOT STUDY
“Pediatric Pain Optimization After Tonsillectomy: A Randomized Double Blind Methadone Pilot Study”
Pain in children remains a prevalent concern because it is often under-recognized and undertreated and has the potential to result in lifelong comorbidities. Evidence shows that untreated pediatric pain incurs a high risk for the subsequent development of persistent pain, disability and psychological disorders in adulthood. Approximately 20 percent of adult chronic pain patients report a history of poorly managed pain in childhood or adolescence. Currently, there is limited guidance from pediatric governing bodies for both intraoperative and postoperative care which results in haphazard approaches to analgesia.
Methadone is a cost effective, efficacious and long-acting opioid. A single intraoperative dose has been used safely in adult surgical populations and has been shown to reduce opioid consumption, decrease pain scores and increase patient satisfaction when compared with shorter acting opioids. Methadone use in pediatrics has been reported in clinical trials in patients having major surgery but has not been studied in routine pediatric surgeries. This has limited its generalizability for perioperative use in children.
The 2022 DIG will allow Dr. Lisa Einhorn to pursue a randomized pilot study examining intraoperative methadone use for pediatric tonsillectomy, a common procedure. The clinical trial will investigate methadone’s effect on postoperative opioid utilization and determine the optimal dose to be used in subsequent trials. This work will provide preliminary data for future grants to improve perioperative pain management for children.
44 | DUKE ANESTHESIOLOGY DREAM INNOVATION GRANTS
Dr. Shad B. Smith
BACKGROUND
PhD: McGill University (Canada)
PILOT STUDY
“Mechanisms of Genetic Regulation of Nociception and Injury Resilience by Mras”
Genetic factors substantially affect one’s risk of developing a chronic pain disorder, with potentially hundreds of genes contributing to common pain syndromes. Dr. Shad Smith’s lab investigates the genetic causes of chronic pain using genome-wide screens (known as GWAS) to identify novel risk factors for many such disorders in search of effective, non-addictive treatments for pain. His work with the OPPERA study culminated in a GWAS of temporomandibular disorders (TMD) incorporating data from more than 300,000 people. The principle finding from this study was a novel TMD risk gene MRAS, which codes for an important cellular signaling enzyme M-Ras. This gene was associated with healing and resilience against chronic pain via an undetermined mechanism that seems to be active in males only. The contribution of MRAS to pain-relevant pathways is an entirely unexplored area, making this a promising direction for target discovery, in addition to revealing a previously undetected sex dimorphism in nociception.
Smith will use his 2022 DIG to better understand the function of MRAS, conducting experiments to characterize the influence of M-Ras on neuronal pathways and establish a basis for future translational studies. The potential clinical utility of this discovery lies in determining the cellular mechanisms by which this gene promotes analgesia and/or healing in a patient who has suffered an injury or trauma - leveraging the body’s own potential to activate innate healing processes.

BLUE PRINT 2022 | 45 2022 RECIPIENTS
INNOVATIVE RESEARCH X INNOVATIVE 3
Providing state-of-the-art methodology for clinical, basic science and translational research empowers Duke Anesthesiology to explore revolutionary clinical inquiries by using innovative investigation methods.
Through significant research in neuroscience, molecular biology, molecular and human pharmacology endeavors, our team is making crucial advancements for patients worldwide.

46 | DUKE ANESTHESIOLOGY
Privratsky,
Michael Devinney,



Melissa E. Bauer,

MD, PhD RESEARCH: Blood-Brain Barrier Breakdown in Sleep Apnea and Postoperative Delirium Jamie
MD, PhD RESEARCH: Annexin A1-Mediated Mitochondrial Protection to Ameliorate Surgical Kidney Injury
DO RESEARCH: Large-Scale Implementation of Community Co-Led Maternal Sepsis Care Practices to Reduce Morbidity and Mortality from Maternal Infection BLUE PRINT 2022 | 47
Annexin A1-Mediated Mitochondrial Protection to Ameliorate Surgical Kidney Injury
 JAMIE PRIVRATSKY, MD, PHD
JAMIE PRIVRATSKY, MD, PHD
Acute kidney injury (AKI) is one of the most common forms of perioperative organ injury occurring in up to 30 percent of postsurgical patients, and it significantly increases morbidity and mortality. A number of vascular and transplant surgeries require interruption of blood flow to the kidney, rendering the kidney ischemic and causing significant metabolic stress. The timing of this kidney insult is known; thus, the possibility exists to intervene to protect the kidney. However, no treatment options exist to prevent or treat postsurgical AKI. The development of kidney protective therapeutics has the potential to greatly improve outcomes in the millions of people who undergo surgical operations and kidney transplants each year.
SPECIFIC AIM 1:
To determine the role of SIRT3 in ANXA1sp-mediated kidney tubule ATP production.
protectants that could limit postsurgical and transplant AKI holds considerable promise. Collaborators and previous Duke Anesthesiology Center for Perioperative Organ Protection (CPOP) investigators Zhiquan Zhang, PhD, and Qing Ma, PhD, developed a tripeptide fragment of the human annexin A1 molecule (AnxA1), termed ANXA1sp, which they showed had augmented protective properties against inflammation compared to
HYPOTHESIS: AnxA1 binds FPR2 in kidney tubular cells to upregulate SIRT3 through peroxisome proliferator-activated receptor gamma coactivator (PGC)1a, which allows for continued oxidative phosphorylation and ATP production.
The long-term goal of Dr. Jamie Privratsky’s laboratory is to develop kidney protective therapeutics to limit postoperative and critical illness AKI. One such therapy could be to limit mitochondrial stress as the kidney is particularly susceptible to mitochondrial stress due to its high metabolic demands. In fact, the kidney has the second highest mitochondrial content of all organs and mitochondrial dysfunction has been highly implicated in the pathogenesis of AKI. As such, the development of mitochondrial

SPECIFIC AIM 2:
To determine the role of mitochondrial necrosis in ANXA1sp-mediated kidney protection.
HYPOTHESIS: ANXA1sp upregulates SIRT3 to deacetylate CypD and limit mitochondrial necrosis to ameliorate kidney injury.
Vehicle ANXA1sp
DAPI 8 OHdG Citrate synthase
48 | DUKE ANESTHESIOLOGY INNOVATIVE RESEARCH
FIGURE 1: ANXA1sp-treated mice have lower levels of oxidative stress as measured by 8-OHdG staining (red) in kidney tissue sections.
ONGOING RESEARCH :
Determine the effects of Annexin A1 on mitochondrial function in myeloid cells and kidney tubular cells
Determine the receptor and signaling pathway through which Annexin A1 modulates mitochondrial protection
Determine the effects of cell-specific SIRT3 deletion on ischemic AKI
other AnxA1 mimetics. In collaboration with CPOP investigator Hagir Suliman, DVM, PhD, Privratsky’s new results reveal that unlike previous research that has shown anti-inflammatory properties of AnxA1 peptide mimetics, ANXA1sp ameliorates ischemic kidney injury in mice by limiting kidney tubular cell death and oxidative stress (Figure 1) and upregulates the mitochondrial protectant sirtuin-3 (SIRT3) (1). Despite the promise of ANXA1sp to limit ischemic kidney injury, the novel mechanism by which ANXA1sp could selectively augment SIRT3 expression and mitochondrial metabolism, and limit kidney cell death are not known Thus, the objectives of Privratsky’s newly-funded R01 grant are to determine the mechanism through which ANXA1sp augments mitochondrial function and metabolism and limits kidney tubular necrosis. Privratsky will pursue the specific aims ( page 48)
FIGURE 2: Proposed schematic for ANXA1spmediated kidney protection. ANXA1sp is hypothesized to increase ATP production and limit mitochondriallymediated cell death.

