APRIL 2024 www.caremanagementmatters.co.uk The role of digital and AI Retention success Protecting human rights Resource Finder Embracing opportunities Better employee engagement Revisiting Government targets Recruitment SOCIAL CARE INNOVATION Beyond the workforce pathway






Care Choices Ltd 3, Valley Court Offices, Lower Rd, Croydon, Nr Royston, SG8 0HF (01223) 207770 www.carechoices.co.uk Care Information Search for Care Blog Publications Useful Contacts Contact Us Details Features Care Choices is the reliable place to find the care that’s best for you and the information you need. Whether you’re looking for a care home or ideas on staying independent at home, this website has been designed to make it easy for you. ENHANCE YOUR PROFILE TODAY www.carechoices.co.uk 01223 206967 І paul.ocallaghan@carechoices.co.uk * Minimum booking period is 1 year. Price excludes VAT. For full details of opportunities to promote your service on the website, contact us. Promote your service to care seekers for as little as £5.76 per week*
Social Care Insights
David Brindle previews the much-anticipated findings of the Older People’s Housing Taskforce and shares details of a current housing-with-care success story.
Inside CQC
Mary Cridge explains the motivations behind the development of the Care Quality Commission’s dementia strategy.
CMM News
Into Perspective
This month’s Into Perspective explores the potential quality and legal implications of local authorities cutting their adult social care budgets.
Celebrating Excellence
CMM reviews our Markel 3rd Sector Care Awards 2024 ceremony and details all of this year’s winners.
Event Preview
The National Care Association (NCA) previews its National Conference on 9th May 2024 – an informative event with guest speakers and interactive panels.
What’s On?
Straight Talk
Is Advance Care Planning fit for purpose? Professor Heather Richardson provides her response.


In this issue



Beyond the workforce pathway: Innovating the future of social care
Kathryn Smith looks beyond Government’s recent care workforce pathway, focussing on innovation as a vehicle for change in the sector.
The role of digital and AI: Enhancing care and embracing opportunities to co-design
Dr Gillian Horne questions how we use digital and AI to enhance care, given the national rhetoric that it has the potential to save staff time and benefit residents.
Foundations for retention success: Building blocks for better employee engagement
Dave Beesley investigates, with research-led commentary, what the sector can do about retaining talent at a quicker rate.
Picking up the pace: Protecting the human rights of people with a learning disability and autistic people
Dr Rhidian Hughes examines Government’s progress towards reducing its reliance on long-stay assessment and treatment provision for autistic people and people with a learning disability.
Resource Finder: Recruitment
CMM profiles leading social care recruitment organisations to support the sector in bolstering its workforce.
CMM April 2024 3
REGULARS
05 07 09 30 46 48 49 50
FEATURES
42 25 20 25 33 39 42 20 33 39
EDITORIAL
editor@caremanagementmatters.co.uk
Lead Editor: Henry Thornton
Content Editors: Aislinn Thompson, Melissa Rumbold
PRODUCTION
Designer: Rebecca Mendil
Director: Lisa Werthmann
Studio Manager: Jamie Harvey
ADVERTISING
sales@caremanagementmatters.co.uk
01223 207770
Advertising Manager: Aaron Barber aaron.barber@carechoices.co.uk
Director of Sales: David Werthmann david.werthmann@carechoices.co.uk
SUBSCRIPTIONS
Sign up to receive the latest magazines and news for FREE. info@caremanagementmatters.co.uk
01223 207770
www.caremanagementmatters.co.uk
Care Management Matters is published by Care Choices Ltd who cannot be held responsible for views expressed by contributors. Care Management Matters © Care Choices Ltd 2024
CCL REF NO: CMM 21.2

CMM magazine is officially part of the membership entitlement of:


@DavidJ_Brindle
David Brindle Social care commentator and Chair, Ambient Support

Jenny Wilde Partner, Acuity Law

@CQCProf
Mary Cridge Director of Adult Social Care, Care Quality Commission (CQC)
@AcuityLaw @geoffreydcox

Geoffrey Cox Managing Director, Southern Healthcare (Wessex) Ltd

Professor Heather Richardson Director of Academic Learning and Action, St Christopher’s CARE @StChrisHospice

@CQCProf
@SCIE_socialcare
Kathryn Smith
Chief Executive, Social Care Institute for Excellence (SCIE)

Dr Gillian Horne Programme Director – Care Services, Rowcroft Hospice @RowcroftHospice

@Cohesiontalk
Dave Beesley
Social Care Talent Director, Cohesion

@RhidianHughes
Dr Rhidian Hughes Chief Executive, Voluntary Organisations Disability Group (VODG)
4 CMM April 2024
CONTRIBUTORS
www.caremanagementmatters.co.uk Are you getting the benefit of the CMM website? Sign up today to start getting more from CMM. It’s FREE for care providers.
SOCIAL CARE INSIGHTS
From David Brindle
David Brindle previews the much-anticipated findings of the Older People’s Housing Taskforce and shares details of a current housing-with-care success story.
Can you remember how you saw in the new year? Jim Leftwich has fond memories. ‘My wife and I danced the night away to Showaddywaddy,’ he recalls. ‘How’s that for living?’
Leftwich is a very happy resident of Hughenden Gardens Village, a 260-apartment development by the ExtraCare Charitable Trust in High Wycombe where a tribute act – Showaddywaddy Elite if you want to book them – ushered in 2024 with their covers of the original band’s own covers of rock ‘n’ roll classics like Three Steps to Heaven and Under the Moon of Love. You probably had to be there.
Judging by his enthusiasm for life at Hughenden Gardens, Leftwich seems to think he has arrived if not at heaven itself, then at something very close to it. As he recently told the opening session of this year’s online Housing LIN Summit, downsizing from a four-bedroom house means he has no garden to do, and no maintenance to worry about, leaving him plenty of time to use the on-site gym. He walks a mile every morning, around the grounds if dry and through the corridors if wet.
The development is one of 20 retirement villages or schemes run by ExtraCare, all offering care services as needed. Advocates of the housing-with-care model see it as key to easing both the care and the housing shortfalls facing the nation, freeing up general housing as it does. But they say that its growth is being
held back by planning obstacles, a lack of enabling legislation and a shortage of funding for provision for people lacking the capital to buy an apartment, but keen to rent.
According to ARCO (The Associated Retirement Community Operators), only 0.6% of people aged 65 and over in the UK live in a community meeting its criteria for an ‘integrated’ scheme, compared to 5.0% in Australia, 5.5% in New Zealand and 6.0% in the US. If provision was increased to support 250,000 people in such schemes, about 2.5%, it claims there would be savings to the NHS and social care of £5.6bn a year.
After years of campaigning, ARCO thought it had achieved a breakthrough last May when the Government launched the Older People’s Housing Taskforce, charged with exploring ways of increasing the supply of specialist housing for people in later life, widening their options and identifying challenges that needed to be overcome. The taskforce was told to report within 12 months and ARCO welcomed the announcement as a ‘watershed’.
As that 12-month deadline fast approaches, however, there are growing fears that the taskforce’s report will be lost in the run-up to the general election and may not be picked up by the incoming administration. There have also been very few indications of what the report will say.
Care Minister Helen Whately was giving

little away when she addressed the Housing LIN Summit, organised by the Housing Learning and Improvement Network, which brings together housing, health and social care professionals. She said she was expecting a strong, well-evidenced report and recommendations. ‘I have seen some of the work in progress. It’s excellent stuff, exactly what we need.’
We shall see. But whatever the strength of direction at national level, it’s vital that local leaders do what they can with existing powers and resources to ensure that housing-with-care is a meaningful option for people. And North Yorkshire is showing the way.
Richard Webb, North Yorkshire Council’s Director of Health and Adult Services, told the Housing LIN Summit that the county was taking a deliberately proactive approach to expanding housing-with-care and now had 28 schemes offering a total of 1,540 apartments.
Anecdotally, though with some emerging hard evidence, the cost of accommodating someone with care needs seemed about a third of that of residential care. In another positive, schemes situated in town centres were helping regenerate communities such as Thirsk and Bainbridge.
Looking ahead, Webb said, why not adapt the model for young adults with care needs? Now there’s a thought. They might not thrill to Showaddywaddy covers, of course…



CMM April 2024 5 @CMM_Magazine #CMMOFFTHEPAGE www.caremanagementmatters.co.uk To subscribe and listen to previous episodes , visit: www.caremanagementmatters.co.uk/podcast kindly sponsored by EPISODE TEN AVAILABLE NOW SUPPORTING THE WELLBEING OF THE HOMECARE WORKFORCE
Brindle is a social care
and
of Ambient Support. Email: david.brindle@ambient.org.uk X: @DavidJ_Brindle
David
commentator
Chair





Welcome to Architecture, the future of care management software, built with Artificial Intelligence at its core. We’re a young start-up with over 20 years experience in the industry, but our very first customer told us that she now saves £1400/week by automating repetative and time consuming tasks by using Architecture. Artificial intelligence is poised to transform the work landscape by automating tasks and processes that previously consumed hours within a matter of seconds. This is not something in the future, The Future is Here, Now! Your All in One - Social Care Platform, Architecture. Get in touch to see our incredible new software platform. Lee Trueman, Health Automated.
AI Digital Health Care Records Real time changes in medication, care intervals etc 9 AI Automated Rostering Allocate runs and appointments by most qualified, trained or experienced carer 9 Biometric Pain & Sentiment Analysis Visual indicators to record and monitor pain management
Visual Medication Identifiers Identify medication by image, with stock control measure’s 9 AI Automated Social Care Management Automated scheduling, task management, invoicing, HR etc 9 FREE Live Tracking & Emergency Alerts GDPR Compliant Internal Messaging & Video Conferencing 9 Compliance & Financial Monitoring All party transparency on care provision including Family app 9 Plus much more.... Don’t forget to ask about streamlining your recruitment process with Social JobFindr Web: healthautomated.online Email: general@healthautomated.online Book A Call Q. What would you do if you could free up more time? A. Grow your business? Be More Profitable? Less Administration = More Paid Work.
9
9

Mary Cridge, the Director of Adult Social Care at the Care Quality Commission (CQC), explains the motivations behind the development of the regulator’s dementia strategy.
Dementia, according to statistics from Alzheimer's Research UK, will impact on one in two of us over our lifetime, whether that’s caring for someone with the condition, or by developing it ourselves. It’s forecasted that the number of people living with dementia will increase significantly over the coming decades, from just under 950,000 now, to an estimated one million by 2030, reaching 1.6 million by 2050.
At CQC, we’re just beginning the development of a dementia strategy. We’re ambitious in our aims. Our cross-sector strategy will be shaped by this central question – how can CQC use its role to improve the experience of using health and social care services for people living with dementia and their carers?
We want our work to influence and drive improvement to the provision of services, models of care and quality of health and care services which people living with dementia and their carers may need.
We’ve started our work on this and are committed to working closely with a range of partners across the health and social care sectors. I was delighted to kick this off at the end of February with a group of adult social care trade associations representatives. Together we discussed and explored what ‘good’ looks like in dementia care.
It was a rich and wide-ranging discussion and it’s clear that our ambition in this space is shared and welcomed by many. The trade associations had, in many cases, already sought views on this subject from their members, and my thanks go to those of you who share your views with us via routes like this.
INSIDE CQC
Mary Cridge
There is such determination to improve the landscape for those living with dementia and their carers. I left our first workshop inspired by the commitment of providers, not only to support those living with dementia now, but to look to, and plan for the future.
There was vibrant discussion about intersectionality, diversity in care provision and how to properly support people who develop dementia alongside other existing disabilities or conditions. Conversations centred around system challenges and how to support and develop understanding of dementia among families and the wider public. The need for the person to be at the centre of their care plan, with care dedicated and tailored to them and their own story and life experiences was clear.
The first phase of our project involves speaking with a range of stakeholders, including, of course, people with lived experience of dementia and their carers. We are committed to delivering this strategy through consultation and co-production with people and with providers, academics, advocacy groups, statutory bodies and charitable organisations.
The discussions we’re having will build on the significant information and data we collect through our regulatory work. Our data and insight colleagues’ work on reviewing the feedback on care returns we receive has illustrated some of the challenges faced by carers in navigating both primary and secondary care on behalf of the person they are supporting. All this comes together to help articulate that definition of what good looks like.
This is just the beginning of our work. As we develop our strategy, we welcome your feedback and engagement in our central question – how can CQC use its role to improve the experience of using health and social care services for people living with dementia and their carers? Please share your thoughts, experience, ambitions and innovation with us via our dedicated inbox, dementiastrategy@cqc.org.uk
What are you hoping to see from the regulator's dementia strategy? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts.
CMM April 2024 7
is the Director of Adult Social Care at the Care Quality Commission (CQC).
providerengagement@cqc.org.uk X: @CQCProf
Mary Cridge
Email:
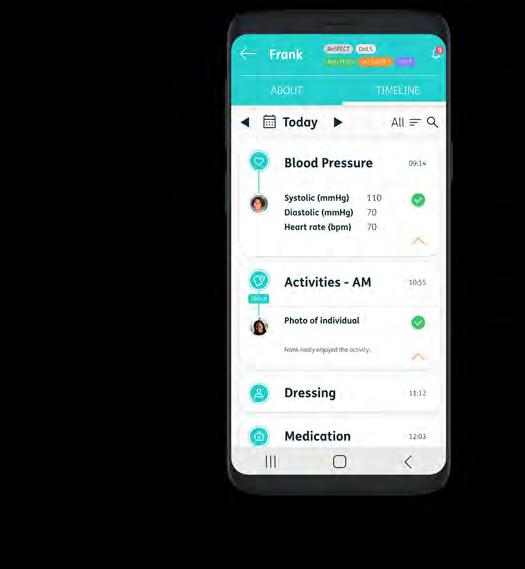
Do you want to know more about how impactful digital journeys are?
Come & chat to us to learn more about how our Connected Care solutions can enhance your staff & resident experience!
Care Planning
Medication Management (eMAR)
Wellbeing & Activities
Care Home Operations

