KNOWLEDGE
COVERAGE BEYOND
COPIC’s premier medical liability insurance offers comprehensive support built on unparalleled expertise and decades of experience. We share our knowledge through meaningful CME/CNE education, an extensive library of resources, in-depth site visits, and more. All of which help you avoid risks, improve practice protocols, and solve urgent issues quickly. That’s Value Beyond Coverage.
COPIC is proud to be the endorsed carrier of the Colorado Medical Society. CMS members may be eligible for a 10% premium discount.

IT’S TOO LATE TO TURN BACK NOW
14 BURNOUT RATE SPIKED IN 2020 AND 2021
The rate of burnout among physicians in the United States spiked dramatically during the first two years of the pandemic. One of the authors of a new study on this spoke at the University of Colorado Anschutz Medical Campus on Sept. 22 at an event supported by the Colorado Medical Society.

15 CMS PREPARES FOR THE 2023 LEGISLATIVE SESSION

The Colorado Medical Society is preparing for a busy legislative session that will likely include many bills affecting physicians. The Colorado General Assembly convenes Jan. 9, 2023.

28 FINAL WORD: ELECTION DAY IS JUST THE BEGINNING
COMPAC Chair Sean Pauzauskie, MD, discusses how the 2022 election will affect state-level politics, and why physicians must be involved in the legislative process.
16 COPIC Comment: The value of early reporting of adverse incidents 18 Reflections: Something more 19 Reflections: Senses 20 Introspections: Malarone dreams
10 PHOTOS FROM THE CMS ANNUAL MEETING IN BRECKENRIDGE
Physicians from around the state gathered for the 2022 Annual Meeting in Breckenridge Sept. 16-17. This was our first in-person annual meeting since 2019 and members were excited to be together to learn and laugh in a beautiful mountain setting.
12 RESULTS FROM THE 2022 CMS MEMBER SURVEY
CMS members were invited to share their thoughts on how our society is serving Colorado physicians through the 2022 CMS member survey. Advocacy and communications, once again, rank as top priorities for CMS resources. Members also feel that it is important for CMS to promote health equity and reduce health disparities.
COLORADO MEDICAL SOCIETY
7351 Lowry Boulevard, Suite 110 • Denver, Colorado 80230-6902
720.859.1001 • fax 720.859.7509 • www.cms.org
OFFICERS, BOARD MEMBERS, AMA DELEGATES, and STAFF
2022-2023
OFFICERS
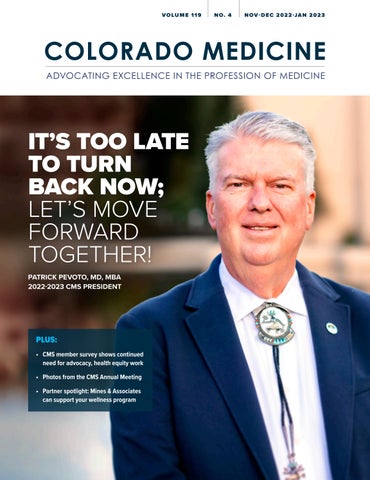
Patrick Pevoto, MD, MBA
President
Omar Mubarak, MD, MBA
President-elect
Hap Young, MD
Treasurer
Mark Johnson, MD, MPH
Immediate Past President
Dean Holzkamp Chief Executive Officer
BOARD OF DIRECTORS
Brittany Carver, DO
Amy Duckro, DO
Gabriela Heslop, MD
Enno F. Heuscher, MD, FAAFP, FACS
Rachelle M. Klammer, MD
Marc Labovich, MD
Chris Linares, MD
Michael Moore, MD
Edward Norman, MD
Courtney Olson, MS
Lynn Parry, MD
Leto Quarles, MD
Hap Young, MD
COLORADO MEDICAL SOCIETY STAFF
Dean Holzkamp
Chief Executive Officer
Dean_Holzkamp@cms.org
Kate Alfano
Director of Communications and Marketing
Kate_Alfano@cms.org
Jennifer Armstrong Program Manager, Government Affairs and Communications
Jennifer_Armstrong@cms.org
Cindy Austin
Director of Membership
Cindy_Austin@cms.org
Dianna Fetter
Senior Director of Business Development
Dianna_Fetter@cms.org
Amy Goodman, JD, MBE
Senior Director of Policy Amy_Goodman@cms.org
Crystal Goodman
Executive Director, Northern Colorado Medical Society
Crystal_Goodman@cms.org
Ms. Gene Richer, M Ed, CHCP
Director of Continuing Medical Education and Recognized Accreditor Programs
Gene_Richer@cms.org
AMA DELGATION
David Downs, MD, FACP
Carolynn Francavilla, MD
Rachelle Klammer, MD
Katie Lozano, MD, FACR
A. "Lee" Morgan, MD
Jan Kief, MD
Tamaan Osbourne-Roberts, MD
Lynn Parry, MD
Brigitta J. Robinson, MD Michael Volz, MD
AMA PAST PRESIDENT
Jeremy A. Lazarus, MD
Mihal Sabar
Accounting Manager
Mihal_Sabar@cms.org
Chet Seward
Chief Strategy Officer
Chet_Seward@cms.org
Debra Will
Assistant Director of Continuing Medical Education and Recognized Accreditor Programs
Debra_Will@cms.org
Tim Yanetta
IT/Membership Manager
Tim_Yanetta@cms.org
COLORADO MEDICINE (ISSN-0199-7343) is published bimonthly as the official journal of the Colorado Medical Society, 7351 Lowry Boulevard, Suite 110, Denver, CO 80230-6902. Telephone 720-859-1001. Periodicals postage paid at Denver, Colo., and at additional mailing offices. POSTMASTER, send address changes to COLORADO MEDICINE, P. O. Box 17550, Denver, CO 80217-0550. Address all correspondence relating to subscriptions, advertising or address changes, manuscripts, organizational and other news items regarding the editorial content to the editorial and business office. Subscriptions are available for $36 per year, paid in advance.
COLORADO MEDICINE magazine is the official journal of the Colorado Medical Society, and as such is also authorized to carry general advertising. COLORADO MEDICINE is copyrighted 2006 by the Colorado Medical Society. All material subject to this copyright appearing in COLORADO MEDICINE may be photocopied for the non-commercial purpose of education and scienti fic advancement. Publication of any advertisement in COLORADO MEDICINE does not imply an endorsement or sponsorship by the Colorado Medical Society of the product or service advertised. Published articles represent the opinions of the authors and do not necessarily reflect the official policy of the Colorado Medical Society unless clearly specified.
Dean Holzkamp, Executive Editor, and Kate Alfano, Managing Editor. Design by Scribner Creative.
Commit to something greater
We deliver care through New West Physicians in Denver as well as the Optum and Mountain View Medical Groups in Colorado Springs. We invite you to be part of our incredible momentum in medicine. The research, growth, and emphasis on technology make this a place where you can have a real impact—and spend more time treating your patients, too. And you’re always backed by the stability of a nationwide health care leader.
Practice medicine the way it was meant to be practiced. Join the Optum team. Contact Chad Smith at 763-361-5975 or chad_smith@optum.com See the difference you can make at optumcareersco.com

It’s too late to turn back now; let’s move forward together!
ADAPTED FROM THE INAUGURAL ADDRESS OF THE 152ND COLORADO MEDICAL SOCIETY ANNUAL MEETING
Patrick Pevoto, MD, MBAThe 1972 song “Too Late to Turn Back Now” by the Cornelius Brothers and Sister Rose talks about the possible pitfalls of falling in love. However, trying to “turn back” for other reasons has its own dangers and pitfalls.