with the help of fellow Duke collaborators, Suliman, Sudarshan Rajogopal, MD, PhD, and Matthew Hirschey, PhD.
Once the work is completed, Privratsky will have defined the novel mechanisms through which ANXA1sp can augment mitochondrial function to limit postsurgical AKI, setting the stage for development of a novel line of mitochondrial protectants. The identification of mitochondrial protectants would not only limit postoperative and transplant AKI but also have broad implications for protection of other organs following surgery and transplantation. BP
FUNDING AWARDED: $1,610,000, FIVE-YEAR R01 GRANT
Funding Source: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
REFERENCES:
1. Suliman H, Ma Q, Zhang Z, Ren J, Morris BT, Crowley SD, Ulloa L, Privratsky JR. Annexin A1 Tripeptide Mimetic Increases Sirtuin-3 and Augments Mitochondrial Function to Limit Ischemic Kidney Injury. Front Physiol. 2021;12:683098. Epub 2021/07/20. doi: 10.3389/ fphys.2021.683098. PubMed PMID: 34276404; PMCID: PMC8281307.
BLUE PRINT 2022 | 49 INNOVATIVE RESEARCH
Large-Scale Implementation of Community Co-Led Maternal Sepsis Care Practices to Reduce Morbidity and Mortality from Maternal Infection
MELISSA E. BAUER, DO
The United States has the highest rate of maternal mortality of all developed nations. Maternal sepsis is one of the leading causes of maternal death in the United States. Most of these deaths are preventable and occur due to delays in recognition, treatment and escalation of care. Since 1987 when the Centers for Disease Control and Prevention started
are stark disparities in race and ethnicity of pregnant patients most affected by maternal sepsis.
This is one of the first studies to co-lead an initiative to improve maternal morbidity and mortality with community, birth equity and sepsis advocacy representatives, and maternal sepsis survivors to learn and apply perspectives not previously considered.
monitoring the causes of maternal deaths, there has been no noticeable improvement in the proportion of patients who died from sepsis. This is especially concerning since there have been overall advancements in sepsis care that have not transferred to care of pregnant patients. Additionally, there
This project partners community members with scientists each step of the way. First, the investigators composed a Maternal Sepsis Community Leadership Board of maternal sepsis survivors, sepsis advocates, birth equity advocates, and community members heavily invested in improving the health and equity of pregnant patients in their community, guided by Dr. Kendra Smith, community engagement expert. This community leadership board has an equal seat at the table providing input on the qualitative work, quantitative analysis and implementation of the maternal sepsis safety care bundle.
RESEARCH
CO-LEADERSHIP:
Community
Birth equity representatives
Sepsis advocacy representatives
Maternal sepsis survivors
Community engagement is crucial to advancing the science forward by having those most affected by sepsis and inequity provide input and guidance on what is best to improve care. Community involvement has been key in
INNOVATIVE RESEARCH
50 | DUKE ANESTHESIOLOGY
Clinician-scientists
the past few decades to improve the care for patients with Human Immunodeficiency Virus (HIV), provide outreach, and provide input on preventative feasible strategies that would be accepted in their own communities. This partnership between scientists and community members provides an invaluable opportunity to conduct science with feedback at each step from those with lived experience from sepsis, advocates for patients with sepsis, advocates to improve equity in care, and those living in the communities where we are working to improve care.
GRANT CO-AWARDEES:
Dr. Melissa E. Bauer
(contact PI)
Experience: 10+ years studying maternal sepsis
Credentials: Fellowships in both critical care and obstetric anesthesiology
Dr. Elliott Main (multiple PI)
Experience: Director for the California Maternal Quality Care Collaborative, a multidisciplinary team that has reduced maternal mortality by 50 percent in California with the implementation of safety care bundles
Initially, investigators will conduct qualitative interviews and focus groups to determine patient barriers to care and provider barriers to implementation. Their community partners will co-create the interview guides with their qualitative experts and receive feedback from implementation science experts and their Clinical Advisory Board. The themes obtained from the focus groups/interviews will allow the multidisciplinary team to determine how best to modify the sepsis safety care bundle to address these barriers. Next, investigators will validate the sepsis screening for maternal sepsis and explore diagnostic criteria for sepsis in pregnancy. The Community Leadership Board will provide input on the thresholds chosen. Investigators will negotiate a balance between not missing patients, but not having a high percentage of false positives. The goal is to not miss any patients, but also strike the balance between not having so many false positives that hospitals refuse to use the screening due to overuse of resources. Once investigators have identified themes from the qualitative work, the community leadership team and scientists will work with the implementation scientists to apply implementation strategies to address the
Credentials: Maternalfetal medicine specialist at Stanford University and chair for the California Maternal Mortality Committee
barriers and modify the sepsis safety bundle for racial/ethnic disparities and rural/urban hospital differences. Screening thresholds will be adjusted based on optimized sensitivity and specificity. The next phase of the grant is implementation across the states of California and Michigan. The modified bundle will be implemented and have modifications for community, rural, academic, and urban hospital settings. The barriers due to race/ethnicity, setting, socioeconomic status, will also have specific care plans for the bundle. Each hospital will be assigned a team of champions (doctors, nurses, community partners) to help with implementation barriers and provide expertise specifically for reducing disparities. Data flows from each state will be provided monthly for each region with
This work will dramatically expand the understanding of barriers to rapid treatment of infection to prevent progression to sepsis and implementation of maternal sepsis care practices from a patient perspective as well as from the clinician view. It will provide data to improve the criteria to more accurately diagnose sepsis and is a critical next step in the long-term goal of reducing maternal mortality and morbidity from sepsis.
specific data on outcomes stratified by race/ethnicity. This data will be evaluated and direct feedback provided with access to the team champions to provide strategies to improve care.
By treating community partners as equal members of the scientific team, investigators are making sure that equity is at the forefront of this work, with the end goal that this model serves as an example for other types of interventions to reduce maternal morbidity and mortality.
BP
FUNDING AWARDED: FIVE-YEAR PHASED GRANT: $1.6 million for initial 2 years, with potential $3.5 million for 3 additional years
Funding Source: Eunice Kennedy Shriver National Institute of Child Health and Human Development
INNOVATIVE RESEARCH
BLUE PRINT 2022 | 51
AIM 1: Determine the extent to which OSA severity is associated with preoperative BBB breakdown.

