2 Guest editorial Redefining ‘optimal medical therapy’ for vascular patients

5 Complex aortic TBE ‘safer’ option than TEVAR for BTAI in setting of zone 2 coverage, new data show


2 Guest editorial Redefining ‘optimal medical therapy’ for vascular patients

5 Complex aortic TBE ‘safer’ option than TEVAR for BTAI in setting of zone 2 coverage, new data show

A multi-institutional analysis has demonstrated fenestrated endovascular aneurysm repair (FEVAR) could be a “safer and more durable option” than chimney EVAR (ChEVAR) in elective juxtarenal abdominal aortic aneurysm (AAA) cases with suitable anatomy, offering potentially “greater generalizability to real-world practice.”
10 The Outpatient The pursuit of academic research in community practice
14 Obituary Vascular community mourns loss of renowned investigator

www.vascularspecialistonline.com
By Marlén Gomez
THE SOCIETY FOR VASCULAR Surgery (SVS), in collaboration with the Society for Vascular Nursing (SVN) and the American Podiatric Medical Association (APMA), has designed an interprofessional curriculum to meet the needs of vascular wound care teams. As the collaborating organizations emphasize, this initiative marks the first of its kind in vascularspecific wound care.
The organizations have shared several promotional videos on social media featuring specialists who promote the course, highlighting the necessity of collaboration between the organizations.
“To prevent amputations takes a team—you can have the best vascular surgeons in the world and the best podiatrist, and if they’re not part of a cohesive team that includes ultrasound techs, nurses, nurse practitioners, advanced providers and wound care people, you’re not going to get the results that you want,” said Joseph Mills, MD, Reid professor and chief of the Division of Vascular Surgery and Endovascular Therapy at Baylor College of Medicine in Houston, in one of the circulating videos.
The Wound Care Curriculum is a combination of on-demand content and an in-person hands-on workshop. The SVS VascuLEARN platform includes 27 on-demand short videos covering essential wound care topics for the online portion. Registrants can purchase the online module independently or participate in a hands-on workshop immediately following the Vascular Annual Meeting (VAM) in New Orleans on June 7.
Additional workshops will be held in conjunction with VAM 2026 and VAM 2027. Each workshop will focus on hands-on practical application
Medical Editor Malachi Sheahan III, MD
Associate Medical Editors
Bernadette Aulivola, MD | O. William Brown, MD | Elliot L. Chaikof, MD, PhD
| Carlo Dall’Olmo, MD | Alan M. Dietzek MD, RPVI, FACS | John F. Eidt, MD | Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS | Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray L. Shames, MD | Niten Singh, MD | Frank J. Veith, MD | Robert Eugene Zierler, MD
Resident/Fellow Editor
Saranya Sundaram, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Senior Director for Public Affairs and Advocacy
Megan Marcinko, MPS Manager of Marketing
Kristin Spencer
Communications Specialist Marlén Gomez
Published by BIBA News, which is a subsidiary of BIBA Medical Ltd.
Publisher Stephen Greenhalgh
Content Director Urmila Kerslake
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution Jocelyn Hudson, Will Date, Jamie Bell and Éva Malpass
Design Josh Lyon
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe
526 Fulham Road, London SW6 5NR, United Kingdom
BIBA Medical, North America
155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA News. Content for the news from SVS is provided by the Society for Vascular Surgery. The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA News will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. | The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | POSTMASTER: Send changes of address (with old mailing label) to Vascular Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com | For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA News. | Printed by Ironmark | ©Copyright 2025 by the Society for Vascular Surgery
By Sophie Wang, MD, Lars Stangenberg, MD, Glenn LaMuraglia, MD, and Allen Hamdan, MD
Vascular and endovascular surgeons are frequently the only specialists other than primary care involved in the longitudinal care of their patients afflicted with clinically active vascular disease. As such, while scrutinizing the longitudinal and periprocedural outcomes in their patients, involvement in the management and counselling of the patients and their primary care provid ers in their cardiovascular risk factor modi fication has become a logical sequence of their overall care. The ongoing effort of understanding procedural and patient outcomes towards quality improvement has led to significant standardization of vascular interventions along the whole spectrum of care—from preoperative evaluation to postoperative surveillance.

panels to evaluate whether patients are meeting their low-density lipoprotein (LDL) targets, and hemoglobin A1C levels may be noted, but these are also deferred to the patients’ medical providers. As such, though it may be noted, surgeons often fail to take a broader view of the patient’s metabolic health in their assessments and planning of their procedures. Metabolic syndrome is one of the strongest predictors of cardiovascular outcomes—it is associated with higher rates of death, stroke and myocardial infarction.3–5 These predictors, which can be considered to reflect “optimal metabolic health,” are quantified by five metrics: systolic blood pressure, fasting blood glucose, high-density lipoprotein (HDL) cholesterol levels, triglyceride levels and waist circumference (body mass index). Current cross-sectional population studies have identified that only 10–20% of the American population is metabolically healthy.6 The rates are alarmingly low, even in normal-weight individuals. A recent report calculated that 60% of the U.S. population would be eligible for “weight-loss drugs” like Ozempic.7 This would obviously be higher in patients with vascular disease.

The term “optimal medical therapy” (OMT) is often used within this framework to describe the standard pharmacological management of vascular patients. In practice, this equates to an antiplatelet agent, usually aspirin, and an aggressive first-line cholesterol-lowering medication, typically a statin. However, this onesize-fits-all approach to pharmacologic management of cardiovascular risk factors may be insufficient in improving long-term outcomes. Recent data from the Vascular Quality Initiative (VQI) raises concerns about the efficacy of the current paradigm. A recent analysis of survival rates for patients with chronic-limb threatening ischemia, with 87% on aspirin and 86% on a statin, reported a dismal 30% five-year survival rate.1 The majority of these patients were on OMT, yet their longevity was dismal. This raises the question: does the use of statins and aspirin represent OMT? Clearly, the definition of OMT needs to be reconsidered and possibly redefined to improve the longevity and outcomes of this patient population.


The primary cardiovascular risk factors that vascular surgeons and primary care physicians currently focus on include smoking, dyslipidemia (particularly hypercholesterolemia), hypertension, chronic kidney disease (CKD) and diabetes. In most practices, vascular surgeons may take a few minutes during a clinic visit to discuss with the patient a plan for individual risk-factor modification. The first focus is often on smoking. But smoking cessation is notoriously difficult—less than 10% of smokers who tried quitting were successful in 2022.2 Many surgeons will offer general advice to patients to use the Quitline or a nicotine patch, but few are organized to provide targeted resources or a well-structured plan. Often, hypertension and CKD are acknowledged as they relate to periprocedural considerations, but the management is deferred to the patient’s medical providers. Similarly, lipid


To identify patients with metabolic syndrome, one of the most important things to quantify and target is insulin resistance. This hallmark of metabolic syndrome can be easily quantified in a clinic setting, either through a HOMA-IR (homeostatic model assessment for insulin resistance), which is based on fasting glucose and insulin, or through a surrogate marker like the triglyceride to high-density lipoprotein ratio (TG/HDL). A TG/HDL ratio above 1.5 suggests metabolic syndrome, and a ratio above 4 strongly predicts extensive coronary disease.8 Many patients have lipid panels readily available, and those that have significant insulin resistance or dyslipidemia—especially in the setting of early onset of cardiovascular disease or recurrent treatment failures—may benefit from targeted counseling. This centers on high-yield dietary changes and involves focus on simple, practical diet modifications to reduce refined carbohydrates and increase healthy fats and proteins. Most patients are very receptive to this type of counseling and, over time, with these changes can reverse their insulin resistance and stop their diabetes medications with simple lifestyle changes.9
Managing vascular patients requires an integrated approach to address the underlying metabolic abnormalities that drive vascular disease progression
As vascular surgeons have the privilege of following their patients longitudinally and have their patients as a captive audience, this presents a unique opportunity to make a greater impact on patient outcomes by altering their risk factors, including metabolic syndrome. Vascular surgeons are more than just proceduralists—they are continued on page 4

Available in 12mm, 14mm, and 16mm Large Diameter
6-MONTH ARTERIOVENOUS FISTULA (AVF)
TARGET LESION PRIMARY PATENCY – COVERED STENTS VS. PTA*
6-MONTH ARTERIOVENOUS GRAFT (AVG)
TARGET LESION PRIMARY PATENCY – COVERED STENTS*

‘How to thrive, not just survive, as a vascular
By Bryan Kay
Outgoing Vascular & Endovascular Surgery Society (VESS) President Misty Humphries, MD, used her presidential address to outline how trainees and young vascular surgeons can “thrive and not just survive as a vascular surgeon.”
The University of California, Davis interim chief of vascular surgery provided five lessons she has learned to help enable her success.
Working in reverse order, she opened with a call to “maintain connection beyond your immediate circle.” Humphries said: “Not everyone you meet will stay with you for the entire length of your journey, and that’s OK, because those people were only meant to be there for that moment. But the people who
matter—they will be there at the finish line.”
Next, she urged those gathered to “celebrate and remember the good things.” Vascular surgeons are notoriously supersti tious, Humphries said, but urged, “Find a way to keep track of the wins.”
Also, she said, “let go of the emotions that are not serving you.”
Vascular surgeons tend to hold themselves to impossible standards, she noted, “constantly replaying the things we should have done differently, but perfectionism is an illusion, and it doesn’t make you better—a lot of times it will just make you feel worse.”

stroke after a carotid repair, a failed bypass leading to limb loss. Invoking the world of sports, she said, “The great masters recognize the difficulty, and they repeatedly run back into the fire. It’s part of their job—it’s part of our job, part of our lives.” If greatness is the goal, Humphries added, “then there will be no balance.”
Finally, she said,
“Surrender to the hard, let go of the idea of balance,” Humphries continued. Vascular surgery has some of the highest stakes in all of medicine, she said. Paralysis after an aneurysm repair,
“Perfectionism is an illusion, and it doesn’t make you better—a lot of times it will just make you feel worse”
MISTY HUMPHRIES
advocates for comprehensive, long-term care and want their patients to have the best possible outcomes. We can work closely with primary care providers to better optimize medication management, particularly when LDL cholesterol and blood pressure targets are not met.
In addition, we can advocate to check lipoprotein(a) levels, especially in precocious patients with atherosclerosis or those with very positive family history, as 20% of the population will be positive, and it is becoming the most potent predictor of adverse outcomes.10 Patients can be counseled on dietary changes and we can advocate for daily exercise programs. Those who may benefit from GLP-1 receptor agonists and SGLT-2 inhibitors can be identified and referred to endocrinologists or other medical providers trialing these medications for our patients with diabetes and CKD in whom mortality and renal protective benefits have been demonstrated.11
The key takeaway is that OMT needs to be redefined into a broader concept in patients with vascular disease, encompassing optimal metabolic health, rather than simply a checklist of medications. Managing vascular patients requires an integrated approach to address the underlying metabolic abnormalities that drive vascular disease progression. The focus should be expanded to include not only traditional medications but also lifestyle modifications, especially diet, exercise and emerging therapies that target the root causes. Ultimately, by adopting a more comprehensive approach to managing vascular patients, both short-term outcomes and long-term survival rates can be improved.