According to Brené Brown in her book “Atlas of the Heart” (Random House 2021), we need to not only understand our own emotions and experiences, but to also be good stewards of others’ emotions and experiences to make meaningful connections with one another.
One such emotion is nostalgia, a medical term coined in 1688 by Johannes Hofer, a Swiss medical student, by combining the Greek words “nostos” (homecoming) with “alga” (pain). He saw the patterns of those living far from home; the symptoms included decreased appetite, fainting, as well as an increased risk of suicide. Albert Van Holler, a Swiss physician, added the occurrence of hallucinations of the people and places one misses as experienced by many Swiss mercenaries who were fighting far-flung wars at the time.
Historian Stephanie Coontz states: “There is nothing wrong with cele brating the good things of the past. But memories, like witnesses, do not always tell the truth, the whole truth, and nothing but the truth. We need to cross-examine them recognizing and accepting the inconsistencies and gaps in those that make us proud and happy as well as those that cause us pain.”
I have been guilty of having nostalgia; wishing we still had paper charts, wishing I could have segued into a less busy and more lucrative gynecology practice,
wishing there were no third parties involved in billing… the list is quite extensive. During the process of remi niscing, there are things spoken and things not spoken.


What’s spoken:
• “I wish things were the way they used to be in the good ol’ days.”
What’s not spoken:
• When people “knew their places.”
• When there was no accountability for the way my behaviors affected other people.
• When we ignored other people’s pain if it caused us discomfort.
• When my authority was absolute and never challenged.
In further defining nostalgia, it could be characterized as a yearning for the way things used to be in our often idealized and self-protective version of the past.
Historian Coontz also adds: “Were the comfort and safety of that past experience real? If so, were they at someone else’s expense?”
I think I have tried to be in control of as much of my life as possible. It is probably one of the main reasons I chose medicine as my career. It seemed to me that many other occupations had the hidden threat of losing one’s job, many times at the whim of someone else, for a myriad of reasons. At least if I started my own medical practice, and became proficient at it, I could “call all the shots.” One could say that I had a fear of losing control.
What do we really control in life? As Michael Singer often says (with editorial changes), “We are on this speck of dirt in mostly empty space. Why do we let things that are entirely out of our control (weather, traffic, legislatures) affect us so much?” We either grasp and cling to the “feel-goods” of life or resist/ push away those things we don’t like. It is like the following.
I like it when:
• Things go the way I want/plan.
• I don’t have to respond to “Google-re searched” questions.
• There are no “soul suckers” on my schedule today.
• Traffic is not “heavy,” and people drive with intelligence.
• The foursome in front of me actually plays “ready golf.”
We tend to grasp these sorts of things.
I don’t like it when:
Forces beyond your control can take away everything you possess except for one thing, your freedom to choose how you will respond to the situation. You cannot control what happens to you in life, but you can always control what you will feel and do about what happens to you.”
- Dr. Viktor Frankl
• Patients/nurses/etc. challenge my advice.

• The same patient comes in weekly, if not more frequently, with the same complaint.
• The surgical tech throws away the sterile marker that I requested on “my card” because she does not think I need it, telling me “no one else does.”
• The rules/protocols change almost daily.
We tend to push these away.
Our responses to events, interactions with others, and decisions can usually
be responses of either love or fear. One day my oldest son Andrew came to me for advice about a decision he needed to make. Somewhere out of seemingly nowhere at the time I responded, “just don’t make a decision out of fear.” It is hard to be vulnerable enough with others to respond in love.
Dr. Viktor Frankl was an Austrian-born psychiatrist who lived in Nazi-occupied Austria in the 1930s. He had the oppor tunity to leave for the United States and escape Nazi aggression since he was of the Jewish faith. He decided to stay and assist his parents who could not go along with him. His mother and father were exterminated; he lived captive in Auschwitz, Dachau and other concentra tion camps for three years before being liberated by Allied forces. He observed his fellow inmates, many of whom were murdered or succumbed to illness, but universally those who lost their hope did not survive. Viktor continued to hope for being reunited with his wife, to eventually get to the United States to practice psychi atry. While Sigmund Freud postulated a human’s primary quest was for "pleasure" and Alfred Adler proposed that the quest was for “power,” Frankl stipulated that the quest was for “meaning.”
He further delineated the three sources of meaning:
• Meaning in work.
• Meaning in love (relationships).
• Meaning in courage during difficult times.
To quote Dr. Frankl: “Forces beyond your control can take away everything you possess except for one thing, your freedom to choose how you will respond to the situation. You cannot control what happens to you in life, but you can always control what you will feel and do about what happens to you.”
Providing quality care for 100 years
For the last century, the Good Samaritan Society has been committed to providing an unprecedented level of quality service to ensure your patients are safe and cared for.
Our expansive footprint ensures we have the expertise to provide them with a smooth transition through various levels of care.
“We’ve been doing this for 100 years. We specialize in it,” says the Good Samaritan Society’s chief medical officer, Gregory Johnson, MD. “We provide support that meets people where they are.”
And this support starts immediately after someone is discharged from the hospital.
“We work with our hospital and physician partners. That’s a special level of collaboration and integration,” Dr. Johnson says.
The impact of exceptional senior care
Delivering the best care in a resident-centered environment has always been our focus. We believe that relationships, collaboration and human connection are essential to what we do.