HYPOTHESIS:
Higher preoperative AHI values are associated with increased preoperative Qalbumin.
Characterizing Blood-Brain Barrier Breakdown in Sleep Apnea and Postoperative Delirium
MICHAEL DEVINNEY, MD, PHD
Up to 40 percent of the more than 19 million older Americans who undergo surgery each year will develop postoperative delirium, a fluctuating disturbance in attention and consciousness associated with increased one-year postoperative mortality, decreased quality of life, and increased long-term risk for Alzheimer’s disease (AD) and related dementias. Despite this substantial morbidity and mortality associated with postoperative delirium, there are few if any FDA-approved drugs to prevent it, largely because we still know very little about the underlying pathophysiology of delirium.
cognitive function and thereby contribute to delirium risk. Indeed, BBB breakdown occurs more often in patients with increased AD risk and is associated with increased AD neuropathology and accelerated cognitive decline. BBB permeability can be assessed by determining the CSF-to-serum ratio of large molecules like albumin (Qalbumin) that normally cannot cross the BBB and enter the brain. No prior study has determined whether postoperative BBB breakdown (i.e., increased Qalbumin) is associated with postoperative delirium.
AIM 2: Determine the extent to which BBB breakdown is associated with postoperative delirium severity.
HYPOTHESIS:
Increased 24-hour postoperative Qalbumin is associated with higher delirium severity scores.
Postoperative delirium may be caused in part by blood brain barrier (BBB) breakdown since 1) anesthesia/surgery are associated with BBB breakdown and 2) BBB breakdown has been associated with neuroinflammation, which has been linked to delirium after hip fracture and may underlie postoperative delirium. The BBB normally restricts diffusion of peripheral toxins and inflammatory mediators into the brain and cerebrospinal fluid (CSF). Postoperative BBB breakdown could allow these peripheral mediators to enter the brain, which could disrupt the neural connectivity necessary for normal
Conceptual model of relationships between obstructive sleep apnea, increased blood brain barrier breakdown (BBB), and postoperative delirium. Obstructive sleep apnea could increase BBB breakdown to predispose patients to postoperative delirium. Anesthesia/ surgery also can cause BBB breakdown to precipitate postoperative delirium.
BBB breakdown in older surgical patients (who are at risk of postoperative delirium) could also occur secondary to obstructive sleep apnea (OSA), a frequently undiagnosed disorder of repeated breathing interruptions (apneas and hypopneas) during sleep. OSA prevalence sharply increases with age, occurring in about 50 percent of older adults. OSA can be diagnosed with home sleep apnea tests, which determine the apnea-hypopnea index (AHI), a measure of OSA severity. OSA may contribute to postoperative delirium via BBB breakdown because 1) animal and in vitro models of OSA show BBB breakdown, and 2) patients with OSA have increased systemic inflammation, which can disrupt the capillary endothelial tight junctions necessary to maintain BBB integrity. Further, older OSA patients exhibit increased brain
52 | DUKE ANESTHESIOLOGY INNOVATIVE RESEARCH
parenchymal water, which could be caused by BBB breakdown. OSA has also been associated with increased risk of mild cognitive impairment, dementia due to AD and accelerated AD neuropathologic progression. These findings suggest that OSA-related BBB breakdown before and/or after surgery could play a role in causing delirium. However, no prior studies have determined whether patients with OSA actually have BBB breakdown (i.e., increased Qalbumin).
To test whether OSA patients exhibit BBB breakdown, and whether BBB breakdown is associated with postoperative delirium severity, Dr. Michael Devinney will measure Qalbumin in 201 non-cardiac surgery patients age ≥60 that completed an NIAfunded study, “Investigating NeuroinflammaTion Underlying postoperative brain connectIviTy changes (INTUIT).” These patients have already undergone pre- and postoperative blood/CSF sampling, cognitive testing and delirium severity assessments. Additionally, 101 patients completed home sleep
apnea testing in Devinney’s FAER-funded sub-study, “Sleep Apnea, Neuroinflammation, & cognitive Dysfunction Manifesting After Non-cardiac surgery (SANDMAN),” which aims to determine the extent that OSA is associated with neuroinflammation and postoperative cognitive dysfunction.
The completion of these studies will advance the understanding of the role of BBB breakdown (as measured by Qalbumin) in postoperative delirium. Further, Devinney will determine the extent that BBB breakdown occurs in OSA patients, which has implications for OSA-related cognitive dysfunction such as mild cognitive impairment and Alzheimer’s disease outside of surgery, and perioperatively for delirium and postoperative cognitive dysfunction. These findings could clarify overall mechanisms of OSA-related neurocognitive dysfunction and could help lead to the development of therapies to promote BBB integrity and prevent cognitive dysfunction and delirium in patients with OSA. BP
FUNDING AWARDED: $372,000, 2-YEAR COMBINED GRANT
Funding Sources: National Institute of Aging, Foundation for Anesthesia Education and Research
Potential mechanisms underlying perioperative neurocognitive disorders in sleep apnea patients.

BLUE PRINT 2022 | 53 INNOVATIVE RESEARCH
Devinney MJ, VanDusen KW, Kfouri JM, Avasarala P, Spector AR, Mathew JP, Berger M. The potential link between obstructive sleep apnea and postoperative neurocognitive disorders: current knowledge and possible mechanisms. Can J Anaesth. In Press.
Blogs from Abroad
GHANA

a Difference
Savion Johnson, MD RESIDENCY CLASS OF 2022
If there is one word to describe my experience, it would be perspective; in just one month in Ghana, I have seen a change in my perspective. The thing about perspective though, is that it normally does not change without encountering a difference of opinion
from Durham
forward. Whereas in Ghana, I am just a man, which makes me think back to the Civil Rights movement where my uncles held up “I am a Man” signs to signify their equality. Because of this dynamic, it has challenged me to think, when race is no longer at the forefront, what is it that defines you? What do you wrap your identity in? Is it faith? Your family? Your career? All questions I hope to continue to explore far beyond my time in Ghana.
CLINICAL IMPACT
I spent my time clinically at the Greater Accra Regional Hospital, a tertiary care center in Ghana, and I also taught anesthesia at the neighboring Ridge Hospital Nurse Anesthesia School.
think of our 80-hour maximum work week and taught me about true duty to your institution, your patients, and your community. It was inspiring.
When not in the operating room, I and my co-resident, Lori Jones, taught the first-year nurse anesthesia students on the basics of anesthesia, in preparation for their upcoming midterm exams. Some of these topics included physics, monitoring, capnography, and airway management. The opportunity to teach the nurse anesthesia students was incredibly rewarding as they were always very eager to learn, often skipping the opportunity to leave school early if that meant we could stay and teach after their other scheduled lectures were done for the day.
Drs. Adeyemi
Olufolabi, Savion Johnson, Lori Jones, and Cameron Taylor in Ghana.

or experience. As someone who had never stepped foot outside of the United States, my trip to Ghana as part of Duke Anesthesiology’s global health rotation allowed me to not only practice anesthesia 5,000 miles away, but also experience a new country for the first time, and it was truly eye-opening. In the United States, the first thing people notice is my skin tone, and race seemingly impacts every conversation moving
During our first week at Greater Accra, we found ourselves in the middle of a nurse anesthetist strike across the country, so we aided the nurse anesthetist on duty with cases in the obstetrics theater. One day when we came into the hospital, he let us know he had been at the hospital for four days straight, because there was no other anesthetist. When I asked him why he continued to show up, he said because there is no one else and he wanted to ensure nothing happened to the OB anesthesia program at Ridge and to ensure women received adequate care. This scenario made me
This experience highlighted so many things we take for granted in regards to our educational experience. One thing that stood out was access to the internet, as the school did not have WiFi. Another thing was lack of seating when all students were present, as there was one lecture we gave where two students shared a desk, which is a stark contrast to our large lecture halls here in the United States. Despite these challenges, the students were always very prepared and enthused about learning about anesthesia. When not teaching in the classroom, or assisting and teaching in the OR, we had the opportunity to interact with the CEO of the Greater Accra Hospital and the chair of the anesthesia department
54 | DUKE ANESTHESIOLOGY GLOBAL HEALTH
Making
5,365 Miles
and discuss perioperative outcomes and what could be implemented to improve them, especially in the critical care setting. It was intriguing to see things at a systems level, to see the challenges faced by the hospital, which included supply issues, blood product allocation and lack of welltrained staff. Despite these challenges, I left very impressed with the ingenuity of the anesthesiologist and nurse anesthetist in that they often utilized creative ways to facilitate good anesthesia care. My greatest takeaway from my time in Ghana was the people of Ghana and their spirit, one of resiliency and making a way when there seems like there is no way. My first global health experience was definitely a successful one and it has sparked my interest in continuing to be involved in global health efforts.
PERSONAL IMPACT
As I walked through the slave dungeons of Elmina Castle in Cape Coast, the first thing that came to mind were the screams of my ancestors, most who never even made it to the slave ships. The next thought was of all the events that had to take place for me to be standing here. Throughout my life, one word that many people have branded me with is resilience. I’ve demonstrated resilience in navigating housing insecurity, growing up in a home plagued by alcohol abuse and violence, and being a first-generation college graduate in order to become an anesthesiologist. But as I looked at the shackles and the “point of no return,” where slaves exited the dungeons before getting on the ships, there was a
Jones,
Traveling to Ghana for the first time with the dual purposes of (1) the provision of medical and educational services and (2) cultural, personal and spiritual exploration has been one of the most deeply impactful contributions to my personal and professional development to date.
Our days consisted of teaching first and second-year anesthetist students at the Ridge School of Anesthesia various topics in anesthesiology, followed by clinical time in the operating rooms at the nearby Greater Accra Regional Hospital (or, Ridge Hospital—a major