There is much to gain for our patients as vascular specialists need to embrace this new path forward—one where the patient’s care provided is truly “optimal” in every sense of the word.
“the best way to thrive as a vascular surgeon is to stand up, even if you are the only one in the room standing.” Vascular surgery is difficult,” Humphries said. “Not everyone understands it, quite honestly, and I think we have to give a little bit of grace there sometimes.”
Meanwhile, at the close of the meeting, Ravi Ranjani, MD, a professor of surgery at Emory University School of Medicine in Atlanta, took over as VESS president.
St. Mary’s Regional Hospital in Grand Junction, Colorado, became the first community hospital to receive designation as an American College of Surgeons (ACS)/SVS Vascular Verification Program (Vascular-VP) center in November 2024.
“This is truly a great honor for St. Mary’s Hospital to be recognized as one of the first nationally verified programs,” said Bryan Johnson, president of Intermountain St. Mary’s Regional Hospital.
Tej Singh, MD, MBA, the institution’s medical director of vascular surgery, spearheaded the successful verification.
“We’re grateful to Dr. Singh for his instrumental work in building a highquality vascular program and achieving vascular verification. His efforts have included improving patient access, working with the Vascular Quality Initiative registry, ensuring national accreditation, compliance in care, and mentoring,” said Ben Smalley, chief operating officer.
continued from page 2
References
1. Levin, S. R. et al. Five Year Survival in Medicare Patients Undergoing Interventions for Peripheral Arterial Disease: a Retrospective Cohort Analysis of Linked Registry Claims Data. Eur. J. Vasc. Endovasc. Surg. 66, 541–549 (2023).
2. VanFrank, B. et al. Adult Smoking Cessation — United States, 2022. MMWR. Morb. Mortal. Wkly. Rep. 73, 633–641 (2024).
3. Hosseini, K. et al. The association between metabolic syndrome and major adverse cardiac and cerebrovascular events in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Sci. Rep. 14, 697 (2024).
4. Lakka, H.-M. The Metabolic Syndrome and Total and Cardiovascular Disease Mortality in Middle-aged Men. JAMA 288, 2709 (2002).
5. Sundström, J. et al. Clinical value of the metabolic syndrome for long term prediction of total and cardiovascular mortality: prospective, population based cohort study. BMJ 332, 878–882 (2006).
6. Araújo, J., Cai, J. & Stevens, J. Prevalence of Optimal Metabolic Health in American Adults: National Health and Nutrition Examination Survey 2009–2016. Metab. Syndr. Relat. Disord. 17, 46–52 (2019).
7. Shi, I. et al. Semaglutide Eligibility Across All Current Indications for US Adults. JAMA Cardiol. (2024). doi:10.1001/jamacardio.2024.4657
8. Sultani, R. et al. Elevated Triglycerides to High-Density Lipoprotein Cholesterol (TG/HDL-C) Ratio Predicts Long-Term Mortality in HighRisk Patients. Hear. Lung Circ. 29, 414–421 (2020).
9. Unwin, D. et al. Insights from a general practice service evaluation supporting a lower carbohydrate diet in patients with type 2 diabetes mellitus and prediabetes: a secondary analysis of routine clinic data including HbA1c, weight and prescribing over 6 years. BMJ Nutr. Prev. Heal. 3, 285–294 (2020).
10. Nordestgaard, B. G. et al. Lipoprotein(a) as a cardiovascular risk factor: current status. Eur. Heart J. 31, 2844–2853 (2010).
11. Bhattarai, M. et al. Association of Sodium-Glucose Cotransporter 2 Inhibitors With Cardiovascular Outcomes in Patients With Type 2 Diabetes and Other Risk Factors for Cardiovascular Disease. JAMA Netw. Open 5, e2142078 (2022).
SOPHIE WANG, LARS STANGENBERG, GLENN LAMURAGLIA, AND ALLEN HAMDAN are Boston-based vascular surgeons.
The Vascular-VP is an ACS Quality Program developed in collaboration with the SVS. This program leverages the strengths of both organizations to create a standardized, evidence-based process to enhance quality improvement and clinical care within vascular programs.
The Vascular-VP offers two levels of participation—one for inpatient centers and one for outpatient centers. As a verified center, St. Mary’s Regional Hospital has also earned the designation of ACS Surgical Quality Partner. Centers seeking verification and a pathway to enhance the quality of their vascular services can find additional information at vascular.org/Verification.—Marlén Gomez
SEMAGLUTIDE SIGNIFICANTLY improved maximal walking distance in people with symptomatic peripheral arterial disease (PAD) and type 2 diabetes in the STRIDE trial designed to evaluate the use of a GLP-1 agonist to manage PAD. The main findings of the trial were presented during the American College of Cardiology (ACC) 2025 scientific session in Chicago (March 29–31) and simultaneously published in The Lancet.— Will Date
By Bryan Kay
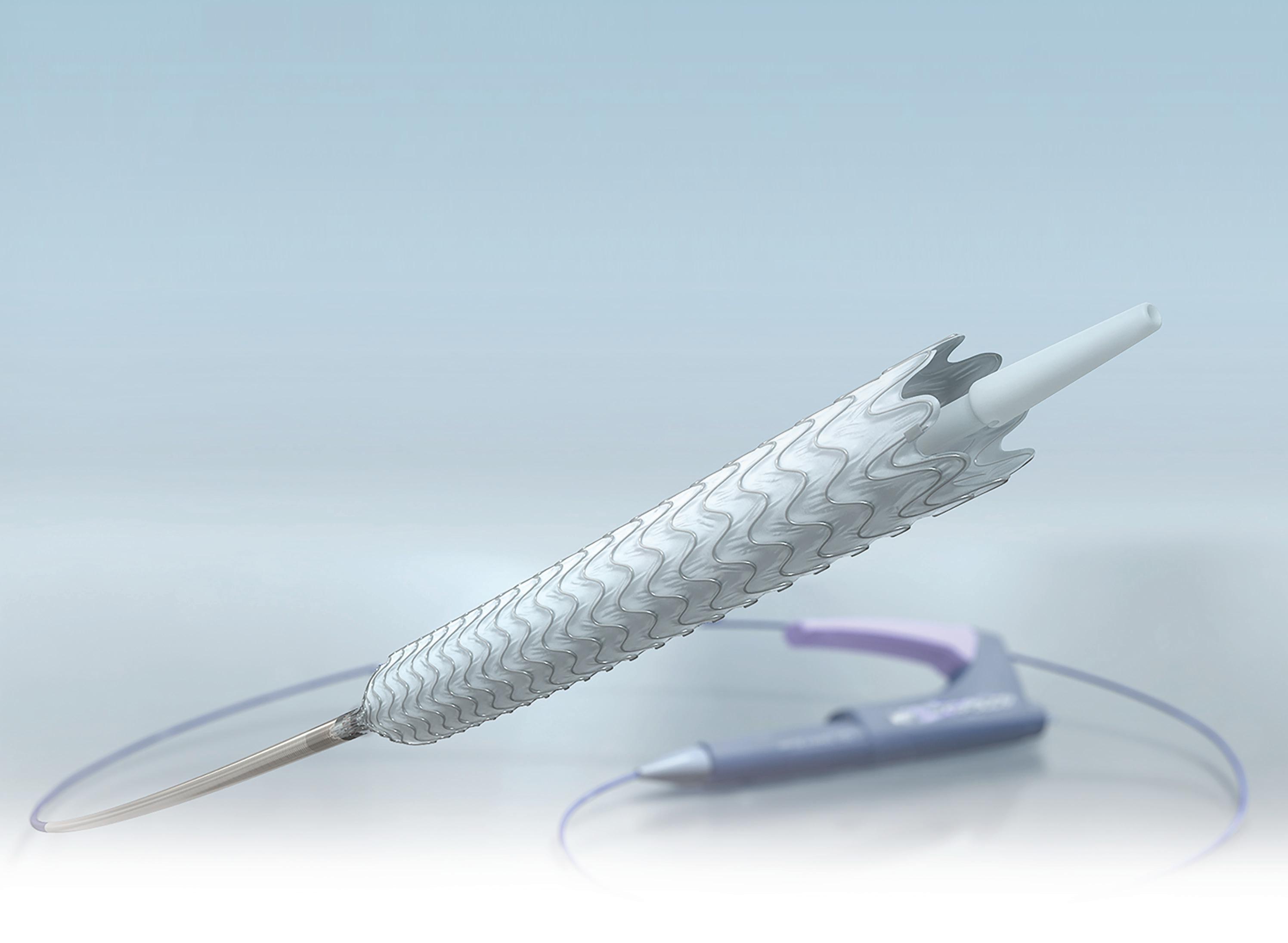
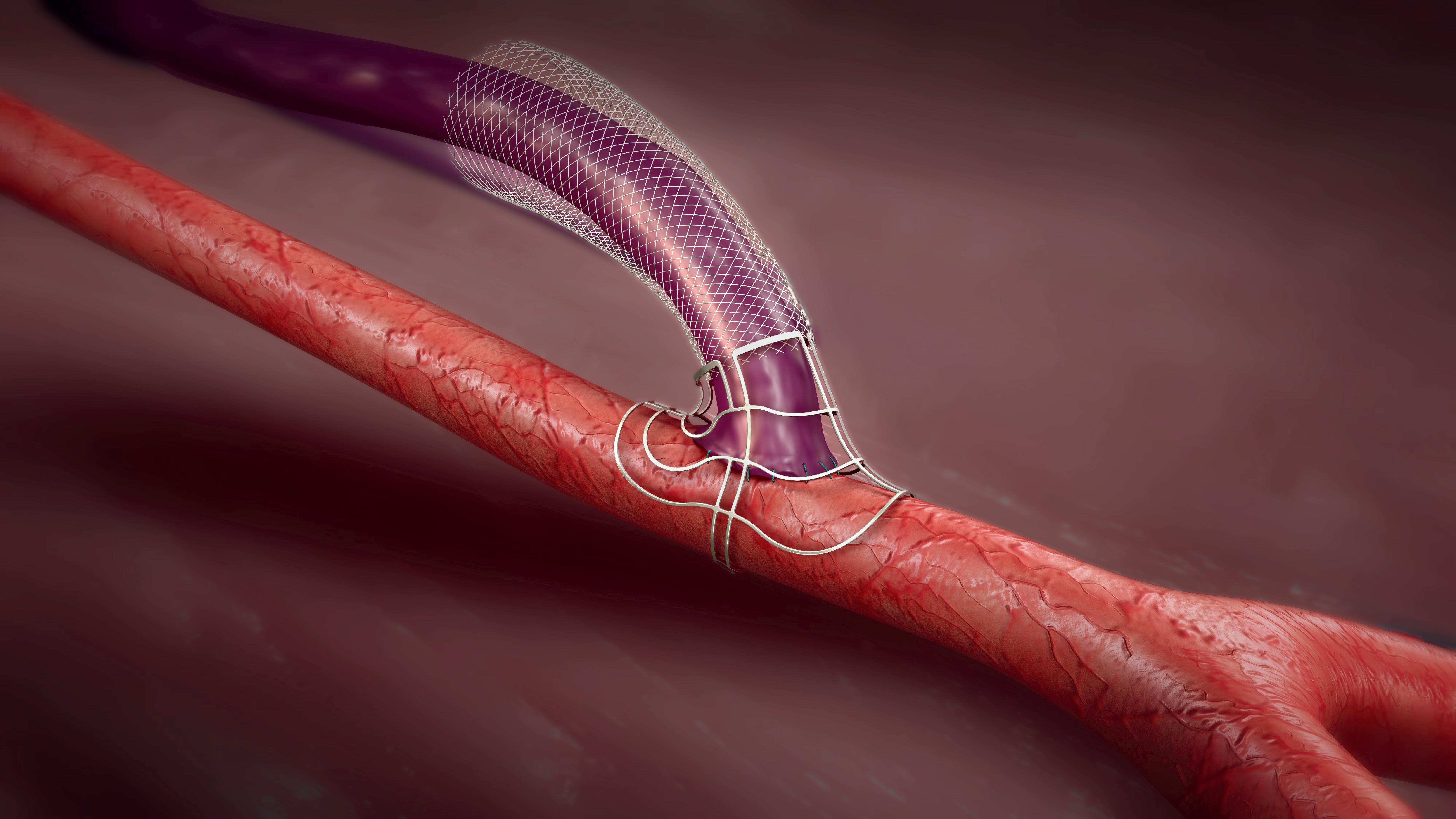
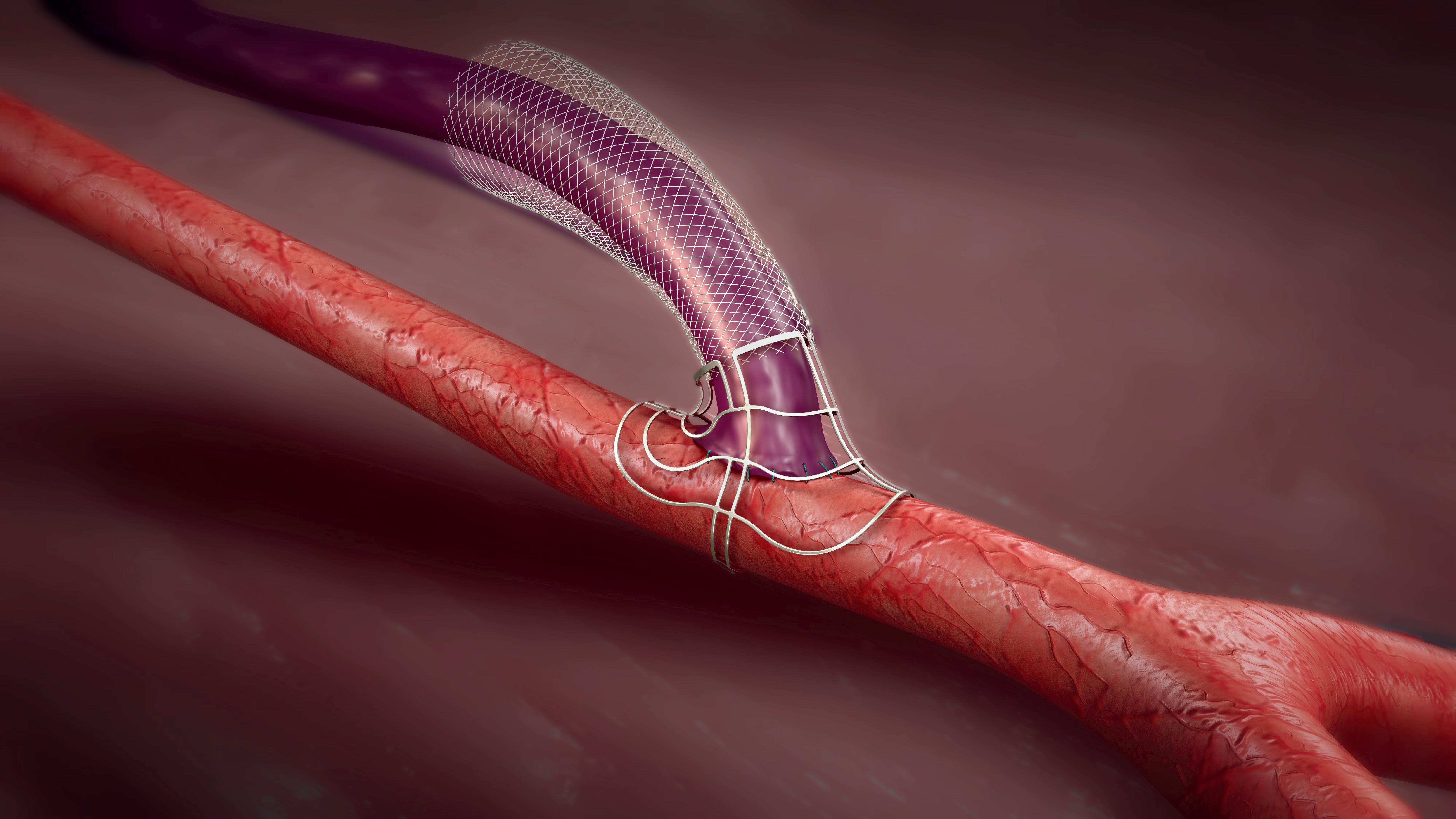
USE OF THE GORE TAG THORACIC BRANCH endoprosthesis (TBE) “offers a safer alternative” to traditional thoracic endovascular aortic repair (TEVAR) with left subclavian artery (LSA) coverage in blunt thoracic aortic injury (BTAI) requiring zone 2 coverage for zone 2 or proximal zone 3 injuries without requiring a concomitant or delayed subclavian revascularization, according to a new study delivered at the 2025 Society for Clinical Vascular Surgery (SCVS) Annual Symposium in Austin, Texas (March 29–April 2).
Kathryn DiLosa, MD, a vascular surgery resident at the University of California, Davis in Sacramento, California, revealed how from 2005–2024, 13 patients had TBE repair for BTAI at UC Davis, with 48 receiving TEVAR with LSA coverage. Technical success—device delivery with ex clusion of injury—was 100% in both groups. Among the TEVAR cohort, nine patients had LSA revas cularization. There were no complications in the TBE cohort, DiLosa and colleagues found, while 12 patients in the TEVAR cohort experienced a complication, including wound infection, arm ischemia, stroke, endoleak and retrograde dissection. No aortic-related mortalities were observed. TBE side branch patency
and BTAI exclusion was 100% at mean follow-up of 18.5 days. Similarly, BTAI was excluded in all TEVAR patients at follow-up.
The UC Davis experience is characterized by the institution’s geographical surroundings in tandem with its early access to the TBE device, explains DiLosa in an interview prior to SCVS 2025. “Here at UC Davis, we are surrounded by tons of very rural highways—mountain highways—so there is a lot of blunt trauma that we deal with,” she says. “As a result, we have a massive collection of patients who have had prior blunt thoracic aortic injuries that we have managed and that has given us a nice cohort to look at some unique features of those injuries and the management of them.”