Using an integrated approach, we’re improving quality of life and well-being while continually developing better standards of care across our communities. Services vary by location but may include:
• Assisted living – Convenient, maintenance-free living with services, amenities and security features to help residents live vibrantly.
• Home-based services – Customized, in-home medical or non-medical care within the comfort of a person’s home with extra support for meals, medications and more.
• Long-term care – 24-hour care and services for those who need the assistance of licensed nursing or rehabilitative staff.
• Rehab therapy – Quality inpatient or outpatient services using physical, occupational and speech therapies to enhance recovery after a hospitalization, illness or injury.
When you choose the Good Samaritan Society, your patient will be cared for by dedicated experts there to promote their well-being.
Partner with the right choice
Whether your patient needs 24-hour care, rehabilitation therapy or care at home, referrals to the Good Samaritan Society are easy and convenient:
• Call your local Good Samaritan Society location
• Call (855) 446-1862 to speak to a specialist about services
• Visit our Health Care Partners page at good-sam.com to use our simple online referral form
We partner with you to provide the best outcomes for your patient – supporting them physically, emotionally and spiritually through the health care journey.
Whatever level of care they need when leaving the hospital, the Society is ready to help restore their well-being.
If you have questions about referring patients or want to learn more about our services, please call (855) 446-1862 or visit our Health Care Partners page at good-sam.com.
How does one achieve the ability to hope? Researcher C.R. Snyder summed it up with the following trilogy:
• Ability to set realistic goals (“I know where I want to go”).
• Ability to figure out how to achieve those goals (requiring flexibility as well as accepting/developing alternate pathways).
• Having agency – believing in ourselves (I can do this!).
Brené Brown also adds: “We need hope like we need air.”
I believe in the call to surrender, to let go. This does not mean giving up in any way. When the person in front of you is driving way below the speed limit and there is no way to safely go around them, let go... take a breath and let the feelings pass through you. Know who you are in there! Know your “why,” what your meaning is in
Darkness
cannot drive out darkness; only light
can do that. Hate cannot drive out hate; only love can do that.
- Dr. Martin Luther King, Jr
this life. Choose to open your heart, not close it. This will take practice! Refuse to live in the past; choose to live in the now.

Mahatma Gandhi stated: “Our ability to reach unity in diversity will be the beauty and the test of our civilization.”
According to Dr. Cornel West: “None of us alone can save the nation or the world. But each of us can make a positive differ ence if we commit ourselves to do so.”
Dr. Martin Luther King, Jr. said: “Darkness cannot drive out darkness; only light can do that. Hate cannot drive out hate; only love can do that.”
The Gospel of Luke, Chapter 17, verse 33 (New Living Translation) says: “If you cling to your life, you will lose it, and if you let your life go, you will save it.”
The hope for medicine is service. The Prayer of St. Francis is the following:
“Lord, make me an instrument of your peace.
Where there is hatred, let me bring love.
Where there is offence, let me bring pardon.
Where there is discord, let me bring unity.
Where there is error, let me bring truth.
Where there is doubt, let me bring faith.
Where there is despair, let me bring hope.
Where there is darkness, let me bring light.
Where there is sadness, let me bring joy.
Oh master, let me not seek as much to be consoled as to console.
To be understood as to understand.
To be loved as to love.
For it is in giving that one receives.
It is in self-forgetting that one finds. It is pardoning that one is pardoned.
It is in dying that one is raised to eternal life.”
That, my fellow colleagues, is the hope for medi cine. It’s too late to turn back now! Let’s move forward together in this great endeavor. We can do this! ■


Board of Directors meeting






MEETING Breckenridge

Opening reception
 C olorado Medical Society members from around the state gathered for the 2022 Annual Meeting in Breckenridge Sept. 16-17. Attendees were excited to be back in person and gave high marks to the programming and social events. We hope all members will join us in person for a local or state event in 2023. View all events at cms.org/events.
C olorado Medical Society members from around the state gathered for the 2022 Annual Meeting in Breckenridge Sept. 16-17. Attendees were excited to be back in person and gave high marks to the programming and social events. We hope all members will join us in person for a local or state event in 2023. View all events at cms.org/events.
Saturday morning education


Afternoon education
Medical student meeting










 1 CMS honored the physicians celebrating 50 years since graduating from medical school. From left, H. Manning Picket, MD, Joseph Soler Jr., MD, Robert Bradley, MD, and James Britton, MD. 2 COPIC CEO Gerald Zarlengo, MD, right, presents the COPIC Humanitarian Award to Rush Pierce, MD, left. 3 Incoming CMS President Pevoto gives his inaugural address. 4 Attendees enjoy a wonderful buffet dinner at the President's Gala.
1 Political journalist Marianne Goodland gave insight into the 2022 elections and 2023 legislative session as the keynote speaker of the COMPAC luncheon. 2 AMA President Resneck discussed efforts to increase health care value on the federal level during a CME session. 3 CMS Past President Brent Keeler, MD, posed a question to a speaker during a CME session 4 Josh Blum, MD, led a CME session on best practices in pain management.
Medical students from the University of Colorado School of Medicine and Rocky Vista University College of Osteopathic Medicine gathered to hear from CMS and AMA leaders and discuss the benefits of involvement in organized medicine.
1 CMS honored the physicians celebrating 50 years since graduating from medical school. From left, H. Manning Picket, MD, Joseph Soler Jr., MD, Robert Bradley, MD, and James Britton, MD. 2 COPIC CEO Gerald Zarlengo, MD, right, presents the COPIC Humanitarian Award to Rush Pierce, MD, left. 3 Incoming CMS President Pevoto gives his inaugural address. 4 Attendees enjoy a wonderful buffet dinner at the President's Gala.
1 Political journalist Marianne Goodland gave insight into the 2022 elections and 2023 legislative session as the keynote speaker of the COMPAC luncheon. 2 AMA President Resneck discussed efforts to increase health care value on the federal level during a CME session. 3 CMS Past President Brent Keeler, MD, posed a question to a speaker during a CME session 4 Josh Blum, MD, led a CME session on best practices in pain management.
Medical students from the University of Colorado School of Medicine and Rocky Vista University College of Osteopathic Medicine gathered to hear from CMS and AMA leaders and discuss the benefits of involvement in organized medicine.
2022 CMS member survey
RESULTS SHOW MEMBER NEED OF CMS ADVOCACY, COMMUNICATIONS AND HEALTH EQUITY WORK
Benjamin KupersmitOVERVIEW
• The 2022 results of the CMS member survey reveal some softening in ratings around communication and feeling connected to CMS versus 2017-2019 results, but core metrics around recommendation and perceptions of the effectiveness of CMS (in improving the health system and their practices) have remained largely unmoved.