tertiary referral center). Currently in Ghana, there is a staggering shortage of qualified anesthesia care providers; for example, there were only two anesthesiologists practicing at Ridge Hospital at the time of our visit. This care gap is currently filled by nurse anesthetists, for now anyway, as Dr. Adeyemi Olufolabi and Kybele Inc. actively work to fill this by recruiting medical students for an anesthesiology residency program at Ridge Hospital. Thus, the education of nurse anesthetist students is vital to the safe practice of anesthesia care.
realization that what I experienced pales in comparison to anything my ancestors survived. It challenges me to want to do more, to be better, and to strive for greater than whatever I can currently imagine.
Co-resident Dr. Savion Johnson and I tailored our lectures to the fundamentals of providing safe anesthesia care, with particular attention paid to “Standards of Monitoring in Anesthesia”—oftentimes devoting an entire lecture period to each of the monitoring standards (pulse
GLOBAL HEALTH
BLUE PRINT 2022 | 55 Lori
MD RESIDENCY CLASS OF 2022
“
oximetry, ECG, end-tidal capnography interpretation, etc.). Our goal was to instill into our students that timely recognition and management of any change in the patient’s condition can truly be lifesaving, and to empower them with the basic knowledge necessary to be able to do so.
To be able to utilize the skills and knowledge that I have gained as a Duke Anesthesiology resident to teach the students and those in current practice (and, thereby to impact the care of patients in real-time and in the future) was deeply humbling. The knowledge that I can walk into a hospital on another continent and respond to emergency situations reflexively while having my expertise be deferred to by those around me has deepened my trust in my training.
When we were not in the classroom or operating rooms, we explored the incredible art, food, landscape, and history that surrounded us—traveling
to art galleries and markets, exploring the rainforest at Kakum National Park, visiting Elmina Castle (the last stop for many enslaved Africans before being brought to the colonies), and sipping fresh coconut water (and I mean, machete-the-top-off-a-coconut-and-popa-straw-in-it fresh) while lounging on the beach next to the crystal clear waters of the Atlantic coast.
The profoundness of the entire experience to me as an African American woman physician descended from enslaved peoples who may very well have been held at Elmina, cannot be understated. I will forever be grateful to the department, my program director, and the global health rotation director for the opportunity to include this experience in my training.
Cameron R. Taylor, MD FACULTY
Thank you” simply is not enough for me to say to Dr. Adeyemi Olufolabi for allowing me to share this incredible experience—my first encounter with global health!
I had the opportunity to teach the anesthesia students at Ridge Hospital in Accra about various topics in obstetric anesthesia. They were eager, curious and anxious to receive instruction. I also was able to spend some time working in their operating theaters observing both obstetric and general surgeries with relatively limited resources. At one point, we had to use a hot water bath from a thermos to thaw two units of FFP to be given to a mother during a hemorrhage, while the patient’s husband went to try and convince family members to donate their blood to her. Overall, the staff
were interested in our techniques and the clinical management of patients, and everyone was polite and receptive to our presence.

During the trip, we also visited local art museums, markets and historic sites, including Kakum National Park and Elmina Castle. We squeezed so much into a relatively short time window, providing an efficient overview of this west African nation.

It is difficult to describe how impactful traveling to Ghana was for me. It certainly provided me a new framework to approach my day-to-day and understand what can be done even when the most modern equipment is not readily available. It was a beautiful culture made of beautiful people. Any faculty who have ever considered a trip like this should seize the opportunity—you won’t regret it. BP

56 | DUKE ANESTHESIOLOGY GLOBAL HEALTH





Visit tinyurl.com/DukeGlobal — Adeyemi J. Olufolabi MBBS, DCH, FRCA Professor of Anesthesiology Affiliate, Duke Global Health Institute Senior Advisor, Anesthesiology Inclusivity Committee WHERE DO YOU WA N T T O CH A NGE LIVE S? Duke Anesthesiology Global Health Program “We have a role to play in global health to make the world a better place.”
Our Residents

58 | DUKE RESIDENCY RECAP
Class of 2022

PRINT 2022 | 59 RESIDENCY RECAP
Daisy Ogede, MD | CA-1

I was born in Nigeria and raised in Chicago, Illinois. I studied neuroscience and anthropology at Washington University in St. Louis. In addition to my pre-medical coursework, my undergraduate career largely consisted of being a track and field athlete. I was fortunate to have a very successful track and field career that I attribute to my stellar teammates and coaches. The lesson I learned as an athlete is “iron sharpens iron.” It is valuable in the life-long journey of learning to surround yourself with people with diverse backgrounds and skillsets.
What led me to anesthesiology was how the field affords me the opportunity to engage with the sickest of patients whose medical illnesses require operative treatment. I appreciate the wide breadth and complexity of cases. I am drawn to the brief, but intense connections made with patients and their loved ones. Additionally, I enjoy the close collaboration with surgical teams, nursing, and other ancillary staff, thus requiring excellent teamwork.
Residency has revealed the inner strength I have within and the invaluable community that is created amongst my colleagues.
I chose Duke Anesthesiology because Duke provides well-rounded training not only in general anesthesiology, but also its subspecialties. Additionally, I believed that the residents not only enjoyed working together, but also bonding and building friendships with each other. I felt that my unique background and talents would be welcomed at Duke.
Despite the long hours spent in the hospital, I believe residency has been a deeply rewarding journey so far. Entering residency, I expected to sharpen and broaden my clinical knowledge and skills. However, what surprised me the most was how I have grown as an individual. Residency has revealed the inner strength I have within and the invaluable community that is created amongst my colleagues. The biggest lesson I have learned thus far is how important it is to lean into a community inside and outside of the hospital. Finding ways to keep in touch with the hobbies and passions that do not involve being a resident physician. In conclusion, I look forward to seeing how the next several years will shape the woman and physician I will become.
resident spotlight
George “Bert” Cortina, MD, PhD | CA-2
During my undergraduate education, I realized I was interested in medicine and engineering. My dual interest led to a computer science major with an eventual goal of using these skills as a physician-scientist. My MD-PhD training allowed me to develop my basic science and medical skills as well as my engineering and applied science skills. In graduate school, I integrated these interests by developing a biophysical model that can predict antibiotic resistance. For a while, I struggled to identify which specialty I might be best able to apply my dual interest. It was during my medical school rotation in anesthesiology that it all clicked. More than any other medical specialty, anesthesiology uses engineering approaches in the care of patients. Throughout my training, Duke faculty have shown genuine interest in both my goals and development. Their passion, along with that of my fellow residents, has further motivated me to work hard and learn. Now in my CA-2 year, I am even more convinced of having made the right choice to train at Duke Anesthesiology.