DiLosa highlights the significance of the UC Davis findings: “Previously, it has been suggested covering the LSA is reasonable, especially if somebody has a bad injury, and they just need it done quickly, where you can come back later. This has been the teaching. But I think now, as we’re seeing new devices that offer something that can be done relatively quickly and efficiently with an off-the-shelf device, our recommendations need to change to match the evolution of endografts.”
The data, says DiLosa, confirm a number of prior studies showing that “15–30% of patients that have coverage of the left subclavian may need revascularization at some point or other.
“We observed that roughly 20% of patients in our cohort needed revascularization for one reason or another, or had revascularization. When you are considering that one-infive patients that gets a repair for an emergent situation will potentially need a bypass, our practice has generally shifted to use the TBE device in any repairs that are going to require coverage of the left subclavian, because, in our experience, we are fairly facile with the device and we are able to complete that repair in just over an hour.”
When the device is available, the TBE should be considered if coverage of the LSA is required to prevent adverse outcomes, DiLosa and colleagues conclude. “One thing that should be made clear is that not all patients with a blunt aortic injury need a repair that involves coverage of the subclavian artery,” DiLosa adds. “However, when coverage is necessary, a branched endograft maintains subclavian artery perfusion, and minimizes stroke and extremity ischemia risk.”
“Here at UC Davis, we are surrounded by tons of very rural highways—mountain highways— so there is a lot of blunt trauma that we deal with”
KATHRYN DILOSA
CHEVAR WAS ASSOCIATED WITH significantly higher rates of type I endoleak and reintervention than FEVAR in a study of juxtarenal AAA cases carried out at five geographically distinct institutions with high-volume centers, the 2025 Society for Clinical Vascular Surgery (SCVS) Annual Symposium in Austin, Texas (March 29–April 2), heard. In addition, FEVAR patients demonstrated significant sac regression, while those undergoing ChEVAR showed “a concerning trend” of early sac regression followed by late re-expansion.
The study data were delivered by Clayton Brinster, MD, an associate professor in the Section of Vascular Surgery and Endovascular Therapy at UChicago Medicine and the co-director in the institution’s Center for Aortic Diseases. Each center enrolled at least 25 consecutive cases of FEVAR and/or ChEVAR, Brinster explained. Some 130 cases were analyzed in total: 77 FEVAR and 53 ChEVAR. Significantly more patients in the ChEVAR group had persistent type I endoleak at one year—15 of the 53 patients, or 28%— vs. 6/77, or 7.8%, following FEVAR. Ten reinterventions were required in 8 of 77 (10.4%) FEVAR patients vs. 20 reinterventions in 16 of 53 (30.2%) ChEVAR patients. Significant sac regression was seen at 12 months (55mm, -7mm) and 24 months (51mm, -11mm) following FEVAR, Brinster told SCVS 2025. Sac regression was not significant at 12 months (59mm, -5mm) following ChEVAR, and sac re-expansion was observed in this group between 12 and 24 months (59 to 63mm, +4mm), he added.
Speaking to Vascular Specialist ahead of the meeting, Brinster said the multi-institutional consortium behind the data was started four years ago and sought to elucidate granular institutional data on two widely used techniques.
“Although FEVAR and ChEVAR have both been around now for over a decade, there is a lack of granular institutional data,” he explained. “There have been maybe five or six solo institutional studies that incorporate some degree of parallel stenting versus FEVAR, but most include a comparison to open surgery or branched devices, or PMEGs [physician-modified endografts], so the data are not so clean. Besides that, it’s really just registry data with short-term follow-up.”
Brinster said the consortium’s strength is not only rooted in the fact it is regionally diverse, but it has also produced “granular institutional data.” The medical centers involved include the University of Chicago, Ochsner Health in New Orleans, NYU Langone Medical Center in New York City, the Mayo Clinic, in Scottsdale, Arizona, and the University of Rochester in Rochester, New York. “The data is therefore perhaps more generalizable to other institutions,” he continued. “It offers that advantage when compared to either national registry data or the U.S. Aortic Research Consortium, because those are very sophisticated surgeons at the very best centers with the very best imaging, with carefully selected patients in general.”
“Although FEVAR and ChEVAR have both been around now for over a decade, there is a lack of granular institutional data”
CLAYTON BRINSTER
continued from page 1
Brinster said that some may argue the fact there were more endoleaks and reinterventions with ChEVAR was “a foregone conclusion,” but noted that there are many surgeons in the field who are experienced with parallel grafting and produce good results. In effect, the study aimed to answer—“for once and for all”—which of the two techniques is better.
“With fenestrated grafting, there are anatomic constraints, and many patients fall outside the IFU [instructions for use],” he said. “ChEVAR has both the advantage of possibly being able to treat those patients and the disadvantage that inherently those patients are more anatomically complex and more prone, perhaps, to gutter leak, endoleak and reintervention.”
Looking into sac behavior, Brinster pointed out the “unexpected” finding of FEVAR inducing sac regression. In the early stage, he said, ChEVAR induced sac regression, “but when we looked out to two years, there was a statistically significant increase in sac size, and that is particularly concerning.”
“I wanted to look into this because it has become an increasingly hot topic in our field,” he added. “It has been linked to late rupture, late intervention and late mortality after EVAR. There are some data out there looking at those outcomes for standard EVAR, but they only go out to one year in those studies—and it is registry data. There are two industry-sponsored registries looking at sac behavior after EVAR at one, three and five years, and that was the basis whereby now Medtronic can firmly recommend endoanchors, or ESAR [endosuture aneurysm repair], in certain anatomic circumstances to improve late outcomes by inducing sac regression. The main pinnacle there was that even stable sac size over time was linked to late poor outcomes.”
A novel classification of aneurysms could provide an additional data point to help improve aneurysm risk stratification, according to a new study.
By Bryan Kay
INSPECTION OF AORTIC LUMEN , wall and thrombus volume changes throughout the cardiac cycle enables novel classification of abdominal aortic aneurysms (AAAs) into four types “representing the complex wall-lumen-thrombus interaction,” a new study delivered during the 2025 Critical Issues America (CIA) in Aortic Endografting meeting in Miami (Feb. 7–8) showed.
The finding is among the latest results brought by Randy Moore, MD, a vascular surgeon at the University of Calgary in Alberta, Canada, who is one of the driving forces behind an emerging technology aimed at providing an algorithm-driven route to precision care—RAW (Regional Areas of Weakness) Maps (ViTAA Medical Solutions).
The current investigation of the technology from Moore and colleagues involves patients who were selected from two studies—one including patients who underwent surgical repair of AAA from 2016–2023, and those in a retrospective study of AAA growth at 12 months based on surveillance imaging,
also from 2016–2023. Multiphase computed tomography (CT) of 14 patients were obtained from Peter Lougheed Hospital in Calgary, with the geometries of the aortic wall and lumen segmented from the images, Moore explained.
Writing in the Journal of Vascular Surgery-Cases, Innovations and Techniques (JVSCIT), where the findings were recently published, Moore and colleagues—led by first author Alice Guest, PhD, from the University of Calgary’s Department of Biomedical Engineering—laid out how “the relative changes of wall, lumen and thrombus volumes throughout the cardiac cycle classified AAAs into the four types.” These are described as type I (aneurysms with a minimal wall movement, negative lumen expansion and positive intraluminal thrombus expansion); type II (aneurysms whose lumen undergoes small expansion, while the expansion is accommodated by the intraluminal thrombus and wall); type III (a transition type characterized by lumen, wall and thrombus expansions);
continued from page 1
of wound care procedures/techniques and showcase advancements. The 2025 workshop will focus on debridement techniques, dressing management and oxygen therapy.
“Our APMA members, podiatrists, collaborate with members of the SVS and SVN every day to care for patients, so it makes sense for us to work together at the association level to put on the Wound Care Curriculum,” said Dyane E. Tower, DPM, vice president of clinical affairs and the medical director of the APMA.
Tower points out that collaboration and the Wound Care Curriculum highlight the increasing focus on teamwork among professions and that “each provider type has a specific role to fill in caring for these patients.”
VAM has previously presented content on wound care, but the results from the 2021 and 2024 Educational Needs Assessments revealed significant gaps in wound care knowledge and practices within vascular teams.
In response to these findings, Alisha Oropallo, MD, and Kathleen Raman, MD, developed a comprehensive Wound Care Curriculum to address these issues. Both vascular surgeons presented the concept of the curriculum through an official business plan request to the SVS Education Council. Following approval of the concept, the SVS team worked to formally partner with the SVS PA Section, the SVN and the APMA.

