Did You Know?
Management of head and neck lymphedema

Background: Head and neck (H&N) cancer treatments may have significant side effects that could be physically, functionally, and psychologically debilitating. Head and neck lymphedema (HNL) is a commonly neglected side effect that remains underdiagnosed and understudied. HNL could manifest externally, internally, or both, and could affect as much as 97% of the patients and may profoundly impact vital physical functions. Although the use of compression is well documented for the management of cancer-related lymphedema, to date, current data surrounding the use of H&N night compression and its effect on lymphedema management is sparse.
Methods: Retrospective analysis of H&N patients seen between January 2016 to May 2023. At each time-point, an inventory questionnaire was used to assess symptoms and functional restrictions. In addition, lymphedema was assessed using neck circumferences, facial composites and tragusto-tragus measurements. Management of HNL using compression garment, along with body weight were recorded and compared over time. Results: A total of 86 patients were reviewed (74% males and 25.6% female), with a mean age of 64.6 years. Total neck circumferences: patients wearing compression, 67% showed a reduction with compression, while 41.5% also showed a reduction, however without the use of compression. Total facial composite: no significant change wearing or not wearing compression. Tragus-to-tragus: 57% showed a reduction with compression, however 54.5% also showed a reduction despite not using compression. Conclusion: Our observations suggest that despite the vital use of compression for upper and lower limb lymphedema, patients with HNL tend to be at their worst initially and significantly improve over time. Our analysis indicated that the majority of patients showed a reduction in their HNL despite not using compression




garments. Future research is warranted to establish if interventions other than compression therapy play a role in favorable HNL outcomes, such as H&N exercises and/ or self-massage.
Source: Management of lymphedema related to head and neck cancer. Presented at the 2023 Canadian National Lymphedema Conference by Marize Ibrahim.
Additional
Follow-up of lymphatic surgeries
Background: Lymphovenous anastomosis (LVA) and vascularised lymph nodes transfer (VLNT) are receiving growing attention with an increased number of surgeons being trained in lymphatic surgeries and reporting their own outcomes. We have been independently following patients who have undergone lymphatic surgeries since 2018 with standardized measurements and volume calculation to objectively assess surgical outcomes over time. Methods: Patients who have undergone LVA or VLNT are followed prospectively. Circumference measurements are taken for bilateral extremities pre-surgery and approximately every three months post-operatively for at least two years.

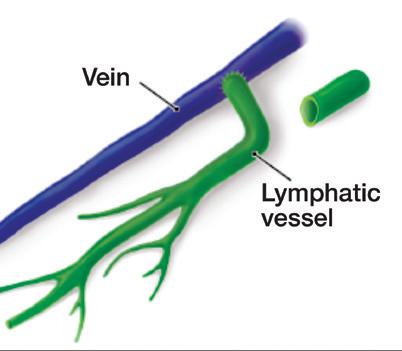
Percentage edema volume is calculated for each limb. Use of compression garments is also recorded at each visit, along with the number of cellulitis episodes. Results: Nine women have been independently followed: 7 with breast cancer-related lymphedema (BCRL), 1 with bilateral primary lower limb lymphedema (LLL) and 1 with bilateral cervical cancer-related LLL. Of the 7 BCRL, 3 had LVA surgery and 4 VLNT. Arm volume measurement increased for 5 women, while a decrease was observed for 2 women. The 2 LLL had LVA procedure: 1 presented with fluctuation in volume over time while the other decreased. Regarding compression, 6 women continued, while 3 stopped, despite volume increase. One episode of cellulitis was recorded post surgery in 3 women. Conclusion: As lymphedema has historically been defined as a chronic condition requiring lifelong care, our results emphasize the benefits and need for longitudinal follow-up
in those who have undergone lymphedema surgeries. It is critical to objectively evaluate post-surgical outcomes of lymphedema, addressing both acute and long-term potential effects. The need for compression garments may also need to be re-evaluated post-surgery as many still require usage, despite the surgical intervention. Longitudinal follow-up with this clientele is essential to better understand the impact of lymphedema surgeries on the lymphatic and venous systems.
Source: Independent prospective follow-up of lymphedema patients who have undergone lymphatic surgeries. Presented at the 2023 Canadian Lymphedema Framework National Conference by Marie-Eve Letellier.
Blood biomarkers of lymphedema
Background: Lymphedema is a common side effect of cancer treatment affecting breast cancer survivors. Patient, cancer, and treatmentrelated factors contribute to the risk of its development. Circulating inflammatory cytokines are not currently used in routine clinical practice for prognostication and their role in predicting lymphedema risk remains unclear. Methods: The study population comprised of a subgroup of breast cancer survivors who participated in a radiotherapy cytokine study from 2010-14. Lymphedema-associated cytokines of interest included IL-4, -6, -17 and TGF-β1. Clinical and integrative risk models were developed to predict the occurrence of lymphedema. The established clinical risk model included age, body mass index, breast density, pathological lymph node burden, and axillary lymph node dissection. Recursive partitioning analysis (RPA) was implemented to develop an integrative model incorporating essential inflammatory cytokine prognostic biomarkers. The discriminative performances of the clinical and integrative risk models were compared using the concordance index (C-index). Results: There were 88 breast cancer survivors who were eligible for the analysis. A total of 10 lymphedema events (11%) occurred within the median follow-up time of 4.9 years [IQR 2.8-8.0]. Using RPA, the change in circulating IL-4 levels post-radiotherapy was a novel prognostic factor for lymphedema risk, which improved the C-index from 0.73 (clinical model) to 0.92 (integrative model, p=0.019). Conclusion: An integrative risk model incorporating circulating cytokine levels resulted in improved prognostication of lymphedema risk and may be useful for triaging patients for earlier management and/or future trials.
Source: Evaluating radiotherapy-induced circulating cytokine levels as predictors of lymphedema risk. Presented at the 2023 Canadian Lymphedema Framework Conference by Jennifer Kwan. Additional authors: M.Hossack, F.Johri, W.Shi, K.Yip, E.Chow, F.Liu