I am an outdoor enthusiast. My favorite activities are running, swimming, mountain biking, and going on hikes along North Carolina’s beautiful Blue Ridge Mountains. Durham is the ideal location, offering easy access to numerous nearby biking and running trails. Additionally, lakes, mountains and ocean beaches are only a short drive away.
There is so much to learn in the field of anesthesiology. This is both remarkably exciting and humbling. The most exciting part of residency is learning something new with a senior resident or faculty mentor and then working to improve my technique in subsequent cases. I have witnessed the importance of communication and the teamwork involved with every procedure. My favorite cases have required both the surgery and anesthesiology teams to be in sync. These experiences, along with my relationships with my fellow residents and mentors at Duke, are motivating and encouraging.
60 | DUKE ANESTHESIOLOGY RESIDENCY RECAP
Throughout my training, Duke faculty have shown genuine interest in both my goals and development.
Match Class of 2026
















RESIDENCY RECAP BLUE PRINT 2022 | 61
Rick Bagott University of Texas, Houston
Sujatha Cumaran Trinity School of Medicine
Amanda Boornazian Baylor College of Medicine
Paul Moiseyev Case Western Reserve University
Brendan Garbe University of Florida
Alexis O’keiffe Howard University
Natasha Navejar Baylor College of Medicine
Theresa Rizk Duke University
Kayla Pfaff Ohio University
Kierstyn Sandwell Des Moines University
Sophia Sourlis Medical University of South Carolina
Sophia Toles Rutgers University
Ashley Vincent Rutgers University
Stefana Voicu Dartmouth University
Derek Woodruff University of Utah
alumnishoutout
with Drs. Sarah Cotter and Delbert Lamb
Sarah Cotter, MD ’19

Where are you now? After residency, I completed an adult cardiothoracic anesthesiology fellowship at Brigham & Women’s Hospital and am now an assistant professor of anesthesia at University of California, San Francisco.

How has your training at Duke Anesthesiology accelerated your practice of anesthesiology? I loved being at Duke, and that feeling has only solidified since leaving. I learned from the very best and have felt well-prepared for the challenges of fellowship and new attendinghood. Best of all, the Duke community is global, and I’ve been able to feel at home even in new places.
How did your training prepare you for being an anesthesiologist in a pandemic? There was simply no preparing for what COVID meant for our specialty, but I do think the attitude of “all hands on deck,” which is fostered during residency at Duke Anesthesiology as classmates grow very close, allowed my colleagues and I to mobilize and offer all we could to help in the midst of an incredibly difficult (and ongoing) crisis.
What is your greatest takeaway over the past few years? It is an absolute privilege to do the work we do. And, it is also important to rest.
What are the greatest lessons that you took with you from the Duke Anesthesiology Residency Program and Duke in general? Having now worked closely with residents (and as a trainee) at a couple of different institutions, I can say without a doubt that Duke offers a combination of rigorous clinical training and protected time to enjoy life outside of the hospital that is unmatched. This is on purpose, and has been carefully cultivated by the residency program leadership. There is a lot going on behind the scenes that you can’t appreciate until you graduate, but I remain so thankful to Annemarie and the rest of the educational folks for an
experience that encouraged growth not just as a physician, but as a person - a friend, a colleague, a family member.
What do you miss the most about Duke/Duke Anesthesiology? The people! And, Friday morning Elmo’s trips after a week of night float.
Advice for residents graduating from our program? Carve out time to remain connected with your Duke family. Wherever you want to go, there will be someone there who is a former Dukie. These relationships will be incredibly important in crafting your career.
Why did you choose anesthesiology as your specialty? I picked cardiac because many of my mentors were cardiac anesthesiologists, and I wanted (still want) to be like them when I grow up. I have a strong sense of pride in feeling like I can take care of the sickest patients on any given day. Overnight transplants don’t get easier (and it’s a lot harder to catch up on sleep with a one-year-old), but there is a deep feeling of gratitude when you’re the one who gets to care for a patient getting a second chance at life. This is a sacred part of what we do. BP
Delbert Lamb, MD ’20
Where are you now? After residency, I completed a pediatric anesthesiology fellowship at Boston Children’s Hospital, where I’m doing additional training in a pediatric cardiac anesthesiology fellowship and will stay on as faculty to care for cardiac/non-cardiac pediatric patients perioperatively.
How has your training at Duke Anesthesiology accelerated your practice of anesthesiology? Duke Anesthesiology really prepares you for the transition to excel in fellowship or to go straight into clinical practice. The large case volume allows residents the ability to care for the bread-and-butter cases to complex/ASA4 cases. CA-3s gain a lot of leadership experience (running the board/OR on senior night call, supervising junior residents and CRNAs, etc.), which allows Duke Anesthesiology residents to be more than prepared for whatever route they take after residency.
What are the greatest lessons that you took with you from the Duke Anesthesiology Residency Program and Duke in general? Remember what matters – know, listen and understand your patients, and remember that your duty is to take excellent care of the patient. Build your community. Establish friendships, trust and a sense of community with your colleagues. Be an advocate and a leader - for your patients, yourself, your colleagues, and your profession. Do your best.
62 | DUKE ANESTHESIOLOGY RESIDENCY RECAP
What do you miss the most about Duke/Duke Anesthesiology? Easiest question I’ve had to answer so far – the people. I came to Durham not knowing anybody, but I left with lasting friendships and family for the rest of my life. Starting from leadership, you have Dr. Joseph Mathew and Dr. Annemarie Thompson (AMT) who support, advocate and allow you to grow. AMT is the most passionate resident advocate I can think of and has remained a close friend and mentor. The faculty are always available for questions, support and mentorship, even after you have graduated from residency. And lastly, my co-residents are some of my favorite people I have ever met and those relationships will last a lifetime.
Advice for residents graduating from our program? Stay true to yourself. Be kind, keep learning and continue to do good in this world.
Why did you choose anesthesiology as your specialty? I enjoyed almost every medical specialty during medical school, but when I rotated with anesthesiologists, I was very quick to realize that they are exactly the type of physician I wanted to be like. They were calm, intelligent and remained so even under times of incredible pressure/stress. Now, I couldn’t imagine doing anything else.
We are quite spoiled at Duke Anesthesiology with excellent clinicians in every subspecialty of anesthesia, but I truly felt with ‘my people’ when I rotated on pediatric anesthesiology. Being able to take care of the tiniest babies to complex congenital cardiac patients is quite fulfilling, but also being able to calm and gain the trust from families is a huge responsibility. I love going to work each day, not only taking care of complex pediatric patients, but also learning and teaching with learners. BP
DR. ANNEMARIE THOMPSON Director, Residency Program