Randy Moore
and type IV (characterized by lumen expansion matching or exceeding wall expansion, while the thrombus exhibits very small or negative deformation).
This phenotypic classification of AAA based on complex interactions has not been previously described, Moore and colleagues reveal. The AAA classification system can improve the assessment of clinical risk for aneurysms, they report, with type I “associated with a stiff aneurysm wall that resists thrombus deformation and may be related to the risk of dissection.” Types II and III are “transition types,” and type IV “is associated with the formation of permeable channels and thrombus cracks which may indicate possible risk of rupture.”
At CIA 2025, Moore described how ViTAA analysis of the aortic wall during 4D scanning identifies wall weakness (RAW Maps), concluding, “4D analysis of wall-lumen-thrombus kinematics allows for phenotypical classification of the aortic wall.”
“4D analysis of walllumen-thrombus kinematics allows for phenotypical classification”
RANDY MOORE
Oropallo calls the curriculum “groundbreaking, as it fills a critical educational gap for interdisciplinary vascular wound care teams.”
Through its hybrid course, the Wound Care Curriculum will offer registrants “a foundational understanding of vascular wounds and then exposure to real-world cases that are addressed in daily practice,” said Orapallo.
Alan J. Block, MD, DPM, a podiatry specialist, shared his perspective on the potential impact of a unified approach to wound care. Drawing from his experience at Ohio State University, Block illustrated how a thorough understanding of patients’ health issues could lead to more effective treatment. For instance, he noted the importance of interpreting ankle-brachial index (ABI) test results, stressing that even subtle abnormalities, such as a reading of 0.9, require urgent attention, especially in asymptomatic patients.
“We wouldn’t ignore a cancer diagnosis until it reaches stage four; similarly, we must address vascular issues before they escalate,” said Block. He detailed the significance of monitoring ABI values, explaining that higher readings could indicate calcification, progressing toward critical limb ischemia if left untreated. Block will participate as faculty in the masterclass workshop in June.
The curriculum offers continuing medical education (CME), continuing education units (CEUs) and continuing education (CE) credits in podiatric medicine, ensuring that participants are wellequipped to tackle the challenges of vascular wound care in the future.
“Our mission is to equip healthcare professionals with the knowledge and skills to provide state-of-the-art care, ultimately improving patient outcomes and enhancing the quality of life for countless individuals facing vascular wounds,” said Raman.
To learn more, visit vascular.org/WoundCare
THE IMPORTANCE OF RADIATION safety training for vascular surgery trainees was highlighted by a recent study that detailed a learning curve effect between first- and second-year fellows performing fluoroscopically guided interventions.
Using optically stimulated dosimeters fitted outside and under lead aprons, researchers at the University of Texas (UT) Southwestern in Dallas detected that median thyroid (82μGy vs. 44μGy; p=0.009) and sternal (89μGy vs. 54μGy; p=0.007) radiation dose was significantly higher for postgraduate year (PGY) 6 (first year) compared to PGY7 fellows.
“When we analyzed regional doses, these were significantly higher for firstyear fellows in comparison to second-year fellows,” explained the study’s presenting author Antonio Solano, MD, a UT Southwestern postdoctoral research fellow.
“There was a higher DAP [dose area product] for second-year fellows, higher thyroid and sternum doses for the firstyear fellows, and the procedure scatter fractions were also higher for the first-year fellows.”
The data were presented during the 2025 Southern Association for Vascular Surgery (SAVS) annual meeting in St. Thomas, the U.S. Virgin Islands (Jan. 22–25).
Solano set the scene by pointing to the existence of better radiation safety training and awareness of best clinical practices for fellows in other interventional specialties. While there is variation in radiation safety training institution-to-institution, he said, vascular surgery trainees tend to learn techniques on the job, “which can result in higher radiation exposure.”
The researchers analyzed radiation exposure for patients, vascular surgeons and trainees during interventions according to level of training in a prospective cohort study over a five-month period.
Operator radiation dose was calculated based on a calibration coefficient factor to estimate radiation at 80kVp. Procedural reference air kerma (RAK), fluoroscopy time, DAP and patient body mass index (BMI) were recorded. Meanwhile, scatter fractions were measured with thyroid and sternum counts to DAP ratio and DAP/ RAK ratio.
“When we analyzed the outcomes for attending surgeon dose, we saw that there were no statistical differences between when they were either operating with the first-year fellows versus the second-year fellows,” Solano added.—Bryan Kay
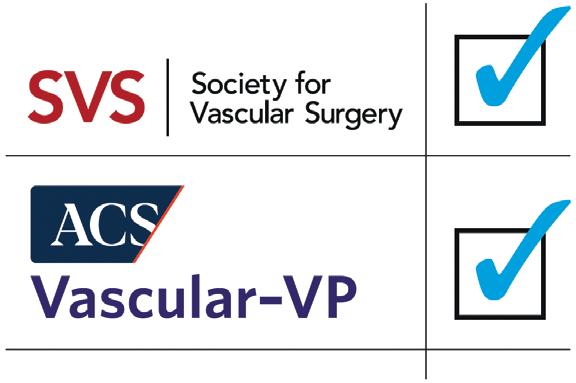
Addresses vessel recoil and dissection1, with radial strength similar to a metallic stent within the first 6 months2
Inhibits restenosis and maximizes patency through sustained everolimus elution3
Preserves flexibility for the future with complete resorption4