Scan me! PERSONCENTREDSOFTWARE.COM

London 24th – 25th
Find us at Stand G40
The Care Show
April
Sector responds to Spring Budget
Leading voices in the sector have responded to the Spring Budget, delivered by Jeremy Hunt, Chancellor of the Exchequer, on Wednesday 6th March.
The focus of the Spring Budget was on reducing personal taxation, despite consistent polling from Ipsos showing that healthcare is the primary issue that will decide the public’s vote at the next election – ahead of inflation and the wider economic situation.
The Chancellor confirmed a ‘landmark public sector productivity plan’, funded by £3.4bn, which will create a more productive NHS and a £2.5bn allocation to the NHS in England for 2024-25.
"This budget is yet another demonstration of this Government undermining its pledges to deliver adult social care reform."
Whilst widely welcomed by the sector, it has been quick to highlight that the relationship between health and social care was overlooked in the Spring Budget. Leading voices have outlined that investing in social care will allow people to have their needs met in the place they call home and reduce pressure on the NHS.
Vic Rayner, Chief Executive Officer at the National Care Forum (NCF), said, ‘This budget is yet another demonstration of this Government undermining its pledges to deliver adult social care reform. We are struck that we have gone from a position where there was a dedicated Health and Social Care Levy to “fix social care once and for all” in 2021, to one where National Insurance has been cut by 4p in the space of a year.
‘There is very little regard to the long-term sustainability of public services in this budget and it is therefore disappointing but not unexpected that there are no new announcements for adult social care. The cost of delivering these pre-election tax cuts will constrain public spending for several years.’
Professor Martin Green OBE, Chief Executive
Officer of Care England, said, ‘Our sector continues to move ever closer to a cliff edge. We all want good-quality care for our loved ones –now we need those in Government to care.
‘Adult social care is an essential service to the public. The cries of our sector have fallen on deaf ears. A stable adult social care system is vital to the health of the NHS, but this relationship is clearly not appreciated.
‘Care services are vital to local economies and employment opportunities, but this has also been overlooked. This was the Government’s last chance saloon to deliver on its promise but with no long-term commitment to funding the system, the situation grows increasingly perilous.’
Independent Care Group (ICG) Chair, Mike Padgham, said, ‘Once again hundreds of thousands of people who currently can’t get care and the many thousands who work tirelessly delivering care, have been cruelly betrayed.
‘A lack of measures to help social care will undermine and potentially destroy the actions announced to support the NHS as one cannot function properly without the other.
‘Today there was an opportunity to be bold and go down as the Chancellor who acted on the crisis in social care and began the process of creating a National Care Service for the country.
‘Instead, the sector was ignored once again and the crisis will deepen, letting down thousands of older and vulnerable adults and damaging our ability to work hand in hand with the NHS to create cradle-to-the-grave help and support.’
Karolina Gerlich, Chief Executive Officer at The Care Workers' Charity, said, ‘While we were pleased that the much-anticipated drop in public spending did not come to pass, simply maintaining the current funding level falls short of adequately addressing the growing demands of both health and social care.
‘As we advocate for comprehensive reforms, The Care Workers' Charity emphasises the importance of acknowledging, valuing and meeting the distinct needs of both health and social care sectors. We are eager to collaborate with policymakers and stakeholders to ensure that the care workforce is valued and well supported, and all individuals receive the high-quality and inclusive care they deserve.’
APPOINTMENTS
Association for Real Change (ARC)
The Association for Real Change (ARC) has announced the appointment of David Sargent, Chief Executive Officer at Real Life Options, as Chair of its Board of Trustees. David brings a wealth of leadership and learning disability, autism and social care experience to the role. David will steer the organisation towards its strategic aims: changing thinking; changing practice; and changing lives. ARC has expressed its thanks to outgoing Chair, Phil Morris, Chief Executive Officer at Havencare.
Bluebird Care
A Huntingdon-based care provider has welcomed new franchise owners who have over a decade of experience providing at-home care to local communities. As their Newmarket and Fenland, King’s Lynn and West Norfolk, Cambridge and Bedford services all celebrated their 10-year anniversary in 2023, Bluebird Care franchise owners Carolyn and Keith Dailey were set on ensuring the future of home care across the region with their new move into Huntingdon.
Age Connects Cardiff and the Vale
Longstanding older persons' charity, Age Connects Cardiff and the Vale, has welcomed its new Chief Executive Officer, Maxine Johnson. Maxine replaces the charity’s outgoing leader, Jeff Hawkins, who has retired after 37 years’ service. Prior to this appointment, Maxine worked as Head of Wales at Cruse Bereavement Support, involved in the provision of compassionate and professional support to people who are grieving. Maxine also has 20 years’ experience working in the third sector.
CMM April 2024 9 NEWS
Latest findings from the SC-WRES report
Skills for Care has published a report detailing the latest findings of its Social Care Workforce Race Equality Standard (SC-WRES) report.
The SC-WRES is an improvement programme which has been designed for social care organisations to achieve anti-racist workplaces. It comprises nine benchmarks which organisations can use to measure the experiences of people from minoritised ethnic backgrounds, develop action plans from the findings and make improvements.
The SC-WRES draws on a clear improvement methodology that's been well tested in the NHS and adapted for social care and sets the direction to achieve meaningful and sustainable organisational change.
This latest report uses data collected from 23 local authorities between September and November 2023. The data collected about minoritised ethnic colleagues was compared with the data about white staff.
This information was then used by the local authorities to create action plans to
address what emerged with short-, mediumand long-term measurable goals.
Key headlines from the report suggest that overall staff from ethnic minorities are more likely to experience a disadvantage across most of the SC-WRES indicators compared to their white colleagues.
The data found that compared to staff from a white background, staff from a Black, Asian and minoritised ethnic background, in the last 12 months, were:
• Half as likely to be appointed from a shortlisting.
• 40% more likely to enter the formal disciplinary process.
• More than twice as likely as a regulated professional to enter the fitness-topractice process.
• 20% more likely to have experienced harassment, bullying, or abuse from people who use social care, relatives, or the public.
• 30% more likely as a colleague and 90% more likely as a manager to have
experienced harassment, bullying or abuse from colleagues and managers.
There was also a smaller proportion of staff from a Black, Asian and minoritised ethnic background in the senior management compared to the overall workforce.
Oonagh Smyth, Chief Executive Officer at Skills for Care, said, ‘The social care workforce is one of the most ethnically diverse in England, where ethnic minority staff make up 23% of the workforce, making it more diverse than the overall population.
‘Yet we know from multiple reports that experiences of people from ethnic minoritised backgrounds working in social care are not always positive, and we know from our own data that the diversity of the workforce isn’t reflected at a senior level.
‘The SC-WRES is a vital step forward in making measurable and authentic change, and I'm proud that Skills for Care will be leading on the next steps of this important work.’
To read the latest findings from the SC-WRES report, visit the Skills for Care website.

10 CMM April 2024 NEWS
Study investigates impact of COVID-19 restrictions
Visit-id: a study of care home visiting arrangements during COVID-19, a study conducted by the Care Policy and Evaluation Centre (CPEC) at the London School of Economics and Political Science (LSE) with Care England, investigated the impacts of visiting restrictions on the wellbeing and autonomy of care home residents and how to best support them and their family carers.
The study, Visit-id: a study of care home visiting arrangements during COVID-19, was funded by the National Institute of Health and Care Research (NIHR) Policy Research Programme. As part of this study, researchers undertook interviews with 27 family carers with relatives in care homes in England during the pandemic. The study aimed to draw practical lessons from how visiting restrictions were implemented and affected residents to inform future public health emergencies.
In the early phases of the pandemic, policymakers had little existing evidence to guide them. Family carers described how, initially, they placed trust in the national guidance, believing that, at that time,
visiting restrictions were in residents' best interest. However, respondents said that they later felt confused by inconsistencies, including perceived differences between Government announcements and care home practices, conflicting advice from local organisations and even being told different things by staff in the same care home.
Also, while some care homes were clear with families about what the national rules said and how they were interpreting these in practice, many respondents were unsure about how much freedom care homes had, which added to confusion.
The restrictions, designed to stop COVID-19 from spreading, had unintended effects. For care home residents, many with dementia, their wellbeing and autonomy often depends on support from close relations as well as staff. Being apart during the pandemic, for example, meant that family carers could not check on their relatives' health as usual or help with meal times or staying mobile. In some cases, respondents believed that this had led to weight loss, loss of mobility, and greater
chance of falling. It was also harder for family carers to work with staff to help identify their relative with dementia’s emotional and physical needs and devise appropriate care strategies.
Josie Dixon, Assistant Professorial Research Fellow at CPEC and the paper’s lead author, said, ‘The autonomy and wellbeing of care home residents depends significantly on relational support, not just from care staff but also families and others. Supporting the whole network of relationships around the resident is critical for averting possible harms from infection control measures and restrictions. Our paper draws on the first-hand accounts of family carers to make practical suggestions about how support can be enhanced in future; through excellent communication about restrictions, optimising how digital technologies are employed, identifying and adapting to specific needs and family-centred approaches to care.’
The findings of the study, Visit-id: a study of care home visiting arrangements during COVID-19, have been published in Ageing and Society

NEWS CMM April 2024 11






12 CMM December 2023 SOLD SOLD SOLD SOLD SOLD SOLD CARE GROUP Midlands Registered for 224 Nursing & residential Purpose built PARK HOUSE NURSING HOME Nottingham ALEXANDER HOUSE Midlands CAPEL GRANGE CARE HOME Kent SHERBOURNE GRANGE West Midlands MELBOURNE HOUSE East Midlands Due to huge demand, we urgently require care homes throughout the country, contact our Managing Director Nick Greaves in confidence on: nick@ngacare.co.uk 07943 107 887 ngacare.co.uk Your Business is Our Priority GET IN T OUC H
Call to freeze prescription charges
An open letter asking the Minister for Primary Care and Public Health to freeze prescription charges for 2024 and 2025 has been handed to the Department of Health and Social Care by campaigners.
The letter, led by the Prescription Charges Coalition, which represents over 50 organisations, has been backed by over 600 members of the public.
Campaigners have called for the prescription charge, which is currently £9.65 per item, to be frozen as people living with long-term health conditions in England are being forced to choose between heating, eating and taking their vital medication. Prescriptions are free in all other nations of the UK.
Laura Cockram, Chair of the Prescription Charges Coalition and Head of Campaigns at Parkinson’s UK, said, ‘Living with a long-term health condition or disability often adds to the cost of living. Many need more heating to stay well and extra electricity to power assistive
technology devices.
‘We are deeply concerned that a further rise in the charge this year will lead to people skipping or not taking the full dose of their medication, and we fear this will have a negative impact on their health and put more pressure on the already under pressure NHS. Ultimately, the UK Government needs to review the unfair exemption list.’
In 2023, research from the Prescription Charges Coalition found that nearly 10% of respondents had skipped medication in the past year due to the cost of prescriptions and this increased their physical and mental health problems, as well as impacted the time they took off work.
Professor Kamila Hawthorne, Chair of the Royal College of GPs, said, ‘The last thing that some of our most vulnerable patients, who are often living with chronic, long-term health conditions, need is greater financial burden at a time when rising cost of living is already making their lives – and living
healthily – so difficult.
‘Many patients already report struggling to pay for their prescriptions, yet if they don’t take their medication their conditions are going to worsen. We need to guard against this and ensure that those in need are protected, otherwise we’ll see existing health inequalities widen even more.’
Tase Oputu, Chair of the Royal Pharmaceutical Society in England, said, ‘Nobody should face a financial barrier to accessing the medicines they need. Prescription charges are a stealth tax on health and increase the risk of avoidable hospital admissions, adding further pressure to the health service.
‘The prescription charges system is confusing for patients and creates unnecessary bureaucracy for pharmacy teams who want to focus on patient care. Amid a cost-of-living crisis, I would urge the Government to freeze prescription charges this year and commit to abolishing this complex and unjust system.’
Research highlights apprehension regarding later life care
A recent Opinium survey, commissioned by care provider, Loveday, engaged 2,000 participants, revealing insights into the concerns and preparations associated with caring for loved ones and personal planning for the later stages of life.
According to Loveday, the onset of the new year sees a surge in care home enquiries, driven by multiple factors. This includes heightened awareness of failing health noticed by the family members over the holiday period, first-quarter financial planning, new year’s resolutions and the impact of the colder weather accentuating the need for additional care requirements.
"These statistics underscore the pressing need for compassionate and comprehensive support in later life, encompassing physical and emotional needs and independence."
Loveday consistently sees an increase of 10-20% in enquiries throughout January and February compared to the rest of
the year. With every enquiry comes a level of understandable uncertainty when considering care requirements for a loved one, Loveday reports. The Later Life Care Survey sought to dispel common myths, educate on some of the key barriers hindering the decision-making process for seeking care and reduce the anxiety and fear of arranging care.
83% of UK adults surveyed expressed concerns about placing a loved one or dependent into care. Quality of care was a significant worry for 61% of respondents, while 49% were apprehensive about the financial implications. 33% admitted they would feel guilty about making such a decision and one in 10 people worried about how to bring up the subject of care with a loved one.
32% of respondents believed that the quality of care homes in the UK is poor, while only 18% considered them good. Only half of the surveyed individuals (50%) deemed care homes to be adequate, however, perception and reality are very different with CQC rating being far better than thought.
James Cook, Managing Director at Loveday, said, ‘The public perception about the standard of care homes in the UK is very different to reality. In fact, 79% of care
homes in the UK are rated Good and 3.5% are rated Outstanding by the Care Quality Commission (CQC). Many care homes are delivering exceptional care and services, and they should be praised for their efforts.’
The survey found that 93% of UK adults questioned fear the ageing process with top concerns including declining health (61%), dementia and loss of mobility (both 55%). Women (63%) were more worried about dementia than men (48%) and nearly half (48%) were anxious about losing independence, while 43% fear the passing away of friends.
Darren Pitcher, Care and Quality Director at Loveday, said, ‘These statistics underscore the pressing need for compassionate and comprehensive support in later life, encompassing physical and emotional needs and independence. The profound fear of ageing, especially concerning declining health and dementia, speaks to the emotional challenges individuals face throughout the ageing journey.’
Loveday hopes that the findings of its survey highlight the importance of initiating open conversations, increasing education and expanding accessible resources to empower individuals in navigating the complexities of later life planning.
CMM April 2024 13 NEWS
ICO inviting people to share views
The Information Commissioner’s Office (ICO) is inviting people with experience of growing up in the UK care system to share their views. Specifically, the ICO is hoping to hear from people to share the challenges they have faced when accessing their care records from organisations.
With a survey launched this week, the UK data protection regulator is committing to improving the support it provides to both people who grew up in the care system in the UK and the organisations that hold their information.
"As the UK data protection regulator, we want to empower people to exercise their rights over their own personal information..."
The ICO recognises that records of personal information are especially important to people who have care experience, often revealing elements of their
childhood history which they cannot recall. Under data protection law, everyone has rights over their own personal information. This includes the right to ask for this information using a subject access request (SAR) but, for people with care experience, this can be a lengthy process.
Last year, the ICO ran workshops with organisations who support people with experience in the care system. The workshops identified that accessing care records is a significant issue with long delays, heavily redacted records and challenges accessing support. The insight revealed that organisations can struggle to understand what information they can release from complex records and often fail to treat these requests with the sensitivity they require.
It also highlighted that the regulator could do more to help people with care experience obtain their personal information and exercise other information rights, as well as support organisations to provide timely responses.
In response to the concerns raised, the ICO is now urging people with care experience in the UK to come forward to share their
experiences of requesting their records and having their personal information handled in the care system. The information gathered about the impact of delays, redactions and other concerns will help the ICO identify areas where it can focus its support.
Catherine Evans O’Brien, Head of Communities at the ICO, said, ‘Accessing care records can be an emotive and personal subject, as the information can play a huge role in helping someone to understand their identity. As the UK data protection regulator, we want to empower people to exercise their rights over their own personal information and we want to improve the support and resources we provide to help people understand these rights.
‘This survey is a major step towards improving the experience of accessing personal information for people who have been in the care system. As well as experiences trying to access records, we want to hear about any concerns people have about how their personal information has been used, so we can understand where we can make the most difference with our support.