• CMS continues to be valued primarily for its advocacy and information.
CMS: MEMBER RATINGS
A majority of members give CMS positive marks almost across the board; the softest scores are for “reflecting priorities,” with a considerably higher “not sure” response of 10 percent than for other questions
• Members rely on Colorado Medicine and the ASAP enewsletter, as well as the PolicyPulse enewsletter, as useful sources of information. Communicates well with membership on the issues facing the medical profession
Gives members like me a chance to provide input and suggestions
having a positive impact on the health care system in Colorado Has a positive impact on my career as a physician in Colorado
A majority also give positive ratings regarding key questions regarding being involved and feeling respected; a substantial number — 21 percent — give a “not sure” response on valuing people of all backgrounds.
Colorado's physicians have an opportunity to be involved at all levels with CMS I feel included and respected at CMS People of all backgrounds and perspectives are valued at CMS
“Would you recommend CMS membership” has remained strong, with 67 percent saying 100% or agree strongly.
OTHER FINDINGS
PROMOTING HEALTH EQUITY
The Colorado Medical Society Board of Directors voted in 2020 to make diversity, equity and inclusion a strategic goal and develop a strategic plan for DEI.
• Physicians place great priority on CMS promoting health equity and reducing health disparities, with fully 84% of members saying this is important, and a majority (55%) saying very important.
• Members also agree (but with relatively softer scores) that promoting DEI specifically is essential to their success practicing medicine, with 68% in agreement (46% strongly).
• Active practice: 70% agree; retired, 58% agree
• Female physicians in active practice: 89% agree (71% strongly); male physicians, 63% agree (37% strongly)
• Active practice not identifying as white: 76% agree (59% strongly); among identifying as white, 75% agree (52% strongly)
• 77% of primary care agree, versus 62% among specialists
DEI TRAINING PROGRAMS
• 43% have participated in a DEI training
• 45% of members in active practice (versus 36% of retired members)
• 49% of those in primary care (versus 37% for specialist)
• 58% of female physicians (versus 36% of male physicians)
• 59% of those who do not identify as white (versus 43% of those who identify as white)
• 51% are satisfied with their DEI training program options (21% very satisfied and 30% somewhat satisfied)
• 20% are not satisfied
• 30% are not sure or said this doesn't apply ■
• All-member survey conducted by Kupersmit Research Aug. 13-Sept. 15, 2022
• 354 members gave a full response to the survey, of a total of 5,582 CMS members emailed (with 455 beginning the survey), giving a 6% response rate
• Margin of error of +5.2% at the 95% confidence level
Burnout rate spiked during first two years of COVID-19 pandemic



PHYSICIANS GATHER FOR EDUCATIONAL EVENT WITH RENOWNED BURNOUT RESEARCHER LOTTE DRYBYE, MD, MHPE
 Stefanie Carroll, Executive Director, Denver
Stefanie Carroll, Executive Director, Denver
The burnout rate among physicians in the United States spiked dramatically during the first two years of the COVID-19 pandemic, according to a study published in September in Mayo Clinic Proceedings. In the study, “Changes in Burnout and Satisfaction with Work-Life Integration in Physicians During the First 2 Years of the COVID-19 Pandemic,” researchers found that 2020 marked the end of a six-year period of decline in the overall rate of work-induced burnout among physicians. By the end of 2021, after 21 months of the COVID-19 pandemic, the physician burnout rate spiked to a new height that was greater than previously monitored by researchers.
One of the authors of the new study, Lotte N. Dyrbye, MD, MHPE, gave an informative lecture on her findings on Sept. 22 on the University of Colorado Anschutz Medical Campus in Aurora, Colo.


Following the lecture, Colorado Physician Health Program (CPHP) medical director Scott Humphreys, MD, moderated a ques tion-and-answer session with Drybye. CPHP provides confidential peer assis tance counseling to physicians, residents, medical students, physician assistants, physician assistant students, anesthe siology assistants, and anesthesiology students with health problems, including medical conditions, psychiatric illnesses, substance abuse, and/or personal prob lems such as family difficulties, stress, or career issues.
Services are provided at no cost to Colo rado licensed physicians and physician assistants. Residents, medical students, and physician assistant students may also be eligible for free services through contracts between CPHP and various Colorado-based training programs. CPHP has directly served over 6,000 medical professionals since their inception in 1986.
Medical Society
The event was hosted by the Denver Medical Society and Denver Medical Soci ety Foundation, and co-hosted by Auro ra-Adams County Medical Society, Arap
ahoe-Douglas-Elbert
Medical Society, Colorado Medical Society,
Northern Colorado Medical Society and University of Colorado School of Medicine. ■
Colorado Medical Society prepares for 2023 legislative session
 Kate Alfano, CMS Director of Communications and Marketing
Kate Alfano, CMS Director of Communications and Marketing
The Colorado Medical Society has been busy through the summer interim and election season, thanks to the bipartisan CMS Political Action Committee, COMPAC. Weighing in on 67 races, physicians around the state interviewed their local candidates to discuss medi cine’s top priorities. COMPAC's candi date win rate was 88 percent in the House and 69 percent in the Senate.
COMPAC is unique for our thorough candi date interview process, which educates candidates on the minutia of physician priorities and vets them on their health care stance. We extend a grateful thank you to all the physicians and friends of medicine who participated in the process and contributed to COMPAC and the Small Donor Committee (SDC).
The interview process also helps CMS build relationships with legislators, and this helps our advocacy efforts as we have had focused time for dialogue with them before the busy session starts – this year on Jan. 9, 2023.
Inappropriate scope of practice expan sion by non-physician providers has been a pressing issue over the last few legisla tive sessions and next year will see more attempts. After failing in 2021 and 2022, physician assistants (PA) are expected to champion another legislative push next year to expand their scope of practice.
CMS, working in concert with the House of Medicine, has met repeatedly with the Colorado Academy of Physician Assis tants over the summer to address their concerns about administrative burdens and our shared interest in ensuring Colo radans have access to the safe care they need. The sticking point continues to be PA interest in changing longstanding law and regulation to practice medicine independent of physician supervision. CMS has and will continue to be firm in our commitment to safety and physician-led care teams.
In addition to PA scope of practice expan sion, the next session will also feature a drive by psychologists to secure new
On Oct. 30, those in the Capitol community received the sad news that Rep. Hugh McKean, R-Loveland, died unexpectedly. The House minority leader was a great friend of medicine, trusted voice and collaborator. CMS expresses our condolences to his family.
authority to prescribe psychotropic medi cations. CMS is working closely with the Colorado Psychiatric Society on this issue.
We continue to advocate for reduced administrative burden for physicians, particularly in prior authorization. We are working with legislators to bring back a bill we supported in the 2022 session that would streamline the prior authorization process and reduce barriers to necessary care for patients.
As always, CMS is focused on maintaining the stability of the liability climate. Particu larly in the wake of action in California that

began as a ballot initiative that would have completely upended California’s insur ance market and resolved as a compro mise to raise the cap with adjustments for inflation, we are working closely with COPIC and other partners in monitoring potential threats to our tort environment. There will be continued conversation.
Thank you in advance for your engage ment in our advocacy efforts. If you have a story to share that could be part of testimony or talking points, we encourage you to reach out to our government affairs team. Email membership@cms.org ■
The value of early reporting of adverse incidents
 Gerald Zarlengo, MD Chairman & CEO, COPIC Insurance Company
Gerald Zarlengo, MD Chairman & CEO, COPIC Insurance Company