Proven With 2-Year RCT Data INDICATIONS
Esprit™ BTK Everolimus Eluting Resorbable Scaffold System
INDICATIONS
The Esprit™ BTK Everolimus Eluting Resorbable Scaffold System is indicated for improving luminal diameter in infrapopliteal lesions in patients with chronic limb-threatening ischemia (CLTI) and total scaffolding length up to 170 mm with a reference vessel diameter of ≥ 2.5 mm and ≤ 4.00 mm.
CONTRAINDICATIONS
The Esprit™ BTK Everolimus Eluting Resorbable Scaffold System is contraindicated for use in:
• Patients who cannot tolerate, including allergy or hypersensitivity to, procedural anticoagulation or the post-procedural antiplatelet regimen.
• Patients with hypersensitivity or contraindication to everolimus or structurally related compounds or known hypersensitivity to scaffold components poly(L-lactide), poly(D, L-lactide), and platinum.
WARNINGS
• This device is intended for single use only. Do not reuse, reprocess, or re-sterilize. Note the product “Use-by” date on the package. Reuse, reprocessing, or re-sterilization may compromise the structural integrity of the device and / or delivery system and / or lead to device failure, which may result in patient injury, illness, or death. Reuse, reprocessing, or resterilization may also create a risk of contamination of the device and / or cause patient infection or cross-infection, including, but not limited to, the transmission of infectious disease(s) from one patient to another. Contamination of the device and / or delivery system may lead to injury, illness, or death of the patient.
• The Esprit™ BTK System is intended to perform as a system. The scaffold should not be removed for use with other dilatation catheters.
• The Esprit™ BTK System should not be used in conjunction with other non-everolimus drug eluting devices in the same vessel as the Esprit™ BTK Scaffold.
• It is not recommended to use this scaffold to treat lesions located at any joint or other hinge points, such as the knee or ankle. The recommended region for below-the-knee (BTK) treatment with the Esprit™ BTK Scaffold is the infrapopliteal arteries at a location ≥ 10 cm above the proximal margin of the ankle mortise. The Esprit™ BTK Scaffold has not been tested for use outside the recommended implant locations.
• This product should not be used in patients with aneurysms immediately adjacent to the scaffold implantation site.
• Insertion of the Esprit™ BTK System and implantation of the scaffold should be performed only under fluoroscopic observation with radiographic equipment providing high resolution images.
• Quantitative imaging is strongly recommended to accurately measure and confirm appropriate vessel sizing (reference vessel diameter ≥ 2.5 mm). If quantitative imaging determines a vessel size < 2.5 mm, do not implant the Esprit™ BTK Scaffold.
• Adequate lesion preparation prior to scaffold implantation is required to ensure safe delivery of the scaffold across the target lesion. It is not recommended to treat patients having a lesion that prevents complete inflation of an angioplasty balloon.
• Successful pre-dilatation with residual diameter stenosis of < 30% by visual estimation is required for treatment of the target lesion; < 20% by visual estimation is preferred.
• Ensure the scaffold is not post-dilated beyond the allowable expansion limits.
• Use of appropriate anticoagulant and / or antiplatelet therapy per standard of care is recommended for use of this scaffold system.
• This product should not be used in patients who are not likely to comply with the recommended antiplatelet therapy.
• Judicious selection of patients is necessary, since the use of this device carries the associated risk of
scaffold thrombosis, vascular complications, and / or bleeding events.
PRECAUTIONS
• Scaffold placement should not be performed in patients with known allergies to contrast agent that cannot be medically managed.
• It is not recommended to treat patients having a lesion with excessive tortuosity proximal to or within the lesion.
• When multiple scaffolds are required, only combinations of Esprit™ BTK Scaffolds must be used. Any potential interaction with other drugeluting or coated devices has not been evaluated.
• The delivery system is intended for deployment of the scaffold only and should not be used to dilate other locations.
• I mplantation of the scaffold should be performed only by physicians who have received appropriate training.
• A s with all catheter-based procedures, scaffold placement should be performed at facilities where patient can be prepared for necessary intervention and / or surgical removal of the device and vessel repair as per facility protocol.
• P re-dilatation should be performed with an angioplasty balloon. Cutting or scoring balloons can be used per physician discretion, if the lesion appears to be mildly calcified.
• Failure to pre-dilate the vessel may impair nominal / optimal scaffold delivery.
• I mplanting a scaffold may lead to dissection of the vessel distal and / or proximal to the scaffold, requiring additional intervention.
Note: In cases of bailouts, bailout treatment of the target lesion can be done using the Esprit™ BTK Scaffold of the appropriate length. If an appropriate length Esprit™ BTK Scaffold is not available, physicians should use standard of care.
• A n unexpanded scaffold may be retracted into the introducer sheath one time only. An unexpanded scaffold should not be reintroduced into the artery once it has been pulled back into the introducer sheath.
• Post-dilatation is strongly recommended for optimal scaffold apposition. When performed, postdilatation should be performed at high pressure (> 16 atm) with a non-compliant balloon up to 0.5 mm larger than the nominal scaffold diameter.
• Use an appropriately sized non-drug coated balloon to pre-dilate the lesion. When treating a long lesion, scaffold the distal portion of the lesion prior to scaffolding the proximal portion of the lesion.
• Ensure that the scaffolded area covers the entire lesion / dissection site and that no gaps exist between scaffolds.
• The extent of the patient’s exposure to drug and polymer is directly related to the number of scaffolds implanted. The safety of everolimus, polymer, and polymer breakdown products was evaluated in preclinical studies and the biocompatibility assessment of the Esprit™ BTK Scaffold.
• The safety and effectiveness of the Esprit™ BTK Scaffold in patients with prior brachytherapy of the target lesion or the use of brachytherapy for treatedsite restenosis in the Esprit™ BTK Scaffold have not been established. Both vascular brachytherapy and the Esprit™ BTK Scaffold alter arterial modeling. The potential combined effect on arterial remodeling by these two treatments is not known.
• The safety and effectiveness of the Esprit™ BTK System have not been established in clinical trials with the use of either mechanical atherectomy devices (directional atherectomy catheters, rotational atherectomy catheters) or laser atherectomy catheters.
• Formal drug interaction studies have not been performed with the Esprit™ BTK Scaffold because of limited exposure to everolimus eluted from the scaffold.
• Everolimus, the Esprit™ BTK Scaffold’s active pharmaceutical ingredient, is an immunosuppressive agent. Therefore, consideration should be given to patients taking other immunosuppressive agents or who are at risk for immune suppression.
• Oral everolimus use in renal transplant and advanced renal cell carcinoma patients was associated with increased serum cholesterol and triglyceride levels, which in some cases required treatment.
• Non-clinical testing has demonstrated the Esprit™ BTK Scaffold is MR Conditional. A person with the Esprit™ BTK Scaffold may be safely scanned under the following conditions. Failure to follow these conditions may result in injury.
• Static magnetic field strength of 7 Tesla or less
• The Esprit™ BTK Scaffold should not migrate in this MRI environment. MRI at 7 Tesla or less may be performed immediately following the implantation of the Esprit™ BTK Scaffold.
POTENTIAL ADVERSE EVENTS
Potential adverse events include, but are not limited to: Allergic reaction or hypersensitivity to contrast agent, anesthesia, scaffold materials (poly[L-lactide] [PLLA], poly[D, L-lactide] [PDLLA], platinum, or everolimus), and drug reactions to anticoagulation or antiplatelet drugs
• Vascular access complications which may require transfusion or vessel repair, including:
• Catheter site reactions
• Bleeding (ecchymosis, oozing, hematoma, hemorrhage, retroperitoneal hemorrhage)
• Arteriovenous fistula, pseudoaneurysm, aneurysm, dissection, perforation / rupture, and laceration
• Embolism (air, tissue, plaque, thrombotic material, or device)
• Peripheral ischemia
• Target artery complications which may require additional intervention, including:
• Total occlusion or abrupt closure
• Arteriovenous fistula, pseudoaneurysm, aneurysm, dissection, perforation / rupture
• Embolism (air, tissue, plaque, thrombotic material, or device)
• Artery or scaffold thrombosis
• Stenosis or restenosis
• Vasospasm
• Tissue prolapse / plaque shift
• Bleeding (non-access site)
• Additional surgery such as peripheral artery bypass graft surgery or amputation
• Peripheral nerve injury, neuropathy
• Compartment syndrome
• T issue necrosis, gangrene, ulcer and acute limb ischemia
• Reperfusion injury
• New or worsening pain
• I ntervention due to
• Damaged scaffolds
• Partial scaffold deployment
• Scaffold migration / unintentional placement of scaffold
• O ther general surgical risks, including:
• Cardiac arrhythmias (including conduction disorders, atrial and ventricular arrhythmias, and blocks)
• Stroke / cerebrovascular accident (CVA) and transient ischemic attack (TIA)
• Venous thromboembolism (including pulmonary embolism)
• Nausea and vomiting
• Hypotension / hypertension
• Infection – local and systemic (including post-procedural)
• Fever
• Blood cell disorders including heparininduced thrombocytopenia (HIT) and other coagulopathy
• Death
• System organ failures:
• Cardiac Failure
• Cardio-respiratory arrest (including pulmonary edema)
CAUTION: This product is intended for use by or under the direction of a physician. Prior to use, reference the Instructions for Use, inside the product carton (when available) or at manuals.eifu.abbott for more detailed information on Indications, Contraindications, Warnings, Precautions and Adverse Events. This material is intended for use with healthcare professionals only.
Illustrations are artist’s representations only and should not be considered as engineering drawings or photographs. Photo on file at Abbott.
Information contained herein for DISTRIBUTION in the U.S. ONLY.
Abbott
3200 Lakeside Dr., Santa Clara, CA 95054 USA, Tel: 1.800.227.9902
™ Indicates a trademark of the Abbott Group of Companies. www.cardiovascular.abbott
©2024 Abbott. All rights reserved. MAT-2408411 v3.0
• Respiratory failure
• Renal failure
• Shock
The risks described below include the anticipated adverse events referenced in the contraindications, warnings, and precautions sections of the everolimus labels / SmPCs and / or observed at incidences ≥ 10% in clinical trials with oral everolimus for different indications. Refer to the drug SmPCs and labels for more detailed information and less frequent adverse events.
• A bdominal pain
• A nemia
• A ngioedema (increased risk with concomitant angiotensin-converting enzyme [ACE] inhibitor use)
• A rterial thrombotic events
• Bleeding and coagulopathy (including hemolytic uremic syndrome [HUS], thrombotic thrombocytopenic purpura [TTP], and thrombotic microangiopathy; increased risk with concomitant cyclosporine use)
• Constipation
• Cough
• Diabetes mellitus
• Diarrhea
• D yspnea
• Embryo-fetal toxicity
• Erythema
• Erythroderma
• Headache
• Hepatic artery thrombosis (HAT)
• Hepatic disorders (including hepatitis and jaundice)
• Hypersensitivity to everolimus active substance, or to other rapamycin derivates
• Hypertension
• I nfections (bacterial, viral, fungal, or protozoan infections, including infections with opportunistic pathogens). Polyoma virus-associated nephropathy (PVAN), JC virus-associated progressive multiple leukoencephalopathy (PML), fatal infections and sepsis have been reported in patients treated with oral everolimus.
• K idney arterial and venous thrombosis
• Laboratory test alterations (elevations of serum creatinine, proteinuria, hypokalemia, hyperkalemia; hyperglycemia, dyslipidemia including hypercholesterolemia and hypertriglyceridemia; abnormal liver function tests; decreases in hemoglobin, lymphocytes, neutrophils, and platelets)
• Lymphoma and skin cancer
• Male infertility
• Menstrual irregularities
• Nausea
• Nephrotoxicity (in combination with cyclosporine)
• Non-infectious pneumonitis (including interstitial lung disease)
• Oral ulcerations
• Pa in
• Pancreatitis
• Pericardial effusion
• Peripheral edema
• Pleural effusion
• P neumonia
• P yrexia
• R ash
• Renal failure
• Upper respiratory tract infection
• Urinary tract infection
• Venous thromboembolism
• Vomiting
• Wound healing complications (including wound infections and lymphocele)
There may be other potential adverse events that are unforeseen at this time.