 DR. BRIAN COLIN Associate Director, Residency Program
DR. BRIAN COLIN Associate Director, Residency Program

new& noteworthy
Find us on Twitter!
Follow the new Duke Anesthesiology Residency-Run Twitter Page @DukeAnesRes or #DukeAnesRes
Keep in touch!
Doximity rankings
For 2021-2022: #1 in the South #1 in North Carolina #5 National Reputation
Update your alumni profile today: bit.ly/DukeAnesAlumni
BLUE PRINT 2022 | 63 RESIDENCY RECAP
“When you look at the trajectory of any academic institution, the strength of the residency is a key factor in departmental success. They are future faculty, clinicians, researchers, and leaders. Our charge is to prepare them to be lifelong learners, adaptive leaders and outstanding clinicians.”
60 100%22 2 9
DR. ANGELA POLLAK Assistant Director, Residency Program
Q&A
Dr. Laura Niklason is an internationally-renowned physician-scientist whose groundbreak ing research in vascular and lung tissue engineering led her to become a world leader in regener ative medicine. At Humacyte, she uses scalable platform technology to develop and manufacture universally-implantable bioengineered human tissues, intended to mimic key aspects of human physiology, to transform the practice of medicine and improve patients’ lives. We asked her to reflect on her career and time at Duke.
Q: Why anesthesiology?
A: I felt this was the right clinical patient population for me and it allowed me to split my time between science and medicine.
Q: What were your biggest takeaways from your time at Duke Anesthesiology/Duke?
A: As a young physician trying to develop my career, I was living in two fairly independent worlds - teaching courses in biomedical engineering and rounding in the ICU in anesthesiology. It took me time, but I learned how to prioritize and how to say “no” to certain opportunities because otherwise you get pulled in too many directions. In science and medicine, we’re all smart, hardworking people; so if you’re going to work hard, you might as well focus on what you really enjoy and what you are uniquely qualified to do - I’ve used that thought process as a guide post early on.
Q: What is your fondest memory from your time at Duke?
A: My fondest memories are of working in the ICU. It was stimulating and exhilarating to take care of patients who were very ill, in collaboration with really smart colleagues, and sometimes make a difference in the trajectory of the patient.
Q: Key lessons from your leadership roles?
A: During my time in the ICU and the OR, in particular at Duke, the ability to make important decisions with almost always limited information is a skill that I learned and have carried forward ever since. A really important aspect of leadership is a tolerance to risk; being able to operate in a situation where you don’t have perfect knowledge of everything, but you have to make a decision and be comfortable with it. I think that is one of the most critical things that I took away from my time at Duke and applied at both Yale and Humacyte.
Q: What was your drive to serve as a vice chair for research at Yale?
A: I was recruited to Yale to enhance the pipeline for physicians interested in research in anesthesia. I was passionate about creating a specialized research track that begins in the CA-1 year, similar to the ACES Program at Duke Anesthesiology. I had a running start in research when I joined Duke, but not everyone has that advantage, so I wanted to create a pathway where young investigators would be successful.
Q: Advice for young physician-scientists looking to navigate the research environment?
A: There can be pressure to work on what is fashionable or trendy, but I’ve always been an advocate for focusing on what you like and what is important. It is less important to, for example, stay narrowly within the purview of what is considered to be anesthesiology. I suggest to find mentors outside of your department and in different specialties – so long as there is some tie to that specialty and it is clinically relevant. Another critical step is to focus on the selection of your questions; ask questions that are both important and tractable.
Q: What are some critical steps in advancing science in general?
A: A willingness to cross boundaries between disciplines. Ensuring that young scientists are well trained in the basics and fundamentals of at least one discipline, so that they may fruitfully collaborate with other disciplines.
Q: What are key qualities of a good mentor?
A: Having someone who is willing to give you their honest, straightforward advice and wants to build you up, but is not intimidated by their trainees, are important traits in a mentor in any stage of your career. And, having more than one
64 | DUKE ANESTHESIOLOGY ALUMNI NOTES
person to go to for advice is incredibly important.
Mentorship is also partly about how the trainee approaches it; don’t be afraid to “bother” those in senior roles - people love to be asked what they think and generally want to help other folks.
Q: Did you have mentorship through the Humacyte startup process?
A: My then chairman, Dr. Mark Newman, and other entrepreneurs gave me advice about how to balance my time; a lot of advice was along the lines of things will take longer than you think and cost more than you think. An important lesson for me was finding patient investors. Starting a company as an academic – there is not one single road and each route is different.
Q: How did you choose the industry vs. academic path?
A: I made a conscious decision to not start a company until I had tenure at Duke. By that time, I had been NIH-funded on this research for about 10 years. I could see the potential path of my vascular engineering work turning into a clinical product. But NIH’s mission is to fund high-risk new research, not to develop products to be tested in patients. So, you have to make that jump in realizing this is no longer just a research project, but a product to develop for patients. At Humacyte, we had to spend $40 to $50 million just to get to our first patient. It is a completely different order of magnitude in terms of the number of people, the good manufacturing practices – all of the components that you need; the NIH just doesn’t fund at that level.
1998
Joined Duke Anesthesiology/ Biomedical Engineering/ Surgery faculty
2004
Co-Founded biotechnology company, Humacyte

2006
Joined Yale faculty (division chief, vice chair, adjunct professor)
2010 Engineered whole lung tissue capable of exchanging gas, one of the top 50 most important inventions of 2010 by Time magazine
BLUE PRINT 2022 | 65
Left to right: Humacyte manufacturing space, HAV implant (not in-human) and HAV green stain (collagen in the HAV wall).

Q: How should one partner with industry to get a project up and going?
A: One of the common ways is to start your own company, which is what I did; I knew that we had to specifically do this ourselves. But there are many instances where companies are doing similar things to your research, so partnering with a company could be another route. But in that case, the academician would need a patent that is already filed. You need something in your hand that you can bring to the company that has value.
Blue Stain: Nuclei of cells that have infiltrated the HAV wall. Red Stain: Contractile protein in the cells, showing the cell type in the HAV wall.
money. Researchers and investors may not see eyeto-eye on the importance of publishing results. And, when you partner with a company, you lose a large fraction of the control on how things move forward, so you just have to keep your eyes open about that.
The bottom line, if you partner with a company, the chances are you make it to market and then you’ll have a pie, but you won’t have all of that pie, you’ll have a quarter of that pie. But if you don’t partner and you don’t start your own company, than the chances are there will be no pie. So, it is just a matter of how you think about pie.
Q: What attracted you to regenerative medicine?
A: Regenerative medicine, even now but certainly in the 1990s, was a new field. It was not populated by a large number of scientists, so it was possible to make a big impact. This is still true.
Q: What are the advantages and disadvantages of partnering with industry?
A: Industry offers a lot of resources, especially if they have products already on the market. The amount of money they can bring to bear on a problem can be impressive and if the speed for product development depends on how much rocket fuel (money) you have, than it can be incredibly accelerating. The downside is companies have their own motivations – they want to make products, sell them in the marketplace and make
2013 Humacyte achieved first human surgical implantation of human acellular vessels (HAV) at Duke University

2014
Q: How is Humacyte achieving its mission of “transforming the practice of medicine?”
A: Humacyte is actively pursuing clinical trials in a range of applications: end-stage renal failure, vascular trauma, and peripheral vascular disease. By showing the utility of the human acellular vessel (HAV) in multiple settings, we hope to show that our technology has broad applicability.

2015
Humacyte HAVs received FDA’s Fast Track designation for vascular access for performing hemodialysis; Inducted into National Academy of Inventors
Elected to National Academy of Medicine; Named the Nicholas M. Greene Professor of Anesthesiology and Biomedical Engineering at Yale
66 | DUKE ANESTHESIOLOGY
“As an anesthesiologist, the ability to make decisions that are impactful, in the setting of imperfect information, is key. I believe that this ‘tolerance of risk’ helped me to make the decision to start Humacyte.”
All photography courtesy Humacyte
Humacyte’s Human Acellular Vessel (HAV)
A Breakthrough in Regenerative Medicine
Off-the-shelf (immediately available) with an 18-month shelf life
Highly resistant to infection
No evidence of immunogenicity
Host cells repopulate the HAV
For ESRD patients, accessible for dialysis access within one month of implantation
Long-term durability is demonstrated in ongoing studies
Source: humacyte.com
Q: What are your greatest lessons in launching a start up?
A: Everything takes longer than you think it will. Paying attention to details is important. Getting the right people in the right roles is hugely important.
Q: What is the future of Humacyte and your research?
A: Humacyte is working on several pipeline products, including a vessel for coronary artery bypass grafting (CABG), and a vessel that can act as a delivery vehicle for pancreatic islets for the eventual treatment of type 1 diabetes.