14 CMM April 2024 NEWS Study online to gain an MSc Dementia Studies or MSc Gerontology and Global Ageing Our unrivalled expertise in dementia and ageing will help you expand your knowledge, support your professional development and advance your career prospects. • Study online and part time, to fit your studies around your professional or family commitments • We are home to the internationally renowned Dementia Services Development Centre
Gain skills required for roles within healthcare practice settings, informal support settings, policy or business areas associated with ageing populations or undertake further research STUDY
MASTERS IN DEMENTIA AND AGEING Find out more: study@stir.ac.uk
•
A
Cera launches Academy Career Pathway
The home care provider, Cera, has announced its commitment to the learning and development of carers, investing over £5m in the launch of its Academy Career Pathway.
Cera’s Academy Career Pathway aims to facilitate the progression of carers by enabling employees to gain fully funded and professionally recognised qualifications alongside their current work. The pathway is split into two streams – development opportunities for skilled carers and middle management, and an apprenticeship pathway for early-career carers and operations staff.
In pilots, 245 Cera employees have enrolled on the programme choosing from up to 50 different training options ranging from Level 2-5 care qualifications, skills to support complex or learning disability care and supervisory or management positions.
As part of its Carer Value Proposition, Cera is formally endorsed as a training provider by Skills for Care. With many of its carers joining with no previous experience or being relatively new to the industry with a desire to qualify, Cera has seen growth in
registration for its Level 2 Adult Social Care apprenticeship. Recent data has shown that there has been a 150% increase in Cera carer registrations for the course since 2023.
Those with more experience and looking to develop their skills further can progress to Level 3 and 4 in Adult Social Care via Cera’s pathway. This enables progression into the more senior Field Care Supervisor and Care Co-ordinator roles, unlocking higher pay bands via new management positions and greater responsibility.
All carers can reach management positions via progression through Cera's advanced pathway. The higher degree apprenticeship levels of the scheme have seen 65 managers trained to date and a further 100 carers registered for 2024. This year, 16 people are enrolled in the Level 5 Leader in Adult Care programme, where the company supports branch managers with their goal to move into higher management roles (i.e. Registered Manager with CQC). From Q4 2023 to Q1 2024, Cera saw an 82% increase in the enrolment of managers.
Training is also available for those beyond
care and central operations. Cera provides opportunities for employees to explore interests in other areas of the business, with its Recruitment and Finance teams completing training in Digital Marketing and Accounting areas.
Dr Ben Maruthappu, Founder and Chief Executive Officer of Cera, said, ‘In the NHS and social care, turnover rates for staff have always been notoriously high, and a huge driver of this is a lack of a clear progression. While it’s positive to see the Government finally take a stance with its new pledge, we hope that our Academy Career Pathway acts as a model example for other care providers looking to support the professional development of staff in line with the Government’s new pledge.
‘By offering our employees new learning and development opportunities, we are illustrating our commitment to enhancing the quality of social care and offering rewarding careers. The domestic healthcare industry is fuelled by intelligent and driven carers, who deserve new incentives to foster professional growth and overall job satisfaction.’



CMM April 2024 15 NEWS • Life Insurance • Relevant Life Insurance • Shareholder Protection • IHT Planning • Critical Illness • Private Medical Phoenix Specialist Risk Solutions, Office One, 1 Coldbath Square, Farringdon, London, EC1R 5HL PHOENIX SPECIALIST RISK SOLUTIONS Phoenix Specialist Risk Solutions Ltd are authorised and regulated by the Financial Conduct Authority – FRN: 992540. HAVE YOU GOT COVER? Call 01273 977221 or visit: www.phoenixsrs.co.uk


HEAR4ALL is a service dedicated to excellent hearing care for residents of care homes.
We offer a complete service, from professional earwax removal and routine hearing tests, to the provision of hearing aids and other technologies to support residents with their hearing health. www.hear4all.org


16 CMM April 2024
enquiries@hear4all.org | 02382 444 045 Meet us on STAND J20 24th & 25th April at Care Show London
Person Centred Software partnering with CommonAge
Person Centred Software has announced a partnership with CommonAge, The Commonwealth Association for the Ageing. Person Centred Software delivers integrated care home solutions and CommonAge is a charity dedicated to ensuring older people are fully recognised and supported to live well in an all-age-friendly Commonwealth.
Person Centred Software will actively contribute to CommonAge's initiatives to encourage a society that values and respects older individuals, ensuring they are supported and cared for.
CommonAge promotes and advocates for the needs and rights of older people through its activities and networks. By partnering with CommonAge, Person Centred Software reinforces its own commitment to supporting the wellbeing and quality of
life of older individuals.
Tammy Sherwood, Chief Customer Officer at Person Centred Software, said, ‘We are proud to support CommonAge in driving positive change in how we support older people. Their advocacy work makes a real difference in the lives of older individuals across the Commonwealth.’
Mansur Dalal, Chair of CommonAge, said, ‘With over 10 years of impact, we are absolutely thrilled to have Person Centred Software as a dedicated and innovative partner in our journey.
‘Now more than ever before, it is vital we come together, sharing knowledge and experience, to find workable solutions to ensure older people in all Commonwealth countries, and indeed the world, are recognised and supported to enjoy the highest possible quality of life.’
National provider boosts residents’ income
Over 3,500 Anchor residents have been supported to gain an average income boost of £8,000 each. Residents have gained an estimated combined total of more than £6m over the financial year.
Through its Be Wise service, Anchor offers free and impartial advice on benefits, energy bills, budgeting, income and expenditure, basic debt management advice and easing cost-of-living pressures. A Resident Support Fund has also helped residents to buy food, pay energy bills and purchase home essentials.
Gordon, an Anchor resident, said, ‘I was receiving a state retirement pension of £184 per week and a small private pension of £18 per week.
'I contacted Be Wise and they awarded me £100 towards my energy costs and £60 towards food from the Resident Support Fund. My Housing Benefit and Council Tax support had stopped, and I was fearful I would lose my home.
‘They completed a full benefit check and made an application on my behalf for Attendance Allowance, which was awarded at the lower rate of £68.10 per week, and in addition this meant I received Pension Credit of £27 per week, which also led to the cost-ofliving payment of £300 and the Warm Home Discount payment of £150. My Housing Benefit and Council Tax support were reinstated back to when they stopped at full eligibility.’
Age UK report reveals failing DoLS system
WHAT’S THE STORY?
In a new report, A Hidden Crisis, Age UK has shed light on what it believes to be the failing system for providing proper legal protection for older people who have lost their mental capacity, often due to dementia, and who are believed to need to be deprived of their liberty for their own safety.
A Deprivation of Liberty Safeguards (DoLS) provides a set of checks to ensure that the deprivation of liberty is in the person’s best interests, is necessary to prevent harm to them, and is a proportionate response to the likelihood and seriousness of that harm. But, despite the existence of these protections, according to Age UK, DoLS is not working well in practice and for a large proportion of older people, is not working at all.
WHAT WERE THE FINDINGS?
Since 2015/16 the estimated number of incomplete DoLS applications has remained at over 100,000, and in 2022/23 126,100 applications went uncompleted. Where applications were completed, in 2022/23 it took an average of 156 days for a standard authorisation – longer than the statutory timeframe of 21 days.
According to the report, in many cases, the decision to constrain the individual’s freedom for their own good would have probably fulfilled
the DoLS criteria, but within such a huge number there must be a risk of injustice for some individuals, whose lawful right to liberty will have been inappropriately denied. The Local Government and Social Care Ombudsman has also identified instances where local authorities have effectively adopted a policy of not even trying to deal with large numbers of low- and medium-priority applications.
The problems with DoLS particularly affect older people –84% of people subject to a DoLS application in 2022/23 were aged 65 years or over. Furthermore, in 2022/23, 49,325 people died while waiting for their DoLS application to be dealt with.
WHAT DO THE EXPERTS SAY?
Caroline Abrahams CBE, Age UK Charity Director, said, ‘Personal liberty is part of our birthright and central to our understanding of what it means to live in a democracy, so it is profoundly shocking that so many older people with diminished capacity are living and dying without the proper legal protections for limiting their freedoms being in place.
‘As a result, we risk the nightmare scenario that somewhere, there’s an older person locked in their room in a care home, supposedly in their own best interests when, in practice, an objective assessment by a trained social worker would have found this not to be justified at all.’
CMM April 2024 17 NEWS IN FOCUS NEWS / IN FOCUS
FROM ACROSS THE GLOBE
Global palliative care market
According to GLOBOCAN, in 2020, there were approximately 10 million deaths from cancer and 19.3 million new cases, while the World Health Organization (WHO) estimates that 40 million individuals require palliative care. There will be an ever-increasing global demand for palliative care as the number of patients with terminal conditions continues to rise.
According to the Center to Advance Palliative Care (CAPC) the global palliative care market size was valued at $12.74bn in 2022.
It is estimated to reach $25.68 billion by 2031, growing at a compound annual growth
ascends
rate (CAGR) of 8.1% during 2023–2031.
The Americas is the most significant shareholder in the global palliative care market and is anticipated to grow at a CAGR of 8.2% during 2023–2031. In 2019, 72% of hospitals in the United States had a palliative care team, which was up from 67% in 2016
and 7% in 2001.
Europe is anticipated to experience a CAGR of 9.3% during 2023–2031. According to Eurostat, 20.6% of the European Union's population was 65 or older in 2020. The prevalence of chronic diseases among older adults increases the demand for palliative care.
EU funds new €3.1m social care programme in Albania
The European Union (EU) has launched a new ‘EU for Social Care’ programme in Albania. The programme is funded by the EU and implemented by UNICEF Albania and World Vision, in partnership with the Ministry of Health and Social Protection in Albania.
The project will support 14 municipalities, for a period of
36 months, to establish and expand social care services to address the needs and rights of vulnerable groups in Albania, such as children with disabilities, women at risk and young people in difficult situations.
This project is expected to reach 6,000 at-risk families and 350 professionals and
frontline workers in social care – through social care services, innovative practices and support with tailored training and mentoring. All of the EU for Social Care programme’s activities and actions have been designed to respond to the EU’s integration requirements for the country.
Aiming to establish

different typologies of social care services, the programme also sets out to promote volunteerism and engage young people and students.
The programme launch was attended by the Minister of Health and Social Welfare, Ms. Albana Koçiu, EU Ambassador, Mr. Silvio Gonzato, and UNICEF representative, Mr. Murat Sahin.
Agreement on European Disability and Parking Cards
The European Commission has welcomed the political agreement reached between the European Parliament and the EU Member States on the Directive establishing the European Disability Card and the European Parking Card for persons with disabilities.
A harmonised European Disability Card and the improved European Parking Card will ensure easier recognition of disability status and equal access to special conditions and preferential treatment across the EU, during short-term stays in
other EU countries. These cards will facilitate the mobility of persons with disabilities. No matter if you are a cardholder in Spain traveling in Poland or a Polish resident, the card will guarantee access on the same terms.
The main elements of the Directive include:
• Recognising the European Disability Card as proof of disability across the EU.
• Providing European Parking Card holders with the same parking rights across the EU.
• Requiring Member States to issue and renew the European Disability Card and European Parking Card free of charge, in both physical format (with digital features) and in digital format.
• Ensuring publicly accessible information on the conditions and procedures for obtaining these cards.
• Guaranteeing enforcement and compliance by empowering persons with disabilities and their representatives to take legal

action under national law.
After the formal agreement by the European Parliament and the Council in the coming months, the Directive will enter into force on the twentieth day following its publication in the Official Journal of the European Union. Within 30 months after the entry into force, Member States will have to incorporate the provisions of the Directive into national law.
One year later, the legislation will take effect, at which point persons with disabilities can apply for the cards.
18 CMM April 2024 NEWS NEWS NEWS
NEWS
Beyond the workforce pathway: innovating the future of social care

Government’s recently announced care workforce pathway is a welcome step towards addressing workforce issues. But what else can be done? Kathryn Smith, Chief Executive at the Social Care Institute for Excellence (SCIE), looks beyond the pathway, focussing on innovation as a vehicle for change.
The current landscape
With more than 11 million people in England and Wales aged over 65, social care has never been so important in maintaining people’s health, wellbeing and quality of life. For too long, however, the sector has faced an uphill struggle to provide the level of care that people need due to challenges relating to staff shortages and poor pay and working conditions.
In England alone, there are around 152,000 vacant adult social care roles. Pay during the last financial year averaged just over £10 per hour. This has a knock-on effect: in August 2023, almost 250,000 adults were waiting for an assessment of their care needs and about 85,000 had been waiting for at least six
20 CMM April 2024

months. Government’s announcement of the new care workforce pathway in January this year was therefore a welcome step forward in acknowledging and valuing the vital role of the social care workforce in society.
First steps
The reforms laid out by the Department of Health and Social Care mean, for the first time, those who work in social care have a structured career path in front of them with better job prospects and access to accredited qualifications. More than £20m will go towards funding apprenticeships while tens of millions more has been pledged to subsidise training places and establish two new accredited qualifications, one for those
working in direct adult social care roles and another in digital leadership.
These are promising developments that we hope will result in building and retaining a more skilled workforce. This should, in turn, increase the quality and timeliness of care for those who need it. We will certainly be watching the development and roll-out of these plans with interest. However, while these first steps are positive, we must ensure that they are exactly that – first steps.
The road ahead
There is still much more to do to make social care a desirable career choice. Low wages have plagued the sector for as long as I can remember, exacerbated over the years by
rising living costs and salaries not keeping pace with inflation. Workers and providers are often overstretched due to increasing demand, particularly as more of us are living longer and often with complex needs and conditions.
Social care can also be complicated to access, and many families choose to, or feel they need to, take on all or some of the responsibility of looking after their loved ones. This has led to a ‘silent army’ of unpaid carers who can often experience exhaustion, stress and burnout.
Plenty of evidence exists describing our social care system as creaking under pressures caused by chronic underfunding and the challenges of recruiting and retaining a skilled, knowledgeable workforce. A career pathway on its own will not solve these >
CMM April 2024 21