There is a phrase that we repeatedly tell our insureds: Contact COPIC after any major unexpected outcome or incident that could adversely affect a patient’s care. Why? Because early reporting is probably one of the most important aspects of medical liability insurance. The sooner COPIC knows, the sooner we can activate our resources and expertise for insured physicians.
• There is no penalty for early reporting of an incident.
• Promptly notifying COPIC of an inci dent allows us to consider all possible approaches for the best response and resolution.
• Early reporting enables us to capture details while an incident is fresh in everyone’s minds; it also allows us to evaluate whether a situation is appro priate for COPIC’s 3Rs Program or the Candor process – options that provide an alternative to traditional litigation that seek to maintain the physician-pa tient relationship and resolve matters after an adverse outcome.
• Reporting an incident also serves as a trigger to help determine if and how your insurance coverage may apply.
In addition to unexpected outcomes that adversely affect patients, you should report situations where litigation might
occur (e.g., threats or a notice of a lawsuit, attorney requests for medical records), disciplinary or professional review actions against an insured, and data breaches and other cyber liability issues.
HERE ARE GENERAL GUIDELINES FOR REPORTING AN INCIDENT TO COPIC:
1. Ideally, the provider involved should report the incident – we recognize that some systems may have specially trained risk managers to assist in reporting and we can accept a report from these managers on behalf of an insured.
2. Make every effort to report within a reasonable time (usually 24 to 72 hours) after the provider or practice becomes aware of the incident.
3. Report incidents by calling COPIC or initiating the process on our website. COPIC-insured physicians can report an incident at (720) 858-6395 during business hours (Monday-Friday, 8 a.m. - 5 p.m.); or they can initiate the report ing process at www.callcopic.com, which will result in a follow-up call by a nurse specialist. To submit an online incident report, login to the Service Center and select “Incident Reporting.”
4. Have the following information ready: patient identification, policy number, date(s) of service or incident, and procedure/medical services provided to include a summary of the incident.
A . Please note that you do not need to obtain a patient’s consent – writ ten or otherwise – to share HIPAA Protected Health Information (PHI) with COPIC in an incident report.

COPIC Medical Foundation: Submit an application for 2023 grant funding
The COPIC Medical Foundation (CMF) works to improve health care outcomes through grant funding of:

• Programs and initiatives that improve patient safety and quality of care or through systems changes and improvements.
• Pilot programs that are designed to reduce medical errors.
• Development and implementation of checklists and other tools to improve disease management and transitions in care.
2023 focus area: Fragmentation across care settings
For 2023, our grant funding will continue to focus on the issue of reducing fragmen tation across care settings. A top concern in the field of patient safety, breakdowns in care from a fragmented health care system can lead to readmissions, missed diagnoses, medication errors, delayed treatment, duplicative testing and proce dures, and reduction in quality of care leading to general patient and provider dissatisfaction.
Funding cycle
CMF is accepting applications Nov. 1, 2022 through Jan. 14, 2023 for its 2023 cycle of grant funding.
Criteria
To be considered for funding, orga nizations must meet the following minimum criteria:

• Approach or program has demon strated potential for uptake or replica tion by the health care community.
• Organization is designated as a 501(c) (3) organization or has an identified fiduciary.
Deadlines and applications
Grant applications are due Jan. 13, 2023, by 5 p.m. MST. Applications can be emailed to: mhintze@copic.com
Applicants can expect to hear from CMF regarding potential support by March 1, 2023. Download the grant requirements and application at www.callcopic.com/ about-copic/copic-medical-foundation
Something more
Helene KuffelI still remember the weeks before I started my clinical year of medical school. I had studied for thousands of hours in the classroom, taken countless exams, and seen patients in the hospital and clinic with my preceptors. Still, I felt like I knew next to nothing that would be of any use to me on the wards. I was not excited or ready to take care of patients; rather, I was terrified that I was fast approaching the moment when everyone would real ize I was faking it and had absolutely no clue what I was doing, and certainly had no right to be here among my talented and intelligent peers. I was convinced I had fooled everyone for two years and that the charade was about to come crumbling down around me.
Looking back, I see that there was a lot of “me” thinking. At no point in the lead-up to my clerkships did I step back to think about the bigger picture – about the patients I would meet, and how they would impact me just as much, if not more, than I would impact them. While it took me longer than I care to admit to see beyond my own anxiety, I got there, in the end, thanks to one patient in particular, who will likely stay with me long beyond medical school.
I continue to think about her every week, wondering about what else we could have done for her. Three weeks into my internal medicine rotation, I was sent to the emergency department to triage a new patient. One of the nurses pulled me aside to warn me, “I think she’s in withdrawal; she has a history of IV drug use, so be careful.” When I entered the room, I saw a young woman, my age, shaking and moaning, unable to sit still, struggling to breathe, and shrieking. “My body is not okay, something is wrong!” I tried to comfort her, and as I began to piece together her story, which was
difficult between her labored breathing and agitation, I learned that in addition to injection drug use (IDU), she had a history of severe multivalvular endocarditis with septic emboli, treated only four months prior with a bioprosthetic aortic valve. Now, she was presenting with a week of fevers, fatigue, and progressive short ness of breath.
Despite everyone’s judgments and preconceptions, she was adamant that she had not injected drugs since her surgery. Over the course of our workup, we determined that she once again was suffering from endocarditis, now complicated by a massive aortic root abscess. However, because of IDU and recent valve replacement, our surgeons would not bring her to the OR despite her rapidly deteriorating condition. Even with multiple providers, therapists and ID doctors defending the patient, they could not be swayed.
Around this time, cultures returned grow ing an organism more commonly associ ated with dental infections, and not IDU. I immediately went to see her, and she confirmed that she had been suffering from dental pain for weeks. Armed with this new information and imaging of a tooth abscess that further supported our patient’s story, we again reached out to the surgeons who then consented to perform the surgery. Our team worked around the clock. The dental team came in at 9 p.m. on a Friday night to remove her tooth. Now, her surgery, which had already been delayed by over a week, could finally take place.
I remember sitting with her while all of this was happening, trying to comfort her where I could, but mostly just trying to be present. She had no one else with her. She hadn’t spoken to her family in

over a year and asked that I not call her mother, who, she said, never believed her. I didn’t feel comfortable with this, but I didn’t push the issue. I thought we had time. When I left at 11 p.m. that Friday, I felt satisfied that things were moving forward. I felt like I had actually contributed some thing to her care.