Q: How did you decide to come back to Durham to run Humacyte full time?
A: At different points in a career, you can make a maximal impact doing different things. I felt that I could make the greatest impact by running Humacyte at this stage of my life.
Q: When people describe you as a “trailblazer,” what does that mean to you?
A: I think that trailblazers are, by definition, people who are unperturbed by going off the trail. By trying something new and different – but not just for the sake of new and different – but because new and different might just be better. It has never bothered me to do things in a different way – so it is easy to leave the main trail and strike out in a new direction.
Q: What is your philosophy on work-life balance?
A: You can only have a short, finite number of things that are important to you. Making sure that your family knows that they are important, really important, matters. More
2017
Humacyte HAVs became the first product to receive FDA’s Regenerative Medicine Advanced Therapy (RMAT) designation; Inducted into Women in Technology Hall of Fame
2019
than lip service, but really important. The same goes with colleagues at work.
Q: What is your best advice to those looking to enter the anesthesiology specialty?
A: Don’t limit your potential areas of inquiry to the strict, narrow realm of anesthesiology. Since our specialty touches everything in the hospital, and touches all diseases, the world is our oyster.
Q: Last year, the key word in “Alumni Notes” was perseverance. What would you say is the key word of your journey?
A: Gosh, I might have said “Perseverance.” Lacking that, I would say “Bravery.” BP
State-of-the-art manufacturing facility commissioned in Durham, NC
2020 Elected a member of the National Academy of Engineering
ALUMNI NOTES
BLUE PRINT 2022 | 67
DEPARTMENT CHAIRMAN
Joseph P. Mathew, MD, MHSc, MBA
Jerry Reves, MD, Professor of Cardiac Anesthesiology
Ambulatory Anesthesiology
Alex Cravanas, MD, MBA
Michael Kent, MD
Steve Melton, MD

Karen Nielsen, MD
Juhnnel Vera Santiago, MD
CHAIR’S COUNCIL: (pictured left to right)

Mark Stafford-Smith, MD, CM, FRCP(C), MBA, FASE
Miriam M. Treggiari, MD, PhD, MPH
Gavin Martin, MB ChB, FRCA, MMCi
Joseph P. Mathew, MD, MHSc, MBA
LEADERSHIP COUNCIL:
Atilio Barbeito, MD, MPH
John Borrelli, MBA
Dan Cantrell
Adam Flowe, CRNA
Jeffrey C. Gadsden, MD, FRCPC, FANZCA
Padma Gulur, MD
Dhanesh K. Gupta, MD, MBA

Ashraf S. Habib, MBBCh, MSc, MHSc, FRCA
Edmund H. Jooste, MB ChB
Evan Kharasch, MD, PhD
Stephen M. Klein, MD

Vijay Krishnamoorthy, MD, MPH, PhD
Melinda F. Macalino
Evan Kharasch, MD, PhD

Padma Gulur, MD
Madhav Swaminathan, MD, MMCi, FASE
John Borrelli, MBA
Gavin Martin, MB ChB, FRCA, MMCi
Joseph P. Mathew, MD, MHSc, MBA
Timothy E. Miller, MB ChB, FRCA
Adeyemi J. Olufolabi, MBBS, DCH, FRCA
Mihai V. Podgoreanu, MD, FASE
Dana Rawls
Edward G. Sanders, MD
Mark Stafford-Smith, MD, CM, FRCP(C), MBA, FASE
Madhav Swaminathan, MD, MMCi, FASE
Annemarie Thompson, MD
Miriam M. Treggiari, MD, PhD, MPH
Kevin Vorenkamp, MD, FASA
Cardiothoracic Anesthesiology
Brandi Bottiger, MD
Anne Cherry, MD
Kamrouz Ghadimi, MD
Loreta Grecu, MD
Nazish Hashmi, MBBS
Rebecca Klinger, MD, MS
Sundar Krishnan, MBBS
Jerrold Levy, MD, FAHA, FCCM
Yasmin Maisonave, MD
Negmeldeen Mamoun, MD, PhD
Joseph Mathew, MD, MHSc, MBA
Sharon McCartney, MD, FASE
Sachin Mehta, MD
Alina Nicoara, MD, FASE
Angela Pollak, MD
Mark Stafford-Smith, MD, CM, FRCP(C), MBA, FASE
Madhav Swaminathan, MD, MMCi, FASE
Annemarie Thompson, MD
Ian Welsby, MBBS, FRCA
Meredith Whitacre, MD
Community
Lu Adams, MD
David Bacon, MD
Lindsey Bewley, DO
Ryan Bialas, MD
Ajinder Chhabra, MD
Stephanie Cooper, MD
Nathan Davis, MD
Benjamin Dunne, MD
Matthew Glass, MD
Christopher Gratian, MD
Elsje Harker, MD
John Heath, MD
Erica Heniser, MD
68 | DUKE ANESTHESIOLOGY DEPARTMENTAL FACULTY
CHIEF: Stephen M. Klein, MD
CHIEF: Mihai V. Podgoreanu, MD, FASE
CHIEF: Edward G. Sanders, MD
Daniel Kovacs, MD
Henry Lather, MD
Eugene Lee, MD
Andrew Lloyd, MD
Debabrata Maji, MD
Jonathan Mathew, MD
Cory Maxwell, MD
Andrea Mazzoni, MD
Scott McCulloch, MD
Tyler McCulloch, MD
Elizabeth Nichols, MD
William Norcross, MD
Shannon Page, MD
Gary Pellom, MD
Lisette Ramos, MD
Earl Ransom Jr., MD
Benjamin Redmon, MD
Richard Runkle III, MD
Siddharth Sata, DO
Nicole Scouras, MD
Kavitha Sharkady, MD
Michael Stella, MD
Zaneta Strouch, MD, MPH
Frank Sutton, MD
Leonard Talbot, MD
Neel Thomas, MD

Danai Udomtecha, MD
Andrew Wong, MD
CHIEF:
Vijay Krishnamoorthy, MD, MPH, PhD
Critical Care Medicine
Omar Al-Qudsi, MD
Sandy An, MD, PhD
Yuriy Bronshteyn, MD
Kathleen Claus, MD
Blair Costin, MD, PhD
Michael Devinney, MD, PhD
Amanda Faulkner, MD
Taylor Herbert, MD, PhD
Ehimemen Iboaya, MD
Nancy Knudsen, MD
RJ Krom, MD, PhD
Nitin Mehdiratta, MD
Rachael Mintz-Cole, MD, PhD
Jamie Privratsky, MD, PhD
Galen Royce-Nagel, MD
Mara Serbanescu, MD
Arturo Suarez, MD
Miriam Treggiari, MD, PhD, MPH
Paul Wischmeyer, MD, EDIC
Miguel Yaport, MD
Christopher Young, MD, FCCM
CHIEF:
Timothy Miller, MB ChB,
General, Vascular & Transplant Anesthesiology
Chakib Ayoub, MD, MBA


Jeanna Blitz, MD, FASA
Brian Colin, MD
Derek Covington, MD

Bruce Derrick, MD
Jonathan Dunkman, MD
Sarada Eleswarpu, MD
Arun Ganesh, MD
Heath Gasier, PhD
Evan Kharasch, MD, PhD