22 CMM April 2024 Bookademotoday! eLearning, compliance, and HR management, all under a single login. Trusted by over 5,000 providers and a ¼ of a million trainees. “The platform itself is outstanding in the services and reporting tools it offers, but the customer service is what makes me recommend Blue Stream to others in the care sector; in my experience it is unmatched” System Administrator Newcastle upon Tyne Care Provider Established Management of Information System Fully integrated HR System 120+ CPD-certified eLearning modules Exclusive Discussion Forum for BSA trainees 01773 822549 nch@bluestreamacademy.com LiveChat at bluestreamacademy.com For more information, visit www.painchek.com/uk/ or call 0333 577 3397 ® PainChek provides a fast and reliable way of identifying and quantifying pain for all residents, regardless of their ability to self-report their pain. PainChek’s assessment tool is a clinically-validated medical device that utilises AI and facial analysis technology to give a voice to those who cannot reliably self-report their pain, such as those living with dementia or other cognitive impairment. Enabling best-practice pain management. Over 3.5 million pain assessments completed globally using PainChek®
underlying issues, so how do we create the conditions for these new career roles to flourish?
One obvious change is improving the pay and rewards for care work, but we also need to step back and consider how our future social care system can adapt and expand to meet the pressures it faces. Our view is that innovation in the way we design and deliver services to tackle the sector’s many challenges must play a key role in securing its future.
Tackling challenges through innovation
Done well, service innovation can support people in achieving greater independence, living longer in their own homes and experiencing fewer care crises that result in hospital admissions. For staff, innovation can release more time for care and produce efficiencies, enabling funding to go further and therefore benefit more people.
Our partners in the health sector are already experiencing the difference that innovation can make. The emergence of artificial intelligence (AI) is showing potential in identifying and diagnosing some cancers and other conditions faster and at an earlier stage, for instance. Wearables and digital apps are empowering people to take control of their health and manage their conditions more easily. The development of artificial and bionic limbs can enhance a recipient’s quality of life. Computer algorithms are beginning to predict service demand, track service provision and pinpoint pressure points within the healthcare system.
Government’s Accelerating Reform Fund (ARF), a £42.6m programme for social care, aims to drive forward innovation by, for the first time, funding the scaling up of innovative practice across adult social care and kickstarting a change in support for unpaid carers. This initiative aims to boost the quality and accessibility of social care, accelerating progress towards the social care vision where people have choice, control and support to live independent lives and care and support is of outstanding quality and accessible to all. The Fund is available to all local authorities and will fund at least two projects per region in England.
We will be providing direct hands-on support to ARF-funded projects, helping local authorities to develop partnerships with health and care providers and voluntary and community groups and encouraging co-production with people who need care and unpaid carers. In this way, projects will benefit from shared learning and expert insights so that initiatives are more inclusive and accessible, and we can increase our knowledge of the barriers to innovation and how we can overcome these to scale up and embed new approaches and deliver new models of care.
Government has set out 12 priorities for the ARF to ensure all successful projects place people’s needs at the heart of innovation and ensure no-one feels isolated. These include connecting people to local information, advice and services through social prescribing, using digital tools for workforce recruitment and retention purposes, investigating
community-based models of care and the role of local networks and groups in supporting people to age well and promote wellbeing, and understanding the impact of volunteer-led pathways of care.
A significant element of the ARF will focus on the estimated 4.7 million unpaid carers in England. Caring for your loved ones, either because you want to or cannot afford professional care, can be physically and emotionally draining. Through greater innovation, we want to ensure unpaid carers get the support they need through tailored respite, increased access to carer services and greater involvement in care planning at the hospital discharge stage.
Spreading innovation for better care
In social care, innovation does not need to be radical to make a difference in the way care and support is provided.
The shared Lives service, for example, where people aged 16 and over are matched with a carer, move in with them and receive support within the carer’s own home, is generating cost-savings compared with residential care while promoting greater independence. Our independent analysis found that this can result in an average saving of £8,000 for people with mental health needs and £26,000 for people with learning disabilities.
Meanwhile, simple ideas like Jelly Drops water sweets enable care home staff to easily ensure their elderly residents stay hydrated, freeing up time to spend on other aspects of patient care. Wireless sensors in the home can help track routines and alert families and carers if there has been no activity, and smart speakers and plugs can help people execute simple tasks around the home more easily.
We should always be looking at the way we are providing care and asking ourselves if we are delivering it in the most effective and efficient way. As technology becomes more advanced, new opportunities to streamline and improve care and support will be inevitable, and we must grasp these with both hands.
Government’s planned digital leadership qualification and digital skills training will be key in embracing digitisation and optimising new technological approaches, but we must also be actively evaluating the benefits of digital innovation so that only projects that bring the most benefit are adopted nationally.
Of course, innovation is only good if it ultimately works for people who draw on care and support. With everything we do, we must always seek to understand if and how care will be improved. We will focus our efforts on not only identifying innovation in the sector but also how best to scale and spread the best ideas and practices for the future.
We know that improving career prospects, pay and working conditions of social care workers will build a valued workforce and ultimately benefit those who use these services. However, with a growing and ageing population, many of whom are not currently getting the support they need, these measures must be coupled with more innovative practices that can propel the sector forward now and in the long term. CMM
What innovative methods have you introduced to your daily operations? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts.
CMM April 2024 23
Kathryn Smith is Chief Executive at the Social Care Institute for Excellence (SCIE). Email: media@scie.org.uk X: @SCIE_socialcare
BEYOND THE WORKFORCE PATHWAY: INNOVATING THE FUTURE OF SOCIAL CARE >


24 CMM April 2024 Scan me
THE ROLE OF DIGITAL AND AI :
Enhancing care and embracing opportunities to co-design
Faced with the challenge of designing a brand-new nursing home for people with advanced dementia and complex nursing needs, and given the national rhetoric that digital and AI has the potential to save staff time and benefit residents, Gillian Horne questions how we use digital and AI to enhance care.
My application for a digital fellowship has enabled me to tackle the question of how we use digital and artificial intelligence (AI) to enhance care.
Literature review
Initially, I looked at the evidence to find out what and how digital and AI is used in care home settings. I found most of the 110 articles had only been published in the last five years, and few were from the UK. Of the 21 articles that met the search criteria, I discovered distinct groups of digital and AI technologies that had been tested in care home settings.
These included environmental sensors, wearables, combined digital technologies, social and assistive robots and healthcare data analytics. I also considered some of the ethical issues reported.

> > CMM April 2024 25





The benefits of our software Person Centred Accessible Legible Accurate Up-to-date Always Available Complete Secure WORKFORCE MANAGEMENT & STAFF APP RESIDENT ADMINISTRATION & BILLING CARE PLANNING & TASKS COMPREHENSIVE REPORTING Care Management Software Or upgrade today with ease: +44(0)1989 763131 (Option 2) www.panaway.com Find out more: +44(0)1989 763131 (Option 2) Haigh Engineering Ltd., Alton Road, Ross-on-Wye, Herefordshire, HR9 5NG, UK 01989 763131 – info@haigh.co.uk Reach Net Zero quicker and save £’000s with Panaway ® Bedpan macerators use less energy than washers, costing only £50-£150* compared to £3,000-£5,000 per year. Panaway macerators, from Haigh, are economical, energy and consumables usage available online 26 CMM April 2024
Environment sensors
These include ‘smart’ phones, tablets and speakers, which are used to communicate with loved ones via text, Facetime, WhatsApp and other forms of video conferencing, many of which came into their own during the COVID-19 pandemic. These are also used to play music and audiobooks, to access news and weather reports, or to play games1,2.
Sensors attached to residents’ clothing are used to monitor walking episodes from other types of activity for people with dementia3, while bed and chair sensors with machine learning or air tags with GPS tracking are reported to prevent wandering4 or to identify risk in the prevention of pressure ulcers5. These sensors have also been used to provide real-time in-bed/off-bed status, providing daily records of residents’ sleep quality, prolonged pressure and living patterns.
An AI-Toilet was tested in care homes, monitoring urine and faecal outputs6, and one trial looked at the design of futuristic incontinence wear, using sensors to detect saturation and defaecation7
Wearables
Evidence suggests that wearables can help monitor posture or activity and support early identification of changes in health or mood. Wearables come in different forms, such as smart watches, chest straps, hearing aids, glasses, clothes, shoes, helmets, rings and lenses.
"Virtual reality was reported to enhance residents’ social engagement, enabling residents to virtually leave the home and reconnect with their personal interests, providing entertainment and distraction."
They track activity and location, monitor vital signs and detect falls and stress, hydration, seizures, sleep and arrythmias8. One reported wearable was a smart belt offering automatic airbag deployment, reducing the impact forces to the hip region in serious hip-impact fall scenarios9. Improved communication between residents and staff reduced delays in staff response through smart-watch communication instead of nurse call systems10.
Combined digital technologies
When wearables, sensors and/or apps are combined to exchange data over the internet, they are sometimes known as the ‘internet of things’ (IoT). Several combined digital technologies were evidenced in this review, including ‘Swallowscope’11 to detect swallowing difficulties
and provide remote visual assessment by speech and language experts.
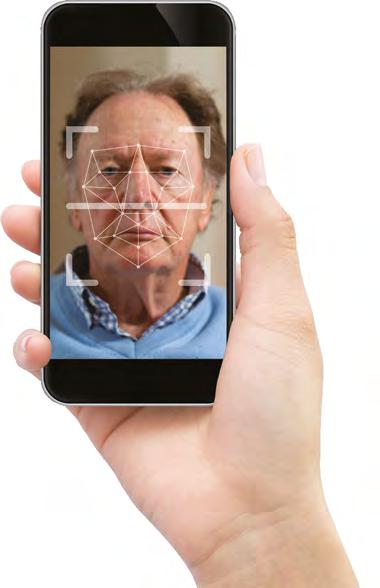
PainChek12 is another example, providing a point-of-care medical application to assess pain in people with dementia by detecting facial expressions on a smart device connected to software that can recognise levels of pain. Telemedicine, sometimes combined with electronic stethoscopes and otoscopes, can reduce the need for hospital attendance or admission and can also enable remote prescribing13, 1 .
Virtual reality was reported to enhance residents’ social engagement14, enabling residents to virtually leave the home and reconnect with their personal interests, providing entertainment and distraction. An AI-enabled smart phone app15 has been developed and evaluated for real-time pressure ulcer assessment, supporting care home nurses who may not have tissue viability expertise to make more accurate assessments. ‘Mindful Garden’16 a/b, a digital screen-mounted garden display of layered motion pictures, helped manage behavioural and psychological symptoms of dementia and reduced bathing time in care homes.
Social and assistive robots
Paro the seal is reported in several papers; it is suggested that this robotic seal calms and soothes residents. Pet robots provide companionship, comfort, entertainment, wellbeing, improved mood and sleep quality, reducing occupational disruptiveness, distress and anxiety and even inducing a sense of being in a close relationship17, 18, 19, 20 .
An assistive service robot named SMOOTH21 has been evaluated for its ability to undertake three separate functions: transporting laundry; guiding residents to follow it; and offering beverages. Further refinement is needed, as each task required staff to input programme changes into the robot’s functions.
Healthcare data analytics
Digital care records are now in place in most care homes within England. They record health and care data, medications administered and may connect to the IoT. These digital records enable healthcare professionals to share important data with other healthcare team members and families; with AI, they can enable us to search, develop, test and learn to predict patterns in residents’ health and behaviour.
Text-mining22 to evaluate the quality of care from narratives in residents’ records and using AI to survey statistical health data can reduce nursing care time. AI has also been used with administration systems to detect frailty and to predict falls23, 24 .
Digital platforms have been developed for ‘shared care,’ co-ordination and care planning for the frail elderly, providing a set of tools centred around an electronic healthcare record24. Alongside this, AI algorithms have been used to prevent and predict pain and subsequent agitation25, support decision making for residents’ care in relation to pressure ulcer management26 and detect patterns of change in behaviour of residents, enabling nurses to investigate and intervene if needed27.
>
CMM April 2024 27 THE ROLE OF DIGITAL AND AI: ENHANCING CARE AND EMBRACING OPPORTUNITIES TO CO-DESIGN
>
Ethical considerations, barriers and enablers
Acceptability by residents and staff is an important ethical consideration in choosing and deploying digital and AI. The potential for deceit and de-humanisation were reported, particularly if automating certain nurse functions20, 28. Residents were more likely to accept the use of digital if family and staff were able to explain the benefits29. Comfort is also important in terms of acceptability for wearables and sensors1
Not surprisingly, consent, privacy and safety were also viewed as important ethical principles. For residents experiencing fluctuating capacity, whether they remembered they were being monitored was considered an issue of psychological safety for them24. Staff perceptions of being monitored were also raised.
The support and training of staff, how easy learning to use digital is and ensuring there is enough IT infrastructure and support, were deemed significant for the successful use of digital and AI. Insufficient resources, staffing, inappropriate devices or apps, ‘sociotechnical ageism’29, limited organisational support and lack of support from families were reported as barriers which impact on the use of digital/AI in care homes.
Some practical issues were raised in this review, such as ensuring sufficient battery power, energy and internet connectivity to run smart devices and servers. Interesting solutions were proposed, including self-sustaining or energy harvesting from human movements over different flooring types and textiles30
Discussion
There are multiple types of digital and AI that have been developed to monitor residents’ wellbeing or support staff, prevent harm to residents, diagnose and predict patterns or behaviours, provide enrichment to the quality of residents’ lives, reduce distress, aid comfort or help with communication and interactions.
However, this literature review found that there is little research on the effectiveness and acceptability of digital or AI deployed in care homes, except around the use of certain pet robots, suggesting this is evolving technology with minimal long-term deployment in nursing homes. There is a need for longitudinal studies to evaluate the impact on residents’ quality of life and staff’s working lives.
The rhetoric that digital can release more time for the workforce to care needs to be carefully considered with each solution developed. Ease of use with minimal maintenance and little need for guidance will be imperative for new digital/AI technologies deployed in nursing homes. Additionally, staff will need training to gain skills and competencies in understanding and using digital/AI; they will be more likely to accept digital
if involved in its design and deployment, supported by the organisation and its culture.
Co-designing with people with experience
Through the digital fellowship, I held a series of workshops with people living with dementia or motor neurone disease, their families and experienced care home workers, to co-design a digital decision-making tool we could use for the nursing home. We established important considerations for digital use in care homes. We turned these important aspects into questions to create a tool for care home managers and others to use in deciding what, if any, digital or AI to use in a care home. The digital decision-making tool will be further tested with other care homes for its use and applicability.
Supporting healthcare and care workers and technical experts to work together to develop robust digital solutions will help to remove perceived barriers and ensure users are included and protected24. I would argue engaging residents and future residents of care homes and their families in the choice of digital is also important for acceptability. We disproved the myth that older people living with dementia and their families would not want to use digital or AI.
Moving forward, safe digital and AI solutions benefitting residents and staff that have been evaluated in ‘live’ care home settings will be important for our future trust and confidence in deploying digital. Finally, care home staff are close to residents and are best placed to see the potential for developing digital and AI to benefit those they care for. Harnessing this knowledge and working with AI developers directly to design solutions that will be useful is the way forward in this evolving digital world.
I’d like to acknowledge the people with experience involved in the co-design workshops and Dr Alison Warren, Associate Professor of Occupational Therapy at University of Plymouth, for their support. CMM