By Claire Motyl,
MD
Just over a week ago, I was racing my medical school vascular surgery attending, Dr. Adam Doyle, down a Breckenridge run memorably named “The Devil’s Crotch.” We were celebrating fresh powder, the conclusion of an excellent fellows program, and the opportunity to reconnect with old students (for him), and with familiar faculty and friends (for me). The conference also gave me the opportunity to reflect on the start of my chief years (I am currently a 4thyear integrated resident), and on the lessons I took away from the course.
As other residents and I swapped stories from the trenches, we frequently shared tales about those who came before us—the residents who raised us. One or two stood out, and when I thought about why this was—why we all talked about them with such high regard—I realized that these were residents who not only cared about teaching us but trusted us enough to give us the opportunity to fail. As a medical

“As important as it may be to look upwards for inspiration, so too is it important to look outwards”
By Dylan Lopez
AS THE NEW ADMINISTRATION
headed up by President Donald Trump gets underway, work has begun on his vision for a fundamental transformation of the federal government, including some aspects of the healthcare delivery system.
While the specialty will continue to engage in specific policy debates in the coming months and years, it is important to think about them in the context of this administration’s broader plans for the healthcare system.
Here are a few trends to watch when it comes to the healthcare players and policy goals of this new administration in Washington D.C.
First and foremost, the specialty should
student, these were residents who told me how to pull a drain and didn’t supervise me the second time I did it; as a resident, this was the difference between the residents who showed me how to use the Perclose for the 1 millionth time, and the ones who let me deploy them and accepted the consequences. Succeeding in these training-level-appropriate quests builds confidence for both parties and sets the stage for unlocking the next level. As we enter the era of Entrustable Professional Activities (EPAs), I think that, within the arena of internal mentoring (resident to resident), we should consciously consider entrustable training activities. While turning away and letting someone else do something for the first time is actually hard (a recent discovery), I do think it is as important as ever to ensure that, as chief residents, we are giving junior residents and medical students time and opportunity to execute independently. Although letting a junior discover the “vein of pain” independently
be focused on changes at the Centers for Medicare and Medicaid Services (CMS).
At the time of going to press, the Senate appeared likely to confirm Dr. Mehmet Oz as the administrator of CMS.
During his campaign for Senate in 2022, Oz championed Medicare Advantage and has spent time since then promoting the plan and recommending it to his social media followers.
Given this historical perspective and the Trump administration’s desire to run the government more in the guise of a business, it is likely that Oz will seek policies that allow CMS to operate more like a profit-seeking business rather than a service.
Additional spending reduction targets in this administration’s agenda come from other agencies within the Department of Health and Human Services (HHS), namely the National Institutes of Health (NIH) and the Food and Drug Administration (FDA).
Any reductions in these areas, especially as they relate to research, could have drastic impacts across the healthcare community. The Society for Vascular Surgery (SVS) is monitoring
might result in a little extra work for the supervisor up front, that resident will certainly not forget where it lives the next time (thank you, Victoria, if you’re reading this, and to the general surgery resident who learned this last month: you’re welcome).
As important as it may be to look upwards for inspiration, so too is it important to look outwards. A second personal (and potentially more controversial) takeaway from the Vascular and Endovascular Surgery Society (VESS) Annual Winter Meeting 2025 (Feb. 6–9) in Breckenridge, Colorado, can be summed up as “do as they do, not as they say.” During an industry-sponsored session on leadership in vascular surgery, one of the panelists described how she performed the first transcarotid artery revascularization (TCAR) at her institution, only to have this practice suspended by the division chiefs of two other departments. Subsequently, a patient presented who was anatomically best suited for a TCAR; those chiefs asked her to intervene, and TCAR then gained a foothold at this institution. While this person’s advice was “ask first, don’t make the same mistake I did,” my takeaway was the complete opposite. Do the right thing, ride the waves you make, and, ultimately, something good might come of it.
Both Dr. Doyle and I are former ski racers, so the concept of tolerance of a certain level of risk is familiar to us, which explains how we ended up on the “Devil’s Crotch.” But whether the memorable event is a ski run, performing an entrustable training activity for the first time, or making waves performing an intervention at a new institution (and asking for forgiveness, not permission), making it memorable is well worth the effort.
“We anticipate a high level of continued judicial review for additional forthcoming executive orders, as well as DOGErelated activities”
these developments closely and engaging with other health-related organizations to ensure a collaborative approach for interfacing with administration officials.
This maximalist strategy of taking a sledgehammer to agencies’ spending raises the topic of Elon Musk and his so-called Department of Government Efficiency (DOGE).
Musk’s quasi-governmental department is attempting to usurp Congress’s power of the purse and adds an additional layer of complexity in the realm of budget negotiations, especially for the remainder of this year.
We anticipate a high level of continued
judicial review for additional forthcoming executive orders, as well as DOGErelated activities.
While these unprecedented actions can be dispiriting for us as advocates in the vascular health space, it is important to take on policy fights one at a time and tailor our methods to reflect this new normal.
Some battles will require us to reach out to Congress; some will require us to build public support to pressure the executive branch; and some will require us to do both. This nimble, multi-pronged approach will increase our chances of success on issues that matter to you and your patients.
The SVS is ready to empower our doctors on all of these fronts. We will continue to work with you and advocate in Congress on issues such as Medicare reimbursement, while also working with you on the public affairs side to build support for our practice in the realm of debates around issues like public health spending.
DYLAN LOPEZ is the SVS advocacy and public affairs manager.
CONTINUED FROM PAGE 9
By Geetha Jeyabalan, MD
Vascular surgeons in community practices have always made essential contributions to advancing vascular care, often with limited resources. Balancing busy clinical practices with research pursuits presents significant obstacles, but also opens opportunities for professional growth, improved patient care and broader institutional success. Surgeons in academia face similar challenges to those in a community setting, with resources becoming scarcer throughout the medical ecosystem. Despite a lack of dedicated resources, surgeons in community practice can successfully incorporate research and other academic pursuits into clinical practice. Community practice surgeons may or may not have residents or other trainees to contribute to research projects, and generally face a lack of
associated resources, such as clinical trial coordinators or research statisticians.
Furthermore, many community or private practices are primarily focused on delivering high-quality clinical care and may not align with the academic interests of individual clinicians. This misalignment can make it difficult to engage colleagues in research efforts. Additionally, many practices offer no institutional or financial incentives for pursuing academic work. Finally, the cost to access and maintain participation in national databases related to research, such as the Vascular Quality Initiative (VQI) and National Surgical Quality Improvement Program (NSQIP), are significant barriers. Dedicated nursing support is also necessary.