Catherine Kuhn, MD
Rachel Lance, PhD
Michael Manning, MD, PhD
Richard Moon, MD, CM, MSc, FRCP(C),
FACP, FCCP
Eugene Moretti, MD, MHSc
Hagir Suliman, DVM, PhD
Ankeet Udani, MD, MSEd
Kerri Wahl, MD, FRCP(C)
David Williams, MD, MPH
Erin Manning, MD, PhD
Gavin Martin, MB ChB, FRCA, MMCi
Hector Martinez-Wilson, MD, PhD

Brian Ohlendorf, MD


Stephen Parrillo, MD
Neil Ray, MD
CHIEF:
Kevin Vorenkamp, MD, FASA
John Lemm, MD
David Lindsay, MD
Amy Manchester, MD
Jonathan Mark, MD
Grace McCarthy, MD
Harika Nagavelli, MD
Srinivas Pyati, MD, MBBS
Karthik Raghunathan, MBBS, MPH
Lance Roy, MD
Rebecca Schroeder, MD
Timothy Stanley, MD
Thomas Van de Ven, MD, PhD
Pain Medicine
Aurelio Alonso, DDS, MS, PhD
Muhammad Anwar, MD, MBA
Thomas Buchheit, MD
Nathan Christie, MD
Cain Dimon, MD
Padma Gulur, MD
Dimitri Putilin, PhD
Scott Runyon, MD
Jean Elie Tabbal, MD
Daniela Vivaldi, DDS
Peter Yi, MD, MSEd
CHIEF:
K.
Neuroanesthesiology, Otolaryngology & Offsite Anesthesiology
Miles Berger, MD, PhD
Nicole Guinn, MD
Jennifer Hauck, MD
Thomas Hopkins, MD, MBA
Michael “Luke” James, MD, FAHA, FNCS
Colleen Naglee, MD
Andrew Peery, MD, MPH
Vijay Ramaiah, MBBS
Bryant Stolp, MD, PhD
MD,
CHIEF:
Edmund H. Jooste, MB ChB
Pediatric Anesthesiology
Warwick Ames, MBBS
Jon Andrews, MD
Guy Dear, MA, MB, BChir, FRCA, FUHM
John Eck, MD
Lisa Einhorn, MD
Hercilia Homi, MD, PhD
Martha Kenney, MD
Elizabeth Malinzak, MD
Matthew McDaniel, MD
John McManigle, MD
Allison Ross, MD
Brad Taicher, DO, MBA
Andrea Udani, MD
CHIEF:
C.
Orthopaedics, Plastics & Regional Anesthesiology
W. Michael Bullock, MD, PhD
Joshua Dooley, MD
Amanda Kumar, MD
David MacLeod, MBBS, FRCA, Dip IMC
MD,
CHIEF:
Atilio Barbeito, MD, MPH
Veterans Affairs
Anesthesiology Service
Sophia Dunworth, MD
Juliann Hobbs, MD, MPH
Hung-Lun (John) Hsia, MD
Eric JohnBull, MD, MPH
CHIEF:
Ashraf S. Habib, MBBCh, MSc, MHSc, FRCA
Women’s Anesthesiology
Terrence Allen, MBBS
Melissa Bauer, DO
Matthew Buck, MD
Jennifer Dominguez, MD, MHS
Jennifer Mehdiratta, MD, MPH
Abigail Melnick, MD
Marie-Louise Meng, MD
Adeyemi Olufolabi, MBBS, DCH, FRCA
Cameron Taylor, MD
Mary Yurashevich, MD, MPH
DIRECTOR: Luis Ulloa, PhD, MS
Center for Perioperative Organ Protection
Madan Kwatra, PhD
Huaxin Sheng, MD
Wei Yang, PhD

DIRECTOR: Ru-Rong Ji, PhD
Center for Translational Pain Medicine
Satya Achanta, DVM, PhD
Andrey Bortsov, MD, PhD
Christopher Donnelly, DDS, PhD
Sven-Eric Jordt, PhD
Francis Keefe, PhD
Katherine Martucci, PhD
Andrea Nackley, PhD
Shad Smith, PhD
Niccolò Terrando, PhD
DEPARTMENTAL FACULTY
FRCA
Jeffrey
Gadsden,
FRCPC, FANZCA
Dhanesh
Gupta,
MBA
BLUE PRINT 2022 | 69



9.10.22 The Cotton Room . Durham, NC 32 nd Annual Duke Anesthesiolo gyASA Alumni Event New Orleans, LA 10.23.22
Hosted by Stacey Hilton DIRECTOR OF



The Inside Duke
you behind
oneon-one

department and

discuss how

BLUE PRINT 2022 | 71
Anesthesiology Podcast takes
the curtain for
interviews with experts in our
across Duke to
we’re “changing the face of anesthesiology.”
COMMUNICATIONSLaunched in 2020
NIH funding
Source: Blue Ridge Institute for Medical Research E X T R A O R D I N A R Y SCIENCE. LIFE-CHANGING DISCOVERIES. in
#
in the nation#3


be the leader in advancing perioperative medicine and pain management.
care through a unique culture of innovation, education, research, and professional growth.

VISION: To
MISSION: Extraordinary
There’s no place like Duke.










































 Dr. Michael “Luke” James
Dr. Miles Berger
Dr. Michael “Luke” James
Dr. Miles Berger







 Dr. Marie-Louise Meng Dr. Adeyemi Olufolabi Dr. Jennifer Dominguez
Dr. Marie-Louise Meng Dr. Adeyemi Olufolabi Dr. Jennifer Dominguez







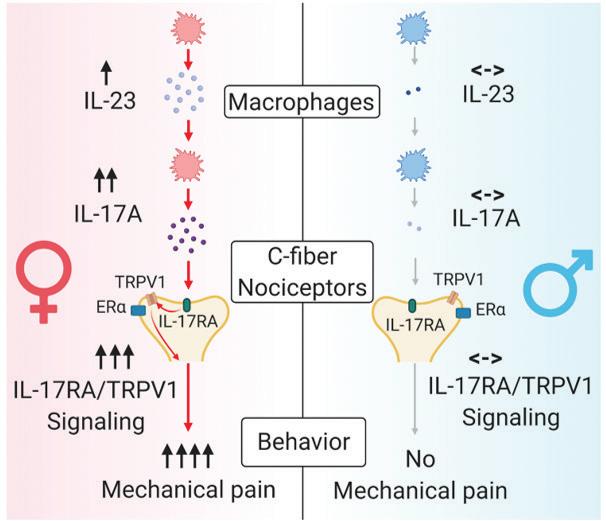




































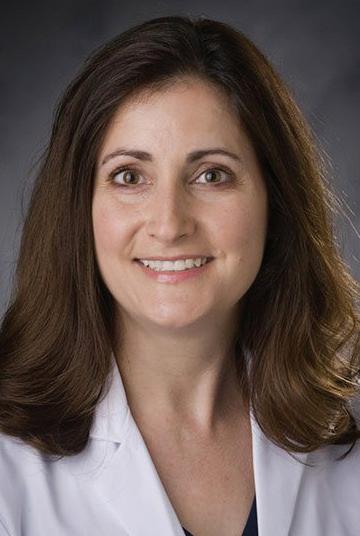

























 JAMIE PRIVRATSKY, MD, PHD
JAMIE PRIVRATSKY, MD, PHD









































 DR. BRIAN COLIN Associate Director, Residency Program
DR. BRIAN COLIN Associate Director, Residency Program
