Dr
X: @RowcroftHospice
To view the full list of academic and literary references used to write this article, visit the CMM website. Are you embracing digital and AI in your care setting? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts.
28 CMM April 2024 THE ROLE OF DIGITAL AND AI: ENHANCING CARE AND EMBRACING OPPORTUNITIES TO CO-DESIGN
Gillian Horne is Programme Director – Care Services at Rowcroft Hospice. Email: Gill.Horne@rowcrofthospice.org.uk
>
Supplier Payments Efficiency & Control
All too often we see examples of inefficient purchasing and invoicing processes, with finance teams burdened with collating bundles of paper invoices every month and manually entering the details into their finance system to pay suppliers and produce management accounts.
If this sounds familiar to your invoicing process, then you need to unlock the power of Wippet. Our digital platform, built specifically for care, provides an efficient way to combine all your supplier payments in one place.
One invoice, multiple suppliers. One payment multiple invoices. Using Wippet you save precious time in making payments, only pay for what you have received and capture rich data you can use to improve your procurement time and time again.
Data drives insight and access to fair market prices
Your spend data is key. Using Wippet to manage supplier payments captures vital spend data that is all to often lost. Understanding your spend better unlocks opportunities to buy better.
But its not just your data. The Wippet platform can provide insight from the wider Wippet ‘eco-system’ that gives care operators access to pre-negotiated prices direct from manufacturers and powerful real-time insights to help target opportunities to save.
With 50 suppliers already listed on Wippet we have a proven track record where we have been able to secure savings for care operators in excess of 20%.


Technology & Capability to enhance all aspects of your procurement
The Wippet platform brings an online shopping experience your teams enjoy at home to their workplace. Easy to use and accessible via mobile, tablet and PC 24/7 and supports rapid and hassle-free implementation.
The Wippet platform has been designed by care procurement professionals. We know first-hand how challenging care procurement is; our team is always available to you as and when you need without recruiting additional headcount.
This affordable solution suits any organisation size, with rapid set up and an onboarding process tailored to the speed you want to develop, your organisation can start saving right now!
Goods
Enhanced
Configurable
API
A simple solution to your challenges in care procurement Registered in England and Wales No. 13115709 VAT No. 388834240 | Sunnycroft, Hill Brow, Liss, GU33 7QJ. Wippet Limited Follow us on: /wippet /wippet SERVICES The world’s only care specific, secure curated marketplace. The Wippet platform is a gateway to fair prices direct from known & trusted suppliers for all care operators, no matter how big or small. info@wippet.com www.wippetforcare.com Procurement in Care Today Long contract terms & price creep Procurement teams overstretched Reduced visibility of true costs Limited Access to Manufacturers Lengthyprocurementtimeframes Limited digital tools Excessive hours in repetitive unnecessary tasks Traditional Invoice processing Riskstoresidentcare &safetyLackofcontrol leadingto poor compliance UnfairPricesforcare operators Amazon Business&Distributorsdominance negotiationsLessinformedLackofData& Insight prohibitiveCostofP2Psystems formany DigitalCarebased Agenda AccesstoFairMarketPrices Insight&Capability Pre-negotiated prices direct from manufacturers 50 Known & Trusted Suppliers Negotiate directly via Wippet platform Step-by step support to implementation at whatever pace you need ‘Lift, Shift & Compare’ your existing suppliers, products & prices Dedicated care procurement experts without recruiting additional headcount Data-led spend analysis powered by AI bringing the market to you Ready made tail spend management solutions to save time and improve control Easy to use & accessible via mobile, tablet and PC 24/7
marketplace fused with P2P functionality
B2B
Integration to financial system to simplify reporting
suite of tools to enhance your procurement capability
payment, multiple invoices
Powerful
One
receipting to ensure you only pay for what you need
compliance via ‘Walled Gardens’
workflows approvals to support your budget management Efficiency&Control Technology Our Solution for Tomorrow
Switch with Ease Club Free Membership Flexible Support Partner Free for spend over £500k p.a. P2P Plus… Fuse Circa. £250/month per care home

INTO PERSPECTIVE
What risks face local authorities planning to cut their adult social care budgets?
This issue, Into Perspective shares insights from the 11th annual State of Local Government Finance in England 2024 report. CMM hears from a law firm looking at the legal consequences of councils slashing their adult social care budgets and a leading care provider discussing how local authorities are stuck between a rock and a hard place with their finances.
In a new report titled The State of Local Government Finance in England 2024, the Local Government Information Unit (LGIU) has revealed that 51% of senior council figures warn their councils are likely to declare effective bankruptcy in the next parliament unless local government funding is reformed, with a further 9% saying they are likely to go bankrupt in the next financial year. Just 4% of council respondents had confidence in the sustainability of local government finance, while only 6% are happy with the Government’s performance on understanding the scale of the problem facing council finances.
Nine out of 10 respondents said their councils are raising council tax, and the same proportion are increasing fees and charges. At the same time, two thirds of councils
are cutting spending on services, meaning that services are getting more expensive for most residents at the same that they are being cut. For councils with responsibility for social care, the survey found that adults and children’s social care together make up the most serious long-term pressure, with 52% of council respondents saying adult social care was the greatest long-term pressure and 16.2% of councils planning on cutting adult social care.
According to the report, high inflation, alongside rising need for council services, has compounded the impact of central Government funding cuts. Even for councils that manage to balance the books, there are concerns that some services they provide may fall below legal standards, which will continue unabated without costly legal challenges.
Respondents to the survey called for a reform of social care, saying the reserves they are using to survive will soon deplete, while others called for more investment in preventative activities ‘which would reduce the pressure on our services – particularly regarding adult social care and children, in the medium to long term’.
The report declares it ‘unsurprising’ that the greatest long-term pressure is split between adult social care and children’s services, when ‘the proportion of upper tier budgets which go on these services are considered’. One respondent said, ‘Four percent of the population use social care, which is 70% of our budget – and you wonder why residents are not happy the place doesn’t look spotless and potholes need to be filled. Residents are not happy their council tax goes on so few. Social care needs reform.’
Jonathan Carr-West, Chief Executive of the LGIU, said, ‘We have long warned that a lack of funding combined with inflation and rising need for adult and children’s social care, homelessness, and SEND services has pushed councils to the brink.
‘This year’s State of Local Government Finance report reveals the desperate, ruinous financial situation councils find themselves in. Cutting services, borrowing more money and spending reserves year after year is completely unsustainable. Citizens are being failed.
‘With over half of councils warning us they are at risk of bankruptcy within the next parliament, it is no longer possible to blame individual governance issues. There clearly is a systemic issue and rather than bunging local government panicked injections of cash, whoever wins the next election will need to reform the entire system, bringing back multi-year settlements based on an area’s need and developing new ways of revenue raising.’
30 CMM April 2024

Local authorities have a duty of care
Jenny Wilde, Partner, Acuity Law : @AcuityLaw
Email: Jenny.Wilde@acuitylaw.com
Providers of adult social care services have been expected to do more with less for years now and so it is no surprise that councils are continuing to slash budgets. Providers remain sitting in the eye of a perfect storm with escalating staff costs, energy bills and mortgage rates adding pressure to their operations. Although the initial shock of the cost-of-living crisis has eased, providers are reflecting carefully on how they spend money and reinvest it back into their own businesses.
"Local authorities need to realise they have a duty of care to the people they place into care services..."
Councils need to understand that failure to pay appropriate fees means that providers may not be able to cover the costs of day-to-day essentials (for example, expensive electronic care systems, advanced training or activities). This will inevitably result in some providers trying to cut corners – not out of choice but necessity. Is that
really the best way to provide care to vulnerable people? Local authorities need to realise they have a duty of care to the people they place into care services and that placements they commission should be properly funded. To fail to do so increases risk.
Ironically, the reduction or stagnation of fees could ultimately result in an increase in local authority quality monitoring and safeguarding activity if providers are forced to work to reduced budgets. This would not only be a false economy and more costly from an expenditure perspective but – more importantly – will have an adverse impact on service users (not to mention the public’s view of local authorities more generally).
A further risk to local authorities is the increased scrutiny by the CQC. The regulator is now obliged to review how councils discharge their duty in line with the Care Act 2014 and, in my opinion, this should absolutely include how services are funded and how a local authority’s refusal to pay an appropriate fee impacts on vulnerable people.

A long-term trend of rationing adult social care
Geoffrey Cox, Managing Director, Southern Healthcare (Wessex) Ltd : @geoffreydcox
Email: geoffrey.cox@southernhealthcare.co.uk
The scale of collapse in the care sector is unparalleled. Unmet need, care withdrawal, underinvestment, disinvestment, commissioning backlog and unimaginable hardship witnessed begs many questions for local authorities. Councils are caught between Care Act responsibilities, ambitions, people needing support and dependency on central Government.
Councils have strict obligations under the Care Act 2014 and face increasing demand. Guidance was designed to promote wellbeing, assess and meet people’s needs, achieve the outcomes most important to them, help them retain or regain skills and confidence and prevent increased need or delay deterioration.
In 2023, there were 30,090 fewer people receiving long-term care, a fall of 4.6%, yet requests for support grew by 10.6%, reflecting a long-term trend of rationing adult social care. Simon Bottery, Senior Fellow, Social Care at The Kings Fund, suggested that social care has got worse since Government pledged to ‘fix’ it in 2019.
He outlined eight key problems, which are now worse:
• Due to a decade of freezing eligibility thresholds, adult social care has increasingly

stringent means tests, restricting access to services.
• The £86,000 cap on lifetime care costs has been postponed and may never be implemented.
• 1.6 million older people aren’t getting the support they need as local authority budgets struggle.
• There are increasing concerns about quality, illustrated by examples of 15-minute care visits in home care and fears of abuse and neglect in care homes.
• Although the CQC has regained powers to audit local authorities, it’s not clear what impact this has had, in light of financial difficulties and diminishing care provision.
• Staff shortages in adult social care, with more challenges ahead with recent Government immigration changes.
• The market is increasingly fragile. Many social care providers have handed back contracts or closed because the rates paid by local authorities for care are too low.
• Plans to get the health and care ‘system’ working better together have struggled to materialise. The reality remains that underfunded social care lacks influence over NHS-dominated structures.
CMM April 2024 31
Leeds Kirklees Derbyshire No inghamshire Warwickshire Worcestershire Cambridgeshire Norfolk Suffolk Hertfordshire Essex Buckinghamshire Northamptonshire Southend-on-Sea Bromley Kent Surrey East Sussex Brighton and Hove Bournemouth Christchurch Isle of Wight Poole Dorset Wiltshire Somerset Lincolnshire Blackpool Shropshire Berkshire North Yorkshire Gloucestershire Bedfordshire Luton Stoke-on-Trent Staffordshire Leicester Lancashire Blackburn Darwen Birmingham Cheshire East Oxfordshire Peterborough Bedford Leicestershire Rutland Hampshire Southampton Portsmouth The leading publisher of local authority care and support information Visit our website or call us on 01223 207770 to discuss how you can advertise your business to people looking for care and support in your area. www.carechoices.co.uk


Montane
To head up this new division the
has announced the appointment of Adam Lee.
The
E:
M:
E:

32 CMM April 2024 Montane insurance services is a specialist, independent broker supporting the healthcare and hospitality sectors. Contact Adam Lee: 07955410114 montaneinsurance.co.uk AMBITION | PROTECTION | INTEGRITY COMMERCIAL INSURANCE BROKERS Montane Insurance Services
Group launch a specialist
insurance division aimed at supporting the healthcare sector.
firm
creation
dedicated insurance
The specialist, independent broker supporting the healthcare sector Contact us:
01257 460270
of a
division aligns directly with the Montane Group and reflects the commitment to becoming the insurer of choice for the healthcare sector.
T:
anthony.rae@montanecare.co.uk
07546 932 811
darren.edwards@montanecare.co.uk
07855 361 960 montanecare.co.uk
M:
Albert House
Plas Bod Llwyd
Melrose
Lake view
Project Matterhorn
Offering a personal service with specific, individual needs of our clients always at the forefront of our approach. Rooted within 25 years, we specialise in building relationships rather than transactional advice. Covering all aspects of Healthcare including residential & nursing homes, adults with learning and physical disabilities, domiciliary care, mental health organisations and supported living. We understand the complex nature of the acquisition and disposal of a healthcare business. CARE
Lilycross
We all know that retaining talent in the social care sector is hard. For some care providers, things are getting better, but not at a quick enough rate. So, what can the sector do about it? Dave Beesley investigates with research-led commentary.
While there is pressure for Government to do more following a successive chain of broken promises, there is still plenty that providers can do to help themselves. No matter how big or small, all providers can deploy a range of solutions at various levels of complexity – tailored to your organisation’s resources. The first step in any retention process is to focus on understanding the data, both sector-wide and within your organisation.
Impact of market conditions
Last year, the sector reported a turnover rate of 28.3%, compared to a UK average employee rate of 15%. While social care turnover has reduced since last year,
>