Collaboration models can be a path to successful research opportunities. Most practices share mutual patients with neighboring or regional health systems or larger academic centers. Creating data-sharing agreements
have become less cumbersome over time and can be a valuable way to create larger sample sizes for research questions. Leveraging available data, rather than national databases, can be a less costly alternative. These data can come from billing databases, vascular labs and existing electronic health records. Larger electronic medical record (EMR) systems have a trove of embedded information, including scoring systems, demographic data, social determinants of health and granular cost data. These are readily available and do not require any additional cost. Of course, institutional review board (IRB) approval is required to utilize some of these data for research. Utilizing external IRBs are options for
“In a time of shrinking institutional budgets, we all must be more creative in convincing hospital and/or practice leadership of the utility and value of engaging in research”
those in private/community practice. Clinical trial work does require research coordinator(s), which can be a barrier to entry for smaller community vascular surgery practices. However, realize that vascular surgery is a relatively closeknit professional world and colleagues who you may have trained with can be valuable sources of collaboration.
In a time of shrinking institutional budgets, we all must be more creative in convincing hospital and/or practice leadership of the utility and value of engaging in research. Sources of funding for these projects can include professional societies and industry, in addition to local hospital endowments. One such example is the SVS Section on Ambulatory Vascular Care (SAVC), which offers research seed grants for community practice vascular surgeons to study outcomes in the outpatient vascular care setting. Demonstrating that having your practice engaged in research and participating in national professional organizations leads to increased referrals, programmatic growth, and institutional/ practice visibility, which can convince partners to stay engaged.


By Jocelyn Hudson
ADDRESSING THE AUDIENCE AT THE 28TH European Vascular Course (EVC 2025) in Maastricht, The Netherlands (March 9–11), Ulka Sachdev-Ost, MD, from the University of Pittsburgh Medical Center (UPMC) in Pittsburgh, Pennsylvania, set out a method to ensure limited funding is directed to the most pressing venous disease research needs.
“As everybody here in this room knows,” Sachdev-Ost began, “funding for research from a federal level—at least in the U.S. and I’m sure it’s similar in other countries—is actually pretty poor given the impact of venous disease for our patients and for the global population.”
Providing a more specific example, Sachdev-Ost homed in on chronic venous disease, which, the presenter shared, “affects quality of life for millions and millions of patients globally.” She also noted that the disease tends to be progressive and is associated with disability, depression and immobility. “These are things that may not be life- or limb-threatening but certainly can affect how people are living their daily lives,” the presenter highlighted.
Sachdev-Ost also underlined a considerable financial burden associated with managing chronic venous disease. Despite considerable patient and monetary costs, Sachdev-Ost pointed out that there is very limited research focused on chronic venous disease. Citing a PubMed search, the pre-
senter noted that the term “chronic venous disease” yields around 24,000 hits compared to 211,000 for “coronary artery disease” and over 3 million for “cardiovascular disease.”
Against this backdrop, the presenter laid out her argument that venous specialists must “focus on identifying high-yield topics that would benefit from dedicated research dollars.” To do this, she proposed, venous research topics must be prioritized.
Sachdev-Ost highlighted the importance of multidisciplinary, multi-stakeholder projects to de fine research priorities, referring to the British-based James Lind Alliance (JLA) as an example of such an initiative. “A big part of [the JLA] is to include patients,” she said. “You must include stakeholders if you’re going to come up with the appropriate research priorities.”
The presenter also detailed a recent multidisciplinary, research priority-setting effort she was involved in with the American Venous Forum (AVF).
Sachdev-Ost shared that she was chair of the AVF research committee in 2024–2025 and was tasked with materializing an idea from the former chair to come up with research priorities in the management of C2 disease, which she presented at the recent AVF annual meeting (Feb. 16–19) in Atlanta.
recalled, with topics—determined based on multiple discussions with the group—focusing on varicose vein management. “We ranked before and after the talk and found that the etiology of varicose veins and equity were some of our big components.”
Concluding, Sachdev-Ost shared that the next step would be to include patients in the discussion to ensure that all stakeholders are involved in setting research priorities related to venous disease.

A question from Stephen Black, MD, from Guy’s and St Thomas’ NHS Foundation Trust and King’s College London in London, England, during discussion time highlighted further the importance of Sachdev-Ost’s point regarding patient involvement in setting priorities.
“ You must include stakeholders if you’re going to come up with the appropriate research priorities”
ULKA SACHDEV-OST
The aim was to approach research priorities in a “transparent” way, Sachdev-Ost told the EVC audience. “We hypothesized that an open forum of brief presentations, open panel discussions and ranking surveys would identify scientific priorities in C2 disease and provide a foundation to design future research efforts,” she said.
The presenter explained that the forum comprised a 10-person multidisciplinary team from specialties including vascular surgery, interventional radiology, vascular medicine, and phlebology.
“We had a really, really good discussion,” Sachdev-Ost
A call for ‘second-generation steps’ in venous stenting INNOVATION
THE NEED FOR A REVOLUTIONARY second generation of venous stents is among the gaps and unmet needs currently at play in deep venous surgery, the 2025 American Venous Forum (AVF), held from Feb. 16–19 in Atlanta, heard. Erin Murphy, MD, from Atrium Health’s Sanger Heart and Vascular Institute in Charlotte, North Carolina, was talking through the most common complications she deals with in practice as she identified a series of gaps in indications for venous stenting during the AVF’s VENOUS 2025 annual meeting.

Patients report with swelling and lack of improvement, she told the meeting, and “most of the time, if we look at why, it’s because we’re treating physiologic but not pathologic compression.” Though less common at this juncture, Murphy said, stent migration represents the most dangerous of the complications venous specialists confront. Which raised the
potential for technology that might “help us differentiate that this is truly pathologic versus anatomic compression,” she said. There have been advances with the coming of dedicated venous stents, and ebbs and flows with devices entering and leaving the the market, Murphy noted.
But IVC stenting would seem to remain “a big gap,” with the Viafort stent (Gore) for the treatment of symptomatic IVC obstruction with or without combined iliofemoral obstruction, under pivotal trial, “our first real big move in this direction,” she added.
What about “second-generation steps” in venous stenting? Murphy pondered.
“We haven’t seen any second moves, so is there something with drug elution like they do in the arteries that we could take advantage of; is there a game changer in the field? What I’ve seen is that there’s really no push for competition right now.”—Bryan Kay
“In the broader context of prioritizing venous disease against all the other disease states that we fight with,” Black began, “the challenge we face is that the impact of death and limb loss for aortic and arterial disease seems to always outweigh the significant quality-of-life destruction that venous patients have, and it becomes hard to challenge that. How do you go about doing that from a point of view of increasing the potential long-term impact of venous disease versus the other priorities?”
Sachdev-Ost responded: “I think that’s an area in which pulling in maybe more of the patient-centered perspective can be very helpful. For many years, peripheral arterial disease and the impact on the muscle was not really given a lot of attention, but now a lot more interest, I think, is there in how much peripheral arterial disease can decrease mobility and create a whole other host of downstream problems that have enormous impacts on spending dollars, etc., for the healthcare system. So, I think similar types of things can be done with venous disease, and pulling in different stakeholders can really help define those metrics.”
NOVEL THROMBECTOMY SYSTEM FOR VTE USED SUCCESSFULLY IN INITIAL TRANCHE OF FIRST-INHUMAN CASES
SONOVASCULAR HAS ANNOUNCED the successful completion of an initial set of eight deep vein thrombosis (DVT) cases using its SonoThrombectomy system as part of a first-in-human (FIH) study. All cases achieved a complete Marder score reduction as assessed by an independent core laboratory, while significant improvements from baseline in Villalta score, revised Venous Clinical Severity Score (rVCSS) and Numeric Pain Rating Scale scores were observed at 30-day follow-up, the company reported. There were no device-related adverse events, major bleeding or deaths.
The data were recently shared during the 2025 American Venous Forum (AVF) in Atlanta, Georgia (Feb. 16–19) by William
Marston, MD, professor of surgery at the University of North Carolina at Chapel Hill School of Medicine.
“The results obtained thus far in SonoVascular’s FIH study demonstrate the SonoThrombectomy system has the potential to become a disruptive technology that would effectively overcome the shortcomings of available therapies for the treatment of DVT,” he said. “In the initial cases, the SonoThrombectomy system has demonstrated its ability to eliminate intravenous clot in a single treatment session with no blood loss and with preservation of venous valves. The system is not limited by the presence of previously implanted filters or stents and is highly steerable for treatment of specific areas of residual thrombus.”
The SonoThrombectomy system delivers ultrasound energy and microbubbles directly to clots through the Resonator catheter, inducing microbubble-mediated cavitation, which mechanically breaks down clots, according to SonoVascular. Additionally, a low dose of tissue plasminogen activator (tPA) is infused in combination with the microbubbles. Bryan Kay

The first and only human-derived bioengineered vessel for vascular trauma repair. 1
Repopulates with the patient’s cells1-3 Low susceptibility to infection4
No immune response observed1-3,5
Off-the-shelf, ready to use1,3
Low amputation results1
SEE FULL IMPORTANT SAFETY INFORMATION at https://bit.ly/ATEV_ISI
INDICATION
SYMVESS is an acellular tissue engineered vessel indicated for use in adults as a vascular conduit for extremity arterial injury when urgent revascularization is needed to avoid imminent limb loss, and autologous vein graft is not feasible.
BOXED WARNING: GRAFT FAILURE
Loss of SYMVESS integrity due to mid-graft rupture or anastomotic failure can result in life threatening hemorrhage.
DO NOT use SYMVESS in patients who have a medical condition that would preclude long-term antiplatelet therapy after acute injury resolution. Warnings and Precautions: Vascular Graft Rupture, Anastomotic Failure, and Thrombosis have occurred in patients treated with SYMVESS. SYMVESS is manufactured using cells and reagents that may transmit infectious diseases or agents; none have been reported during clinical testing. Adverse Reactions: most common (≥3%): thrombosis, fever, pain, anastomotic stenosis, rupture or anastomotic failure, and infection. SEE FULL PRESCRIBING INFORMATION, INCLUDING BOXED WARNING at https://bit.ly/4dl5tuL
REFERENCES: 1. Symvess U.S. Prescribing Information. Durham, NC. Humacyte Global, Inc. 2. Kirkton RD, et al. Bioengineered human acellular vessels recellularize and evolve into living blood vessels after human implantation. Sci Transl Med. 2019;11(485):eaau6934. 3. Dahl S, et al. Readily available tissue-engineered vascular grafts. Sci Transl Med. 2011 Feb 2;3(68):68ra9. 4. Wang J, et al. Biological mechanisms of infection resistance in tissue engineered blood vessels compared to synthetic expanded polytetrafluoroethylene grafts. JVS Vasc Sci. 2023;4:100120.
Trademarks are owned by Humacyte Global, Inc. © 2025 Humacyte Global, Inc. All Rights Reserved. US-SYM-000196