That feeling was fleeting. When I arrived at the hospital the next day, my attend ing met me and shared the news that my patient had arrested and died early in the morning, en route to her surgery.
I kicked myself about a lot of things in the aftermath of her death. Why hadn’t I called her mother? Why hadn’t I stayed with her through the night? Why hadn’t I collected a better history and diagnosed her tooth infection sooner? Why didn’t everyone believe her? What was the last thing she said to me? I had no answers, and I had never felt emptier in my life.
This patient, and that week, completely changed my view of my third year of medi cal school. I had expected it to be impos sible, but impossible because of me and my lack of knowledge and skills. I hadn’t expected it to be impossible because I lost a patient my own age, after my team and I had done everything we could think of to save her. Until I met my patient and then lost her, I was still worrying mostly about my evaluations and my perceived shortcomings. I hadn’t realized that the third year of medical school, and prob ably all of medical training, means that we must begin to look beyond ourselves, in order to let patients into our lives, knowing that they may take hold of us. In fact, some patients will change us, just as much as, if not more than, we change them. Ultimately, I am thankful that many of my doubts and fears can now fade to make room for something more. ■
Senses
Lillian ToaspernLillie Toaspern is a fourth-year medical student at the University of Colorado School of Medicine. After being raised in Denver, she spent time in the Midwest, earning an undergraduate degree in anthropology from Washington University in St. Louis and playing professional soccer in Chicago. Her non-traditional journey to medicine reinforced her desire to treat patients’ health in the context of their daily lives, a mission she hopes to pursue as a family medicine physician. Being away also reinforced her love for Colorado (and its lack of bugs).


Frantic blue eyes searched the room
His gaze desperate His gaze lost
My words were impenetrable to his world
But touch –

Touch was connection Fingers on his forearm, his hand gripping mine
What did he need? How could I help?
Was just sitting here enough?
Every time I saw him, we touched One day we hugged The next day he was gone ■
Malarone dreams
Robert EnglishCritical reflective writing holds a prominent place in the Medical Humanities curriculum at Rocky Vista University College of Osteopathic Medicine. Beginning in the first semester of Medical Ethics, students engage in critical reflection to explore their own assumptions and biases and how their values impact their practice. This submission is selected and edited by Nicole Michels, PhD, chair of the Department of Medical Humanities, and Alexis Horst, MA, writing center instructor.
Robert English is a fourth-year medical student attending Rocky Vista University in Parker, Colo. He’s originally from Billings, Mont., and completed his undergraduate studies at Carroll College in Helena, Mont., where he studied anthrozoology. Robert is excited to be applying psychiatry for the upcoming match. His professional interests include animal-assisted therapy as well as global medical outreach. In his free time, he enjoys playing disc golf and training his dog, Benny.

In January 2022 I had the transformative opportunity to join a medical mission trip to Kenya. My time there was an amazing and enriching experience that I will treasure for the rest of my life, but it came with several unique struggles that acutely challenged my humanistic values as a provider. While I faced these struggles daily, one patient interaction in particular exemplified this experience in my mind. I met this patient in a remote village, unreachable by bus, where a few of my peers and I had volunteered to camp and host a three-day clinic out of a cinderblock church. She was a Maasai woman, likely in her late 30s, who was presenting for “chest pain.”
All of this was communicated via translators who, while exceedingly kind and eager to help, had very limited English. The translator calmly explained to me that the patient had been living with severe “chest pain” for the past 10 years ever since her husband got upset and “stepped on” her chest. From what I gathered, this woman, like many Maasai women, was a victim of domestic violence. She had chronic chest pain because her husband had thrown her to the ground and stomped on her chest, breaking several of her ribs, which even my novice hands could feel had healed improperly. This information was communicated to me as matter of fact as if they were stating the weather. There was no shame or secrecy. In Maasai society, her husband had been well within his rights to “discipline” her this way.
My heart broke for this woman, who was still required to do heavy manual labor on a daily basis – carrying firewood and gallons of drinking water. Despite this, all I had to offer her was a month of Tylenol and a “referral” to get a chest X-ray at a local hospital that would cost her money out of pocket and likely show nothing fixable after 10 years. There were no social workers, no support systems I could refer her to, nowhere she could go to be safe. These frustrations were recapitulated in so many patient interactions. We felt so limited in our abilities to diagnose and treat common condi tions. We worked with a standard of care that was essentially “take your best guess – try not to do harm.” It became easy to numb oneself to the situation, to get frustrated at “another MSK low-back pain” or the fact that no translator could under stand “does it hurt when you pee.”

In our first week of work, I felt these difficult emotions strongly and the obstacles to providing care hit harder. I worried that I was somehow doing it wrong, that I had missed the memo about how to really help these people. At first, I kept these feelings close, only confiding in my roommate on the trip. I realized in talking with him that my struggles were not so unique, and over the coming days I found these sentiments echoed time and time again among my peers. We were all looking for support, and in the close quarters that we were living, this magnetic force pulled us together. By weeks’ end we had forged into something stronger than our individual selves; we had found our community and we named it “malar one dreams” after the notorious anti-malarial many of us were taking. Whether it was over community meals, singing Disney songs on the bus, or venting late into the night, we kept each other strong and passionate about the work we were doing.
I believe that this collegial support was one of my most valu able takeaways from the experience. Often times, the people who can best remind you why you want to be a physician are the people working by your side. I think it’s incredibly important to keep this in mind, as every specialty in medicine works with patients who can feel unreachable or beyond our help. While this is a universal struggle, I’ve yet to meet a physician who truly works alone. “I want to help people” is the cliché answer to the question “Why do you want to be a doctor?” but I truly believe that it is a core motivator of nearly everyone pursuing medicine. It’s such a simple idea, but I think it easily gets lost in the frustrating minutia of practicing on a daily basis.
I felt these frustrations acutely in Kenya, but I got on the bus every morning excited to see patients because I knew why I was there and was reminded every day. Whether it was excitedly sharing a story about reducing a nursemaids elbow or helping a young boy who’d been kicked in the head by a cow, we reminded each other daily that our purpose was to help people to the best of our abilities. Reflecting on this past year, I’ve learned an incredible amount and grown greatly as a future physician. Some of this I attribute to raw experi ence and exposure, but sharing in my peers struggles as we develop a culture of support and collegiality has fostered my compassion and empathy and affirmed the kind of physician I hope to be. ■
INSIGHT
COVERAGE BEYOND
COPIC Financial Service Group’s team of specialists will partner with you to identify your personal goals and navigate your financial path. We’ll help you determine the best option for everything from paying off student loans to retirement planning. We are here for the long haul for each stage of your career, offering insurance and financial solutions at every step. That’s Value Beyond Coverage.