CMM April 2024 33







34 CMM April 2024 WANT TO TRY? Call 0800 086 2462 Find out more www.c-t.co.uk STAY SAFE WITH SMART WIRELESS NURSE CALL Safer, more efficient care TIME FOR CHANGE! Care Home Insurance due for renewal? For FREE, no obligation quotations call 01273 977221 or visit: www.care-insurance.co.uk Phoenix Specialist Risk Solutions, Office One, 1 Coldbath Square, Farringdon, London, EC1R 5HL PHOENIX SPECIALIST RISK SOLUTIONS
this is likely supported by a spike in international recruitment activity which has produced better early retention results. Whilst this might be the case now, the sustainability of international recruitment is arguably questionable. There are also varying impacts that poor retention is having on different workforce demographics. Young people, for example, make up only 8% of all staff, and worryingly, the turnover rate for under-20s in 2021/2022 was reported to be 53%. Supporting and inspiring our workforce of the future has never been so crucial.
“Despite the increase in international staff, vacancies have only decreased by 13,000, so the staffing gap continues to be nearly unmanageable to close.”
Hft’s Sector Pulse Check 2023 highlighted the decrease in domestic applications, especially among small organisations. Despite the increase in international staff, vacancies have only decreased by 13,000, so the staffing gap continues to be nearly unmanageable to close. A focus on domestic recruitment must continue and for it to be successful, the right building blocks need to be in place to create the foundations for retention success.
Why are your people leaving?
Our findings from exit interviews of over 2,200 leavers revealed that almost half were moving out of their career in social care into other sectors. During the pandemic, the sector ‘borrowed’ workers from other industries. These have since reopened and often pay more and can start people in their roles soon after an application is successful. Seemingly, people are returning to where they were, such as hospitality and retail – which, alongside healthcare, are the top sectors candidates apply to alongside making applications to social care. This is a missed opportunity. Understanding why people are leaving your organisation is the next step in
building strong retention practice and finding solutions to fix the issues.
Our data also found that family, domestic or personal reasons were those most consistently cited for exit over the past three years. Likewise, relationships with managers or management style was rated amongst the top three reasons for leaving across all three years of data. A career change or working hours were interchangeably rated third and fourth.
Personal reasons could arguably be outside of an organisation's influence, which is often the case. However, even when this is cited as a reason for leaving, there are common factors that could have influenced employees to stay – if managerial relationships were better or more flexible working arrangements were adopted. There is also a link with working hours and shifts – often a change in family needs means working hours and shift patterns are no longer suitable. How are you considering whether this is a reality for your leavers, finding ways to foster better relations and offer flexibility?
Key to facilitating conversations about an employee’s happiness at work and intentions to stay are through regular catch ups and one-to-one meetings. Our data found over a third of people hadn’t had a meeting with their manager by week eight of employment. When asked whether they felt valued, a third did not. Finding the time to meet with staff and demonstrate their worth to the organisation may well prevent early exit of new starters, especially those new to working in care.
It is also worth considering pay as a reason for leaving. We have seen this reason increase by 1% each year, and while people are not leaving on mass because of pay, it does feature as a reason for people being hesitant to apply to social care. According to Skills for Care, in 2022, care workers needed to be paid around 60p more than the National Living Wage to see an improvement in turnover rates.
Retention solutions
Now that we have reviewed the problems facing the sector, and you have considered how they may be impacting on your organisation, you have a stronger foundation to look at the retention building blocks. Using these blocks, whether they’re large and intricate, or small and sturdy, will ultimately assist
>
CMM April 2024 35
>
FOUNDATIONS FOR RETENTION SUCCESS: BUILDING BLOCKS FOR BETTER EMPLOYEE ENGAGEMENT
in delivering better retention outcomes.
Looking at retention often means looking at the recruitment process. How are you setting out your stall in job adverts? What are people saying and hearing about you? What do candidates understand about you as an organisation? Getting this right doesn’t have to be an expensive exercise. Give an open and honest view of your care setting in the recruitment process. Offer previews, open days and a tour during your interviews, if appropriate to do so. Engage with your local community and take part in events such as Care Home Open Week. Tell stories about the people you care for and support, to give a clear view of what it truly means to be a part of the social care industry.
Another key building block is to review your employee benefits offering. Your workforce will want different things – so ask your current teams and candidate pool exactly what they want. Whether that’s reasonable flexibility in working hours, support with travel arrangements or on-demand pay to name a few, have an open dialogue with your teams.
“Better recruitment and retention within your organisation are not achievable from making improvements once and never doing them again.”
Not only can this help with attracting candidates, but it also assists with making sure that people stay once they are hired, including your under-represented workforce demographic.
The next block of your building needs to focus on your onboarding experience. Even after people have made it through your recruitment process, how they are treated at the beginning and during their employment will have an impact on how long they stay – not just with your organisation, but ultimately within the sector. Provide a meaningful and well-thought-out induction, ensure regular communication as part of one-to-one meetings, discuss opportunities for training and development, recognise and praise good work,
assign buddies and mentors and conduct both retention and stay interviews.
Futureproofing your workforce
If you think your building is complete, you need to keep surveying it for cracks and faults. Like any building, it needs repairs and maintenance as time goes on. Better recruitment and retention within your organisation are not achievable from making improvements once and never doing them again. You need to keep looking at your data and be aware of what others are doing – what are the push and pull factors? Communication within your teams should be prioritised to ensure that people feel valued and heard.
Positively, our research cites that the part of their role that employees enjoy the most is contact with the individuals they care for and support. This was by an overwhelming majority, with over 55% putting it at number one. Similarly, type of work was consistently a top reason for attracting employees to the role. As a sector, we can and do attract people with the right values – especially when we are adopting values-based recruitment.
Better retention doesn’t come overnight. It takes a lot of listening, data analysis and an openness to doing something different. That said, considering your building blocks for change will, in time, go far in having a positive impact. After all, we all have an opportunity to shape the future success of the social care workforce – so doing something now can only help to pave the way to a brighter workforce. CMM

Dave Beesley is Social Care Talent Director at Cohesion. Email: dave.beesley@cohesionrecruitment.com Web: https://cohesionrecruitment.com
36 CMM April 2024
How is your organisation adopting values-based recruitment? What steps are you taking to retain staff? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts.
> FOUNDATIONS FOR RETENTION SUCCESS: BUILDING BLOCKS FOR BETTER EMPLOYEE ENGAGEMENT
FUNDING THE FUTURE OF CARE

Our secured business loans range from £250,000 to tens of millions and are built with the care industry in mind, so owners, operators, residents, and whole communities can benefit from best-in-class care homes and retirement villages.
Tailored finance to help you grow
A loan that follows your project’s life cycle: One bespoke loan to support all of your funding needs.
Capital expenditure to invest in the future: Funds to improve new and existing care facilities.
Flexible loan security packages: We look beyond collateral to your future growth potential.
Custom umbrella facilities:
Save time and money with our long-term umbrella options.
Why partner with us?
Get funded faster: Unlike high street banks, we can have the funds in your account in weeks.
Meet key decision-makers: We invite you to a Credit Committee meeting and keep you updated.
Tailor your finance to your future: Our flexible loan facilities span the full length of your project.
Achieve success with our experts: Our finance team are award-winning experts in senior living.
Given the significant undersupply of beds predicted in the future, we appreciated the speed and responsiveness of the OakNorth team, who also demonstrated a clear understanding of our business and the UK’s care market.
Keith Crockett CEO of Lovett Care
Get in touch with our team of experts today
Email us at questions@oaknorth.co.uk Visit us at oaknorth.co.uk




38 CMM April 2024 Caregraphy Caregraphy is an advanced health and social care management system for creating and managing records like notes, care plans, scheduling, eMARs, and a lot more. It is also geared to improve your competence for Ofsted and CQC compliance. Being easy to use, Caregraphy enhances efficiency allowing you to focus on improving outcomes for your clients. Trusted by providers of supported accommodation, children’s homes, family assessment and other residential settings, Caregraphy is an easy choice. We are not just a software provider, but we are committed to partnering with you to ensure Caregraphy meets your needs. Book a demo today and see how to succeed with Caregraphy! @caregraphy +44 3333 583 123 www.caregraphy.com sales@caregraphy.com An easy way to manage your care organisation BOOK A DEMO
Picking up the pace
Protecting the human rights of people with a learning disability and autistic people

If a true measure of society is how it treats people in some of the most vulnerable circumstances, then what can be said of Government’s commitment to reduce its reliance on long-stay assessment and treatment provision for autistic people and people with a learning disability? Dr Rhidian Hughes examines the issue in depth.
Behind schedule
In the NHS Long Term Plan, the Government made a commitment to reduce the numbers of autistic people and people with a learning disability living in in-patient settings. The commitment made was to reduce the numbers by half by March 2024. However, there are still over 2,000 children and adults in these facilities, meaning the reduction is only around one third.
In 2015, there were 2,905 autistic people and people with a learning disability in these units. Despite some progress, the speed and scale of transformation has fallen far short of the aspiration and, nearly 10 years on, latest NHS England figures show the number of autistic people in inpatient facilities has actually increased.
CMM April 2024 39
>
Data from NHS England points to an increase of 7.3% in the numbers of autistic inpatients (both with and without a learning disability) in mental health hospitals between March 2017 and August 2023, and an increase of 51.3% in the number of autistic people without a learning disability in the same timeframe. The reasons for this are many and complex but include a Mental Capacity Act in need of reform, a lack of early support that can help prevent the escalation of need, a more nuanced approach to risk management and minimisation of restrictive practices. Successive targets to reduce the number of people being referred to these settings and increase referrals into the community have been missed.
Missed opportunities
Almost a decade ago, NHS England, the Local Government Association (LGA) and the Association of Directors of Adult Social Services (ADASS) published Building the Right Support: guidance supporting commissioners to reduce the number of people with a learning disability and autistic people in a mental health inpatient setting and seeking to develop community alternatives to inpatient care. Since its publication, there has been no shortage of service models, specifications and supplementary guidance published. All of this should have meant fewer people needing to go into hospital for care.
These are settings that are highly restrictive, secluded and use physical restraints and over-medication, which are seriously flawed and fundamentally wrong care models.
Scandals including Winterbourne View, Cawston Park and Whorlton Hall have all brought people’s experiences into sharp focus. Recently, the judge overseeing the case of four carers convicted of abusing people at Whorlton Hall said the setting had a ‘malign culture’ and was an ‘unpredictable and inherently frightening place to live’.
Priorities for change
National commissioning guidelines for integrated care boards (ICBs) state that an in-patient stay ‘should be for the minimum time possible, for assessment and/or treatment which can only be provided in hospital’. To meet this guidance requires
established procurement routes to be disrupted and a vibrant care and support market commissioned.
Yet the market for support providers has been largely over-looked nationally. We have seen little evidence that ICBs have plans to help people move out of hospital or crucially avoid being admitted in the first place. We see little upstream investment, while few providers have been encouraged or supported to develop the kinds of community-based services that would provide the alternative to inpatient provision so desperately needed. In some areas we see demand, made up of people ready for discharge, outstripping the supply of high-quality housing and support packages.
There is an urgent need to build social care provider capability, capacity and – crucially – shared interests and values in supporting people, in what is an area of highly complex work. Done well, good commissioning invests to save over the longer term. It resources prevention, partners with community providers and housing suppliers and draws on the experiences of people with lived experience and their families who articulate readily what they need, namely funding in the right place, well-managed transitions between services and skilled staff. But this practice is far from universal, and the system is not on the right course to evidence significant improvement.
Previous governments acted on the scandals of long-stay hospitals with legislation and funding. As a general election looms, the new Government must intentionally draw on the levers it has available to make far better progress than we have witnessed in recent years.
Creating a unified voice
Working with the Challenging Behaviour Foundation and others, we wrote to all political leaders urging them to protect the human rights of autistic people and people with a learning disability. We need the next administration to create and maintain political will to make these ambitions a reality.
VoiceAbility is calling on the Secretary of State for Health and Social Care to intervene and use the new power in the Health and Social Care Act 2022 to direct NHS England to urgently reduce the number of people
with a learning disability and autistic people in assessment and treatment units. Doing so would strengthen public accountability across the system.
In addition, we are continuing to call on the Secretary of State to direct the Care Quality Commission (CQC) to rate all assessment and treatment units as ‘Requires improvement’ if anyone has been living there for more than 12 months. In addition, for that rating to be downgraded to ‘Inadequate’ if anyone has been living there for more than 24 months and for all new admissions to be halted until the rating has improved. The Secretary of State should also require the National Audit Office to present an annual report to parliament on progress.
Time to act
There are citizens who are detained in NHS-funded accommodation, some for many years, and in some instances for over a decade – this is the responsibility of central Government. It would be hard to imagine any other circumstances in which a British citizen could be detained indefinitely by the state, without a trial. Especially, where Government has explicitly acknowledged that the conditions of their detention are, for the majority, inappropriate and should be ended. Yet, they continue to detain them in precisely the same, and in some instances worse, circumstances over many years.
There is no shortage of reports containing practical solutions and no further general reviews are required. There is no debate or disagreement that the placement of people in assessment and treatment units for extended periods of time is damaging to their wellbeing. Neither is there a shortage of knowledge and expertise, including from people with lived experience and their families seeking better outcomes. We know what’s needed, but we need a plan and commitment from Government to act with urgency to address this human rights scandal.
We stand with partners committed to the closure of all inappropriate settings for autistic people and people with a learning disability. We need to push for this to be a national priority and, as the general election looms, we need an administration that is willing to relegate these institutions to the past. CMM
40 CMM April 2024
What are your sector-specific priorities for the next Government? Visit www.caremanagementmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts. Dr Rhidian Hughes is Chief Executive at the Voluntary Organisations Disability Group (VODG). Email: ceo.office@vodg.org.uk X: @RhidianHughes @VODGmembership > FOUNDATIONS FOR RETENTION SUCCESS: BUILDING BLOCKS FOR BETTER EMPLOYEE ENGAGEMENT

WALKIES FOR CARE JAN to MAR
CONNECTED TO CARE
Connected to care; awareness campaign across social media encouraging people to donate and express how they are related to care
Dog walking fundraising month with a collective walk in Richmond Park on Friday 26th April
GOING THE EXTRA MILE
Get together with your colleagues, friends and families and Go the Extra Mile for care workers.
SKYDIVE
This is your chance to be a superhero for a cause. Rally your friends, family, and colleagues, and let's create a sky-high wave of support for care workers.
LEVEL UP FOR CARE
5 - 30 AUG
Level up your support for a cause you're passionate about by participating in our gaming fundraiser, where every virtual victory directly contributes to making a real-world impact
PROFESSIONAL CARE WORKERS’ WEEK 2024
ANNUAL TREK (EXACT LOCATION TBC) (CHARITY CHALLENGE)
TBC -OCT
THE CWC FIREWALK
Spend an evening with Mindshift Experiences learning how to overcome your fears then walk across fire to raise funds for The CWC. 4
WRITING COMPETITION 2024
6
1 - 30 APR
- 31 MAY 20 JUN EVENTS CALENDAR
16 - 19 SEP 20 SEP
NOV - 6 DEC 2 DEC - 10 JAN WINTER PRIZE DRAW 2024 TO DISCUSS RUNS, WALKS and BESPOKE FUNDRAISING PLEASE EMAIL: FUNDRAISING@THECWC.ORG.UK www.thecareworkerscharity.org.uk
RESOURCE FINDER: RECRUITMENT