How a Practice Assistance Program can help physicians with self-care and wellness
Dani Kimlinger, PhD, MHA, SPHR, SHRM-SCP Chief Executive Officer, MINES and Associates
In January 2022, a Medscape physician burnout and depression report published a study that in just one year, from 20202021, burnout was found to have increased among physicians. This study included more than 13,000 physicians. According to the study, more than half of the physi cians shared that their burnout and stress was impacting most areas of their life and that the impact was “strong to severe” and impacting their relationships.
The stress and pressure above and beyond practicing leads to stress, burnout, and exhaustion. Practices face unique pres sures from finding ways to retain nurses and other staff to navigating complex HR laws. The Practice Assistance Program can support CMS members.
Counseling
There are a lot of daily pressures that can cause stress and burnout beyond normal levels that can be difficult to address alone. Reducing these stress levels is critical for your mental health.
A Practice Assistance Program offers free and confidential counseling with licensed mental health therapists to help address stress, burnout, compassion fatigue, and other life situations common within the medical community. A special physicians burnout program is also available to help with more extreme cases with inten sive needs.
Legal/financial
Legal and financial needs can be a huge hassle, especially when juggling every thing else that physicians must think about in any given day.
With a Practice Assistance Program, you would have access to free 30-minute legal
and financial consultations for quick ques tions and quick resolution to basic legal and financial needs. For those bigger and more intensive financial needs, financial coaching sessions are also available that allow you to sit down and discuss your in-depth financial needs with a profes sional financial coach over the course of several comprehensive sessions.
Work/life referrals
The busy day-to-day responsibilities of a physician can leave little time for other things including your personal life and family needs.
Unlimited work/life referrals are a standard part of a Practice Assistance Program and help you find daily services including childcare, eldercare, and other services including restaurants, house cleaners, dog walkers, professional services like plumbers, contractors, photographers, and more to save you time and effort so you can use your personal time for what you really want.
Wellness goals and needs
How can you focus on your own wellness goals when you spend your days helping your patients with their own health and wellness objectives? As a physician, helping people take care of themselves comes as second nature, but that doesn’t mean that you don’t need help from time to time managing your own wellness.
This is where coaching can help! With a Practice Assistance Program, you would have access to hundreds of board-certi fied wellness coaches that can help you set and reach wellness goals, a compre hensive virtual reality, cognitive behavioral therapy program that addresses areas including stress and smoking cessation,
and parenting and lactation coaches to help new and expecting parents navigate the hurdles that come with a new baby. With all these wellness resources, your personal wellness goals no longer have to take a back seat to your practice.
Management/HR
As a physician, you are an expert in a lot of topics and expected to stay current on compliance. Human resources (HR) laws and employee relations can be difficult to stay on top of. This means that while managing your practice, there may be employee and organizational needs that pop up daily that can feel like a minefield to navigate.

We have you covered here, too! As part of the Practice Assistance Program, you would have access to unlimited manage ment consults to talk through important employee and policy issues and work performance referrals to help employees with burnout, stress, substance misuse, or other tough life situations that may be impacting their work. Career coaching is also offered as part of the EAP and can assist, along with conflict resolution services, annual organizational assess ments, and more to take some of the HR burden off your shoulders so you can focus on your patients.
Going forward
If stress, burnout, or lack of HR support is something that you have been seeing in your practice, you don’t have to manage it all yourself. Utilizing a service suite that includes confidential counseling, work/life balance tools, diverse wellness support, and powerful management tools, our Practice Assistance Program offers an integrated suite of services designed to take the pressure off and allow you the
time to focus on your patients, and your self, as much as you both deserve.
Friendly reminder
As a member of the Colorado Medical Society you may purchase robust practice support tools from MINES and Associates, your preferred partner for Practice Assis tance Programs. MINES and Associates’ Practice Assistance Program is designed to support the wellbeing of your practice from the top down to help you address anything from organizational issues to stress and burnout within your team. With MINES as your partner, you would have:
• An employee benefit: Counseling for employees and household members with telephonic, video, and online message-based counseling options. Customizable online platform, legal consultation, resilience, wellness, work/life tools, and more.
• A management support tool: Unlimited management consultations, unlimited work performance referrals, conflict resolution, and an annual organiza tional assessment.
• Telehealth options: Online/telephonic support options for counseling, remote crisis supports for teams and individu als, webinars for live trainings, online physicians burnout program.

Program highlights include:

• Free and confidential behavioral health support service

• In-person, telephonic, video, and online message-based counseling


• Resilience and stress management resources
• Remote and in-person training and crisis support
• Online physician burnout program
To see how MINES can help your practice create a happier and more productive workforce while reducing health care costs, call us at 1-800-873-7138 or visit www.minesandassociates.com ■




Owned and operated by the Colorado Medical Society, and backed by history of physician ownership, MTC is uniquely focused on the needs of its clients. Serving medical professionals is all we do.
MTC’s management team has over 50 years of combined experience in medical answering services. Our operators are professional, friendly, and expertly trained to handle any client situation. We offer a full range of customizable services to ensure your patients enjoy personal, timely communication while you stay on top of your busy schedule.
MTC is committed to providing the highest level of customer service. MTC is a member of the Association of TeleServices Int’l (ASTI) and a proud recipient of the prestigious ASTI Award of Excellence for service quality. MTC continually upgrades its technology and our servers and your data are kept in a secured state-of-the art data center with redundant internet and power supply.
ADEMS, DMS and AAMS host Annual Physician Meet and Greet
Three Denver Metro component medical societies hosted a member meet and greet on Thursday, Oct. 27. Members





enjoyed stunning scenery, appetizers and fun networking at Glenmoor Country Club in Cherry Hills Village. ■
NCMS hosts 2022 Legislative Night