Good people are the backbone of any good service, and the care sector is no exception. Here, we’ve profiled some of the leading recruitment providers that specialise in social care and shared their areas of expertise.
42 CMM April 2024
BlueGreen
Recruit
Tel: 01656 336094


Email: info@bluegreenrecruit.co.uk
Website: https://bluegreenrecruit.co.uk
SECTORS
• All types of health and social care.
• Residential care.
• Home care.
• Extra care.
• Supported Living.
• Reablement/intermediate care.
SERVICES
• Permanent and fixed-term recruitment and support.
• Recruitment and support covering all levels of roles.
LEAD INDIVIDUAL
As a recruiter, headhunter and talent scout, Managing Director, Natasha Best, is wholeheartedly devoted to linking individuals with opportunities that resonate with their abilities and aspirations. Her fervour lies in guiding others to unlock their potential and reach their career objectives. Natasha's experience working with vulnerable groups has sharpened her knack for identifying talent and empowering individuals to recognise and embrace their own worth.
Guided by personal principles of courage, collaboration and optimism, she is steadfast in fostering partnerships with people to amplify their achievements and showcasing the myriad possibilities life holds. Natasha is profoundly driven to effect positive change and eagerly seeks opportunities to contribute in any capacity possible.
Natasha has a degree in Psychology, Leadership and

Natasha Best
Tel: 01656 336094
Management and a Business and Innovation Masters. She also has accredited qualifications in Charity Management, so enjoys working with organisations with a social purpose.
COMPANY INFORMATION
BlueGreen Recruit prides itself on acting as your internal talent acquisition partner, working hard to understand your business and your requirements for the role you’re hiring for. The team focus is on introducing you to a select number of candidates who fit the specification and the organisation.
BlueGreen Recruit’s consultants work to build effective and lasting relationships with partner organisations. This approach ensures the team can act as an integral part of your corporate function. Roles the company typically recruit for range from ancillary staff and support workers to senior management and leadership roles, and support roles that include HR, finance, projects and quality.
At BlueGreen Recruit, the ethos is rooted in being a valuesled organisation. The pillars of confidence, active listening, respect and accountability serve as the compass guiding the team. These values not only shape BlueGreen Recruit’s approach to talent acquisition but also permeate every aspect of the team’s interactions with clients, candidates and partners.
For BlueGreen Recruit’s candidates, the team offers ongoing support and advice, whether or not they are working together to seek a placement.
Email: natasha@bluegreenrecruit.co.uk
Health Automated
Tel: 01255 446655
Email: general@healthautomated.online
Website: https://healthautomated.online
SECTORS
• All care operations.
• Home care.
• Care homes.
• Supported Living.
SERVICES
• Recruitment software.
• Applicant Tracking System (ATS).
LEAD INDIVIDUAL
Lee Trueman, Co-Founder of Health Automated, brings a wealth of experience in digital transformation in the care sector. With over a decade of expertise, Lee has been instrumental in revolutionising the way healthcare organisations leverage technology to enhance their operations. His deep understanding of the healthcare industry and passion for innovation has driven the development of cutting-edge solutions like Social JobFindr. Lee's visionary leadership and commitment to improving patient care through digital solutions have positioned Health Automated as a leading force in the industry. His expertise in digital transformation continues to shape the future of healthcare recruitment and beyond.
COMPANY INFORMATION
Social JobFindr is revolutionising the recruitment process with its AI-driven job matching and applicant tracking system (ATS) capabilities, combining the efficiency of a recruitment app

Lee Trueman
Tel: 07702 553433

with the intuitiveness of Tinder.
With Social JobFindr's advanced AI features, finding the perfect candidate has never been easier. Leveraging powerful algorithms and machine learning, Social JobFindr intelligently scans CVs and job descriptions to match candidates with the right skills, experience and qualifications. This saves valuable time and resources for healthcare organisations by swiftly identifying the most suitable candidates for open positions.
Social JobFindr's ATS seamlessly integrates with Architecture, Health Automated’s AI care management platform, empowering hiring managers to effortlessly manage the entire recruitment and onboarding process from a single platform. Tracking candidates, scheduling interviews, collaborating with recruitment teams and managing documentation has never been more streamlined. This ensures a seamless transition for candidates as they become part of the healthcare organisation.
By utilising Social JobFindr, healthcare providers not only improve the quality of hires but also reduce recruitment errors, minimise turnover rates and, ultimately, deliver exceptional care to patients. The integration of Social JobFindr with Architecture heralds a new era in healthcare recruitment, enabling organisations to access top talent more effectively.
Embrace the future of hiring in healthcare with Social JobFindr and Architecture, the AI care management platform.
Email: lee.trueman@healthautomated.online
RESOURCE FINDER: RECRUITMENT
43 CMM April 2024
ISSUE 2 is out now!
The informative publication is focused on cost-saving solutions and is essential reading for operational leaders and purchase decision-makers in the social care sector.

In collaboration with @cmm_magazine @CareEngland www.caremanagementmatters.co.uk www.careengland.org.uk
Click here for more information, and to read/download the latest issue
Meridale Recruiting Solutions Ltd

Tel: 01902 240019
Email: info@meridalerecruitingsolutions.co.uk
Website: www.meridalerecruitingsolutions.co.uk
SECTORS
• Care homes.
• Nursing homes.
• NHS/private hospitals.
• Councils.
SERVICES
• Overnight care services.
• Live-in care.
• Sitting services.
• Learning disabilities.
• Complex behaviour.
• Physical disabilities.
• Escorting to shopping, holidays and leisure centres.
COMPANY INFORMATION
Meridale Recruiting Solutions Ltd is a prominent healthcare staff recruitment agency based in Wolverhampton. The team, consisting of experienced and highly qualified professionals, understands the importance of finding truly exceptional caregivers. Every member of staff is carefully selected for their compassionate and understanding nature, ensuring

Leonard Kaurrai
Tel: 01902 240019

they are approachable, friendly and capable of working closely with each service user to tailor a care package that best suits their needs. Their commitment to excellence is evident, as their carers are the driving force behind everything they do.
If you require healthcare staff, whether it's for an emergency shift or a longer-term placement, Meridale Recruiting Solutions Ltd is at your service around the clock. In its extensive database, it has a diverse range of skilled professionals covering various specialities, including support workers, senior carers, clinical healthcare assistants and nurses.
Meridale Recruiting Solutions Ltd caters to the staffing needs of residential nursing homes, domiciliary care, dementia care, mental health, complex care and the private sectors. Choose Meridale Recruiting Solutions Ltd for reliable and exceptional healthcare staffing solutions tailored to your specific requirements.
Email: leonard.kaurrai@meridalerecruitingsolutions.co.uk
Social Care People Ltd
Tel: 01234 973020
Email: info@socialcarepeople.co.uk
Website: https://socialcarepeople.co.uk
SECTORS
• Care homes.
• Care homes with nursing.
• Domiciliary care.
• Housing associations.
• Supported Living.
• Mental health.
• Private hospitals.
• NHS.
• Children’s services.
• Disability services.
• Health and wellbeing.
• Public sector services.
SERVICES
• Specialist job board for the care sector.
• Online recruitment advertising campaigns across a variety of job boards.
• Free recruitment training.
LEAD INDIVIDUAL
Claire Dalton, Director, has a career in recruitment spanning two decades, specialising in the social care and not-forprofit sectors. She began her journey in recruitment with local press advertising, transitioning to the realm of online job board recruitment advertising during the early stages of job boards. Claire also served as a Recruitment Manager at a large UK-wide social care organisation, gaining a unique dual perspective on the sector’s challenges.
Specialising in collaborating with clients within healthcare and charity organisations, Claire established NFP People in 2018. After recognising the need for sector-specific differentiation, she introduced the companion brand, Social Care People, last year.

Claire Dalton
Tel: 01234 973020

Driven by a genuine passion for addressing recruitment challenges in the care sector, Claire writes and delivers free training events, aiming to share the insights amassed over the years and empower fellow recruiters to enhance their strategies.
COMPANY INFORMATION
Social Care People works exclusively with clients in the care sector, leveraging its extensive experience with numerous clients across the UK. The company offers a range of services to enhance and streamline recruitment functions for its customers. In September 2023, Social Care People introduced its specialist job board for the social care sector, providing organisations with a cost-effective and user-friendly platform to advertise vacancies, targeting candidates seeking roles specifically in the sector.
In addition, the company partners with care organisations, delivering affordable and comprehensive job board packages across major UK job boards at a fraction of the direct cost. Social Care People assists in candidate management and proactive searching without the high fees associated with traditional placement agencies.
Committed to giving back to the sector, the company provides free online training covering various recruitment aspects, including employer branding, Equality, Diversity and Inclusion (EDI) training and effective advertising writing through group sessions and personalised one-on-one training.
Email: claire@socialcarepeople.co.uk
RESOURCE FINDER: RECRUITMENT 45 CMM April 2024
CELEBRATING EXCELLENCE
Sector Care Awards


Friday 15th March 2024 saw the return of the annual Markel 3rd Sector Care Awards which marked its 10th anniversary this year. The Awards returned to The Grand Hotel in Birmingham which provided a stunning setting to host our judges, finalists, winners and sponsors.
MARKEL 3RD SECTOR CARE AWARDS 2024 Markel
Sally Lindsay hosted the awards for the very first time and effortlessly intertwined humour and heartfelt emotion. She engaged with both the audience and winners, creating an unforgettable connection. Everyone in attendance was also treated to two moving performances from Our Dementia Choir. The choir beautifully opened the awards ceremony and had a profound impact on the audience with their united voices. The group put on a mashup finale which had everyone up on their feet and smiling, rounding off a perfect day.
Compassion Award
Winner: Phil the Gardener, Nightingale Hammerson.
Finalists: Keith Jenkins and compassionate partners, St Andrew’s Healthcare and HOPE Team, The Cellar Trust.
The judges said… ‘Passionate about their role and generous in sharing their knowledge, our winner has gone above and beyond simply by doing what they are great at doing –connecting with people. This person is delivering compassionate, person-centred care – but not by the book, not by reading or policy; simply because it comes naturally. Our winner doesn’t realise the impact they have and the difference they are making to those around them.’
Community Engagement Award
Winner: East Support Services Vulnerable Adults Services.
Finalists: St Margaret’s Hospice Care and New Beginnings NE Ltd and Ngage NE Ltd.
The judges said… ‘This grassroots community group use their natural gifts and community connections to establish a network of vital community meeting points embedded in the places the people they support live. Not only offering their support with mental health but joining and engaging with other community groups and services.’
Leadership Award
Winner: Donna Henderson, Birmingham Mind.
Finalists: Edwine Tembong, Outlook Care and Davina Collins, Cumbria Health.
The judges said… ‘Passionate, tenacious and strong, the winner of this award has absolutely demonstrated outstanding leadership, making a difference not only to the service and those using it, but also to their staff. Our judges were impressed by their drive and commitment and particularly, how they are viewed by their team, who said, "When people pull apart, she’s the type of person to pull us together.”’

46 CMM April 2024
3rd
Technology Award
Winner: Health at Home, Cumbria Health.
Finalists: Bolton Cares Group and Data and Analytics Department, St Andrew’s Healthcare.
The judges said… ‘Despite a very strong field, this service stood out in relation to its proactivity – making excellent use of technology to identify and address health issues early. This has resulted in an overall improvement in efficiency of the service and the patient experience.’
Creative Arts Award
Winner: We Care Campaign/Domestic Dusters Collaboration.
Finalists: DARTS – Creative Directions Project and Ngage North East Ltd.
The judges said… ‘The winner of this award shines a light on how art can be used for campaigning in a unique way to highlight the invisible support systems relied on to keep a diverse and inclusive society going. The judges are really excited to see their continual journey growing.’
CMM spoke to Katy Styles and Vanessa Marr, who commented, 'Sometimes you can lose a sense of what you mean to other people. I think this has been a real reminder of that. I think it’s really special to bring the voices of unpaid carers into perspective, to bring them here.'
Collaboration (Integration) Award
Winner: Safe Spaces.
Finalists: Intergenerational Music Making (IMM) and Dementia Support.
The judges said… ‘The judges of this award felt the winner had truly embodied collaborative and partnership working to provide innovative ‘all age’ support. In doing so, drawing on wide ranging expertise and knowledge "for the good of the people" within a very diverse and deprived population.'
Dementia Care Award
Winner: Alzheimer’s Support Day Care Team.
Finalists: Nightingale Hammerson and Sage House, Tangmere.
The judges said… ‘The winner has expertly developed unique spaces to support those living with dementia and their families. The team work incredibly hard to make sure their members are not defined by dementia, and instead focus on each person’s individuality and character. The judges were overwhelmed by the exceptional care and support given and felt families who walked through the door of these wonderful places would feel an instant sense of relief and become part of an amazing and supportive family.’
Development and Innovation Award
Winner: The Nursery in Belong.
Finalists: Elorn Boglo & Ryan Jones, Brainkind and The Co-production of the Care Planning Process with people living with Dementia, St Andrew’s Healthcare.
The judges said… ‘The winner of this award demonstrates how people with little more than big ideas can achieve innovation that changes lives. This innovation is all about connections and community, and our winner has built a model that encourages people to learn together and benefit from each other.
‘They have created something that breaks down barriers, removes stigma, and makes invisible people seen. Our judges were excited about the potential – and where this could go next.’
Social Care Nursing Award
Winner: Jemma Sharratt.
Finalists: Nicole Hepplewhite and Tracey Dunkley.
The judges said… ‘The judges agreed that this registered nurse embodies "good professional practice". Her attention to the small details, capacity for care and critically thinking truly enables all she works with, to "live to their full potential". With a commitment to lifelong learning, she was able to convey how her empathy and compassion have grown and how this is used when providing person-centred holistic care.’
CMM spoke to Jemma, who commented, ‘I’m so excited about the future of social care and this just shows that we’re right at the beginning of that journey. It’s amazing to see that nursing in social care is being taken seriously.’
End of Life Care Award
Winner: St Ann’s Hospice.
Finalists: Nightingale Hammerson and Galanos House, Royal British Legion.
The judges said… ‘The winner demonstrated an amazing willingness to develop innovative approaches in providing palliative and end-of-life care, focusing on a rehabilitative approach.
'The team hold a strong belief that everyone deserves to have the best quality of life possible when living with a life-limiting illness. The judges applauded the incredible work being carried out to ensure people’s final wishes are possible and to support families before, during and after their loved one’s end of life.’
Finalists: Social Care Frontline Pay Campaign and St Andrew’s Healthcare and those who supported the Language Matters Campaign.
The judges said… ‘This campaign brings together what many in this room know to be true. Our sector is undervalued and underfunded. They have worked alongside people with lived experience to highlight the impact great care and support has on their lives. They have raised a profile of social care nationally, working in collaboration with other providers, people who are supported and political parties.’
Making a Difference Award
Winner: Shaleeza Hasham, Adopt a Grandparent.
Finalists: Ed Russell, WCS Care and Mark Heasman, Provide.
The judges said… ‘We wanted to highlight that we had an extremely difficult decision to make for this award as each finalist was outstanding.
'But, there can only be one winner and the judges decided that this person and their initiative really are leading the way and making a difference across services on a vast scale with their passion for alleviating isolation and loneliness amongst the elderly population. This year’s winner has developed an amazing network of volunteers from all around the world to join people together to share wisdom, experience and perspectives.’
CMM spoke to Shaleeza, who commented, ‘This award means a huge amount for a really small, growing charity with big ambitions because the more we can have exposure, people can hear about the important work that we do, the more we’ll be able to pair lonely elders with willing volunteers around the world.'
A massive thank you!
Our thanks go to everyone who was involved in the Markel 3rd Sector Care Awards 2024, from those nominated to the judges, supporters and sponsors. In particular, our headline sponsor, Markel, without whom the awards would simply not be possible.
We look forward to recognising more inspiring work in the voluntary and not-for-profit care and support sector with our 2025 event, which will take place on Friday 14th March. Follow us on social media to stay up to date. @3rdSectorCare and #3rdSectorCareAwards CMM

Winner: Community Integrated Care – Unfair to Care Campaign.
Headline sponsor
 The Dame Esther Rantzen Campaigning for Change Award
The Dame Esther Rantzen Campaigning for Change Award
CMM April 2024 47
NATIONAL CARE ASSOCIATION (NCA) CONFERENCE 2024
9th May 2024

Join the NCA, chaired by Nadra Ahmed CBE, Executive Co-Chair, and Ian Turner, Co-Chair, for an informative day with guest speakers and interactive panels at its National Conference on 9th May 2024.
Hear from industry leaders at the conference, taking place at Manchester United Football Club, where the agenda will focus on the action that the NCA and the wider sector is taking to improve the quality of care.
Commenting on the motivations behind the conference agenda, Nadra Ahmed CBE, Executive Co-Chair at the NCA, said, ‘For too long, we have allowed governments of all colours to neglect social care. This conference is designed to support care providers to have their voices heard above the rhetoric. We face many challenges, but the two that appear above all others consistently are funding and workforce; both need to be addressed to create a long-term social care solution.
‘As we sit at the edge of another election, we are likely to be told that there is a solution that each party has, so we are bringing politicians and sector experts to our event to tell us their thoughts. Clearly there is a litany of broken promises, but that must not deter us as we know that the need for social care is increasing and in such a way that we cannot afford to allow the collapse of provision across the country. We know that the most “at risk” provisions are small and medium-sized providers, which is why this event is tailored specifically for that group but will apply to large groups too.
‘Our strength is our membership as we continue to support and fight for you. We are united in our purpose to ensure that those who need care and support at critical times of their lives have a service to turn to.’
Turning the tide...fighting back!
The conference speakers will include specialists on the pressing topics that are impacting on the adult social care sector. One such example is Andrew Gwynne MP, Shadow Minister of Social Care, who will be attending as a guest speaker.
Other guest speakers* attending include:
• Sir David Pearson, who will be reflecting on the future of social care. David is currently the Co-Chair of a national steering group to develop an adult
social care workforce strategy. This is being led by Skills for Care.
• Sanjay Dhrona, who will be discussing how to get Outstanding in a CQC inspection. Sanjay is Managing Director at The Close Care Home in Oxfordshire and a Non-Executive Director at The Outstanding Society.
• David Brindle, who is a leading social policy journalist and former Public Services Editor and Society Editor of The Guardian
• Martin Plimmer, who is a Senior Investigating Officer at the Gangmasters and Labour Abuse Authority.
In addition, other sector representatives attending the conference will include bankers, insurance specialists and lawyers, who will be present to speak and provide advice to delegates.
Members and non-members are welcome to attend this important event in the social care calendar. This national conference is a must-attend, informative event for the sector. Registration for the conference opens at 8.45am on Thursday 9th May 2024.
To book your conference ticket and for more information about the event, including costs, visit the NCA website. Alternatively, email info@nationalcareassociation.org.uk to secure your place.
The NCA is currently promoting a special offer for non-members. If you attend the conference, you will receive a three-month subscription to NCA Newsletters.
In addition, if you join the NCA as a member within the three-month period, you will receive a discounted membership, subject to terms and conditions.
*The conference speakers and agenda are subject to change. CMM
EVENT PREVIEW
48 CMM April 2024



WHAT’S ON?
Event:
Date/Location:
Contact:
Event:
Date/Location:
Contact:
Event:
Date/Location:
Contact:
Event:
Date/Location:
Contact:
Event:
Date/Location:
Contact:
Event:
Date/Location:
Contact:
Event:
Date/Location:
Contact:
Care Show London 24-25th April 2024, London
www.careshowlondon.co.uk
National Care Association 2024 Conference 9th May 2024, Manchester https://nationalcareassociation.org.uk/ news-events
Being Prepared for CQC Inspection 9th May 2024, Online
www.skillsforcare.org.uk/news-and-events/ Events-and-networks.aspx
Integrated Care Summit 2024 14th May 2024, London
www.kingsfund.org.uk/events/integratedcaresummit
An Introduction to Age-friendly Communities 15th May 2024, Online
https://ageing-better.org.uk/events/anintroduction-to-age-friendly-communities
The Mental Health & Wellbeing Show 17th May 2024, Cardiff https://mhwshow.co.uk
ACP 2024: Advancing Continence Priorities 20th-21st May 2024, Hilton Liverpool City Centre, Liverpool https://acpcontinence.co.uk/conference
CMM EVENTS
Event:
Date/Location:
Contact:
CMM Insight webinar – growing a greener future 30th April 2024, Online 12.00pm
Lisa Werthmann, Director, 01223 207770 lisa.werthmann@carechoices.co.uk www.caremanagementmatters.co.uk/webinar


CMM April 2024 49
Please mention CMM when booking your place. Sign up online to receive discounts to CMM events and for more information on our upcoming events in 2024. www.caremanagementmatters.co.uk : @CMM_Magazine #CMMInsight
to 1.00pm
Phone: 023 8048 3000 www.alphalabs.co.uk Purchase at NHS supply chain: my.supplychain.nhs.uk/catalogue or www.alphalabs.co.uk/safer-denature Safe, Compliant Controlled Drug Disposal Guard against the misuse of controlled drugs to protect your staff, residents and communities by using drug denaturing kits. ; Suitable for use with tablets, capsules, liquids, aerosols or patches ; Formula contained in a water-soluble sachet to prevent accidental spillage of granules ; Available in volumes 250ml to 20L 07 July 2023 - Care Management Matters - Safer Denature.indd 1 12/07/2023 15:31:11
STRAIGHT TALK
Is Advance Care Planning fit for purpose? Professor
Heather Richardson investigates this question, and shares details of a recent conference created to delve further into the topic.
One fundamental advancement in end of life care has been troubling me for some time – Advance Care Planning (ACP). I have been concerned about the way it’s conceived and practised, with the pandemic only increasing this. What should’ve been a series of thoughtful and compassionate conversations about the focus, place and nature of care as someone’s condition advances, has for many become a transactional tool for people to make stark choices.
As society is shifting and people want greater self-determination and control over their life and death, this needs to be different. We need to act now to give both professionals and members of the public the tools to ensure ACP regains its status as an effective means of establishing what matters to people, then plan and deliver care on that basis, albeit with a healthy dose of realism included.
Working with colleagues involved in Community Action, we organised ‘Future Planning: Advance Care Planning Reconsidered’, a one-day conference, to start a serious conversation about what ACP really is, why too often it’s not working and how we can make it work better.
Sector representatives offered their take on ACP’s value, academics provided evidence of effectiveness and people with lived experience shared the impact of ineffective ACP. Many people reflecting on their own experience offered new ideas about how health and social care professionals talk to citizens about their plans, and how they negotiate the highly sensitive issues around serious illness, death and legacy.
ACP was designed to be a two-way conversation in which professionals would listen to the person’s wishes and preferences, then negotiate openly and honestly
about what was likely to be possible, the opportunities and the risks and how these were best addressed. It was meant to generate a plan that is realistic, in which professionals are transparent about what is possible in stretched health and social care systems, often risk adverse. That doesn’t mean shutting down people’s wishes; but to offer them the earth and then fail to deliver it, is worse than offering nothing at all.
To ensure that this is a reality, we need to better understand what can go wrong. At the conference, Akvile, daughter of a mother who died prematurely, described a series of experiences in which there was no discussion about what her Mum wanted; nor any effort to shape care to meet her preferences. It was clear that this process is not only unsatisfactory for patients, their families and carers but also for many professionals, when it is not done well.
As I reflect on the conference, I am not left questioning the value of ACP, in fact quite the opposite. As our first speaker, Jodie Grace, a paramedic and end of life care champion with London Ambulance Service NHS Trust, recounted, the existence of an electronic Universal Care Plan that clearly spells out someone’s wishes regarding resuscitation and whether they want to go to hospital can have a hugely positively impact on the experience of the individual, their family and the paramedic.
Professionals and the public need to renegotiate ACP’s role and implementation. We must stop using it as a means for professionals to limit people’s care options. Binary choices of home or hospital, resuscitation or not, restrict choice. Instead, we must make it about the focus and nuance of care and the intention to treat.
Those attending the conference were provided with several key pointers for how we can reframe ACP. First was the message that

it needs to draw on a series of meaningful conversations, from which any ‘plan’ is simply an output and not the sole focus or entire process. These conversations, which focus on a negotiated possible future, should be at a time and in a place where people feel like they have the agency, vocabulary and confidence to explore a realistic, deliverable wish list.
Then, we need to focus effort where people are most likely to benefit. Increasing numbers of people with frailty and dementia die in care homes, a trend that is only likely to increase. Care home staff are in the privileged and responsible position of knowing these people better than almost anyone. It’s in everyone’s interests to offer residents and those close to them the chance to tell you about the care they want to receive now and in the future. If it’s more appropriate for their GP to have that discussion, then care home staff should be advocating on behalf of the resident.
The impact of these shifts would be significant. As one delegate put it, if they had truly succeeded in supporting someone with their forward planning, it would help that person feel, ‘included, heard, respected, valued, optimistic and less overwhelmed’. Now that’s an outcome every health professional would be proud of and can aspire to.
This is just the start of the conversation. We’re generating further training which includes reframing the language we use when talking to people about ACP. Too often we use euphemisms and expressions that fail to communicate our intended message. There was a consensus at the conference that ‘Future Planning’ might be a more accessible name for the process. Ultimately, shared death literacy is a target we should all be aiming for. Look out for learning opportunities that help us all achieve this.
50 CMM April 2024
Professor Heather Richardson is Director of Academic Learning and Action at St Christopher’s CARE. Email: education@stchristophers.org.uk X: @StChrisHospice Do you think that Advance Care Planning is fit for purpose? Visit www.caremanagmentmatters.co.uk and leave a comment on this article or join the conversation to share your thoughts.

“NCF provided us with ‘fresh eyes,’ giving us the opportunity to identify the areas we needed more specific focus on”







Specialist, expert consultancy support for care providers covering: www.nationalcareforum.org.uk/projects/ncf-consult/
Cole: jocelyn.cole@nationalcareforum.org.uk
Contact Jocelyn

Yes, that’s right. Absolutely free.
Gain CPD points
Access extended features and additional content
Read latest news email alerts
Comment on features and debate on important subjects
Access archived editorial
Receive a digital edition of CMM (10 issues per year)











FREE PROVIDERS Sign up at www.caremanagementmatters.co.uk @CMM_Magazine SIGN UP
FOR
Designed by Evan Ho buhr










































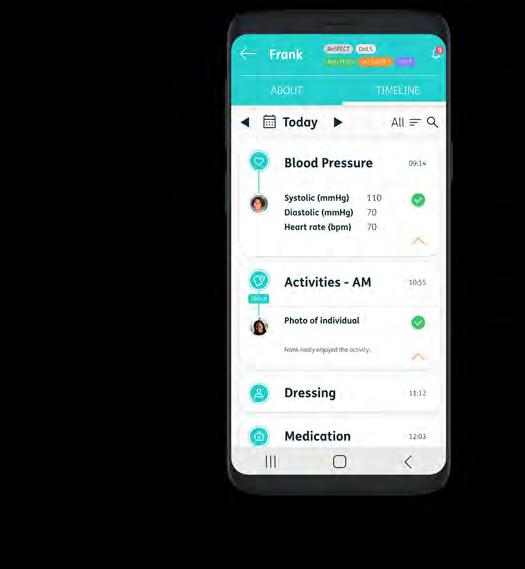





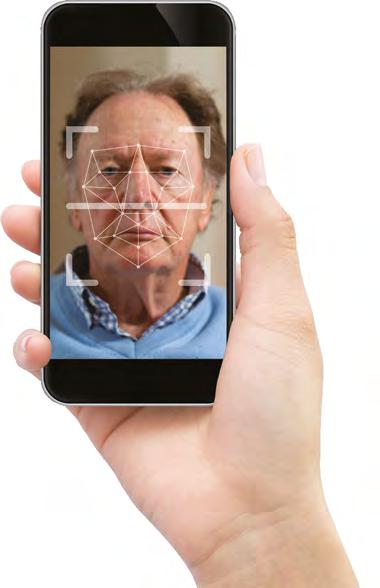
















































 The Dame Esther Rantzen Campaigning for Change Award
The Dame Esther Rantzen Campaigning for Change Award