The Northern Colorado Medical Society hosted their annual Legislative Night at The Garden Room in Loveland on Oct. 6. NCMS President Ted Norman, MD, opened the event and introduced presentations by CMS lobbyists Dan Jablan and Jerry Johnson, and NCMS representative on the CMS Council on Legislation Donna Sullivan. NCMS Physi cian of the Year Christie Reimer, MD, moderated a physician panel discussion on prior authorization, scope of practice, stabilizing the liability insurance climate, and behavioral health resources in our region. Executive Director of the Behav ioral Health Services at the Longview Campus Brian Ferrans presented on facil ity updates. The next Colorado General Assembly adjourns Jan. 9, 2023. NCMS thanks the legislators who attended and the sponsors who provided monetary support and raffle prizes. ■
Members of the NCMS Board of Directors and staff attended the event. From left: NCMS
Norman, MD, President-elect Sean Pauzauskie, MD, Executive Director Crystal Goodman, Narina Grove, MD, Treasurer Brianna Money, DO, Marc Breen, MD, Past President Donna Sullivan, MD, and CMS CEO Dean Holzkamp.
CMS election results: Members vote in Mubarak as president-elect
Omar Mubarak, MD, MBA, a vascular surgeon in Denver, was elected Colorado Medical Society president-elect in August and recognized at the CMS Annual Meet ing on Sept. 17. He will spend the year acquainting himself with the duties of the president and supporting leaders and staff in achieving the strategic goals of the society.
Mubarak is a managing partner of his medical group, Vascular Institute of the Rockies. Originally joining as the fourth physician in the practice, he has worked to grow the practice into a leader in vascular care in Colorado. During his year as president, he aims to be an advocate for all CMS members, especially private practice physicians who are finding it increasingly difficult to keep their doors
open. Mubarak is also a member of the Denver Medical Society, a component society of CMS; the American College of Surgeons; the Society of Vascular Surgery; and the American Medical Association.
Re-elected to the AMA Delegation were Dave Downs, MD, FACP; Rachelle M. Klammer, MD; Katie Lozano, MD; and Lee Morgan, MD.
Thank you to all of the CMS members who voted in the 2022 CMS election. Nomi nations for CMS leadership positions for the 2023 CMS election open in January. Voting will again be held Aug. 1-31, 2023. Look for more information in the next issue of Colorado Medicine, on CMS.org and in the ASAP enewsletter. ■

Advocating for Colorado practices: Colorado Medical Society meets with Centers for Medicare & Medicaid Services
The Colorado Medical Society and Colorado Hospital Association were invited to a dialogue session with the federal Centers for Medicare & Medicaid Services. Pictured with CMS Immediate Past President Mark B. Johnson, MD, MPH, CMS Senior Director of Policy Amy Goodman, and representatives from CHA are federal CMS Principal Deputy Admin istrator and Chief Operating Officer Jona
than Blum; and Special Advisor Kristiana Yao, representative of the federal CMS Denver regional office. Those in atten dance discussed our partnership work and issues in Colorado, including recent successes and challenges. The federal CMS sought to understand how they can best partner with CMS to provide innova tive solutions. ■

NCMS hosted welcome for Fort Collins-based medical students


Staff updates: CEO, membership director and program manager
The Colorado Medical Society appointed a new CEO and hired a new member ship director and program manager for government affairs and communications.
Dean Holzkamp was named CMS chief executive officer at the September meeting of the CMS Board of Directors. He previously served as chief operating officer and director of communications, and has been with CMS since 2001. Holzkamp will manage medical society staff who carry out the work of advocacy and government affairs, communica tions, membership, member benefits, and operational excellence. He will also nurture and build relationships with organizations across the state and nation that serve physicians and patients. He invites members to contact him by email
at dean_holzkamp@cms.org or by phone at 303-748-6113.
Cindy Austin was hired as CMS director of membership. Most of her career has been in sales and fundraising for both large and small organizations. Most recently she worked in membership for the largest Presbyterian church in the state where she helped to grow membership throughout the pandemic. Prior to that she worked in sales for a national tutor ing company and locally for the National Foundation for Fertility Research as their director of development. Her managerial experience comes from the American Heart Association where she led a team in a four-state region raising funds and educating students on heart health.
Jennifer Armstrong was hired as CMS program manager for government affairs and communications. Armstrong has a bachelor’s degree in political science and a master’s degree in politics and public policy. She worked in economic devel opment for the cities of Fountain, Colo., and Commerce City, Colo. Most recently she was a policy analyst for the National Conference of State Legislatures (NCSL), monitoring legislative actions, conducting research and producing issue briefs.
These staff members join a small but dedi cated team of professionals committed to championing health care issues that improve patient care, promote physician professional satisfaction and create health ier communities in Colorado. View our full staff at www.cms.org/about/staff ■
Celebrity Cruises





Sail in Modern Luxury from ultra-luxury Celebrity Flora, Celebrity’s 100-passenger purpose-built ship perfect for exploring the Galapagos, to the New state-of-theart Beyond with amazing itineraries and innovative spaces. Gourmet cuisine and the exclusive Retreat— a ship within a ship luxury suite.

Election Day is just the beginning of CMS advocacy
Sean Pauzauskie, MD COMPAC Chair
Election Day on Nov. 8, 2022 capped an intense campaign season during which physicians around the state inter viewed state-level candidates and gave recommendations for the final endorse ments made by the CMS Political Action Committee (COMPAC) Board of Directors.
COMPAC endorsed candidates in 67 statehouse races this year, making some hard calls in competitive races based upon where candidates stand on priorities like protecting a stable liability climate, promoting health care value, and opposing inappropriate scope of practice expansions. Being non-partisan and pro-physician, we are proud to have friends on both sides of the aisle: 52 percent of endorsed candidates were Democrats and 48 percent were Repub licans. We support medicine’s cham

pions and after November’s election many of those candidates will be going to the Capitol, including 88 percent of endorsed candidates in the House and 69 percent in the Senate winning their respective elections.
Heading into Election Day, conventional wisdom and expert insights suggested that Republicans had an opportunity to close the gap in the Colorado House and pick up seats or regain control of the Senate. As you likely already know, the opposite happened. Colorado voters sent a strong message with Democrats in both the Senate and the House now approaching super majority status.
So why do we do all this unpredictable election work? Because it matters. The fact is that passing a bill is one of the quick est and most profound ways to change the way we practice medicine and care
for our patients. And in the coming year, we will face more legislative challenges and opportunities that will have a direct impact on both the lives of our patients and our professional satisfaction. That includes efforts to rein in cumbersome health plan administrative burdens like prior authorizations that sap the joy out of medicine, protecting patients from more unsafe attempts by non-physicians to expand their scopes of practice, and continuing to defend Colorado’s stable medical liability environment.
We fight for these things because quality, safe and affordable patient care is critical. Importantly, if physicians are feeling opti mistic, that the future is bright, that we’re being treated fairly, then that makes us better caregivers. There’s a downstream effect to our and our patients’ wellbeing.
I became involved in COMPAC two years ago because I believe that together we can make a difference for the profession at the state and federal level.
I’m proud of the foundational work we have already done through candidate interviews. I hope you are, too. Now that the election has passed, this is a crucial time to continue relationship-building. I encourage you to reach out to your legis lators to offer your expertise as a physi cian constituent, or let the CMS Govern ment Affairs team know that you want to be involved. You can join me by sharing your stories with your local legislators and with CMS about how proposed legislation will affect you and your patients. While you’re at it, please contribute to COMPAC and the CMS Small Donor Committee.
Now we continue our important work. Thank you for your active participation. ■
So why do we do all this unpredictable election work? Because it matters.