Scan to View FULL PRESCRIBING INFORMATION
J
anet Powell, MD, the clinical trial investigator who played a pivotal role in several landmark abdominal aortic aneurysm (AAA) studies, died in early March at the age of 79. At the time of her death, Powell was professor of vascular biology and medicine at Imperial College London, England.
Powell was born in Oxford on Aug 1, 1945. After obtaining a BSc in chemistry from the University of Oxford (1968) and a PhD in biophysics in London (1972), Powell moved to the U.S. to study medicine at the University of Miami School of Medicine, graduating in 1981. She then returned to the United Kingdom to complete clinical training in pathology, specializing in cardiovascular risk.
central focus of her work: the patient. “Anything that improves outcomes for patients,” she responded, “including all the randomized trials of abdominal aortic aneurysm management, as well as an early piece of pathology research which showed the importance of inflammation in the developing aneurysm, a theme still being investigated by vascular biologists and evaluated in randomized trials.”
Powell was the chief investigator of the IMPROVE randomized controlled trial, which compared open repair with an endovascular strategy for ruptured AAA. Initial trial results were published in the British Medical Journal (BMJ) in 2014, with one-year results presented at the 2015 Charing Cross (CX) Symposium and published in the European Heart Journal the same year.
“We think that the results of this trial support the increasing use of endovascular repair and that it should always be available, so there’s equity of access to care for patients,” she told Vascular News in an interview on the oneyear results.

Initially interested in the pathophysiology of elastic tissues, Powell said in a 2015 profile interview that her research interests turned to the aorta, specifically through her work with Roger Greenhalgh, with whom she collaborated over many decades.
As part of the Imperial College Vascular Surgery Research Group, Powell was involved in numerous clinical trials in AAA management, including the UK Small Aneurysm Trial, EVAR1, EVAR-2 and IMPROVE.
When asked in a 2015 Vascular News profile interview which piece of research she was most proud of, Powell highlighted a
Powell was actively involved in vascular disease research until her passing. Alongside Imperial College London colleagues Colin Bicknell and Anna Pouncey, she was co-chief investigator of the ongoing WARRIORS trial—her last research project—which aims to examine early endovascular aneurysm repair (EVAR) in women.
“The disadvantage of women with AAA can no longer be ignored, and we hope that you will support us, in what will hopefully be a major step towards readdressing the imbalance in AAA outcomes for women and men,” she urged Vascular News readers in an interview on the trial in 2022.
Powell has been recognized by several societies for her contributions to the vascular field. In 2012, she received a Lifetime Achievement Award from the Vascular Society of Great Britain and Ireland (VSGBI), while the European Society for Vascular Surgery (ESVS) hosts a named lecture at its annual meeting to honor Powell’s advocacy of evidencebased medicine.
Powell is survived by her son Duncan (46) and daughter Tamsin (48), as well as five grandchildren.—Jocelyn Hudson
By Kristin Spencer
THE SOCIETY FOR VASCULAR Surgery (SVS) has launched registration for the sixth cohort of its Leadership Development Program (LDP) on. The curriculum is drawn from the highest quality evidenced-based model on leadership, the book The Leadership Challenge, written by James M. Kouzes and Barry Z. Posner, with an intense focus on applying this knowledge to the real-life challenges vascular surgeons face in the field.
The aim is for the participants to reach their full potential as leaders and make a positive impact in the specialty, in their workplace and community, and in other areas of importance in their lives.
After five years, the program is changing its formatting to better fit the needs of vascular surgery leaders. The program

the program.”
After the kick-off at VAM 2025, the program will consist of webinars, short
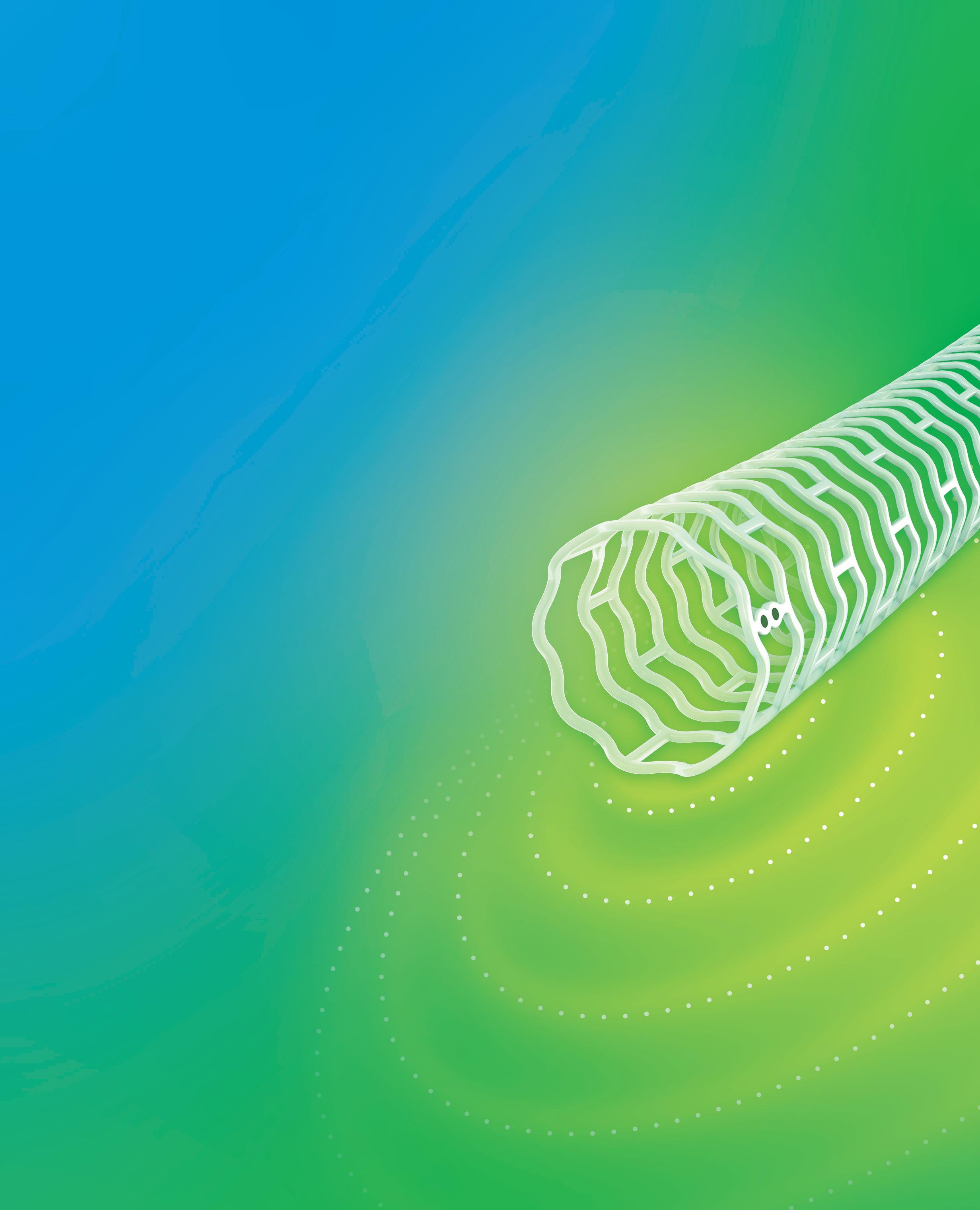
THE SIX-MONTH RESULTS FROM the randomized arm of the Wrapsody arteriovenous access efficacy (WAVE) trial were scheduled for publication in the April issue of Kidney International, ahead of the presentation of 12-month results at the Society of Interventional Radiology’s 50th annual scientific meeting (March 29–April 2) in Nashville, Tennessee.
The creation of an arteriovenous fistula (AVF) to achieve long-term access to blood vessels is required for patients undergoing hemodialysis. However, narrowing of blood vessels in and around the AVF can interfere with hemodialysis delivery, resulting in potentially life-threatening consequences.
The Wrapsody cell-impermeable endoprosthesis (CIE) is designed to help clinicians restore vascular access in patients on hemodialysis who experience stenosis in their venous outflow circuit. The WAVE trial is a multicenter, international, investigational device exemption (IDE) trial designed to evaluate the Wrapsody CIE’s safety and efficacy over two years. In the randomized arm of the trial, 245 patients on hemodialysis who experienced stenosis in the venous outflow of their AVF were treated with the Wrapsody
70.1% vs
on-demand videos, and mentoring calls, concluding with an in-person workshop and graduation ceremony in October. Participants will identify a leadership challenge, working through the process using the skills and tactics they will be learning about from leaders in the field.
“The Leadership Development Program presents its participants with the unique opportunity to learn from people who were once in their shoes,” said Garcia-Toca.
“I believe each participant walks away with tangible tactics to move past barriers they experience in their everyday practice, making them a more effective leader, not only at work, but in their personal life as well.”
Past LDP participants are currently invited to apply for a Mastery Grant to receive up to $3,000 to help them
Visit vascular.org/Leadership for more information.
41.6%
CIE (n=122) or standard percutaneous transluminal angioplasty (PTA, n=123).
Initial results at six months demonstrated that the target lesion primary patency was significantly higher for the Wrapsody CIE vs. PTA (89.8% vs. 62.8%; p<0.0001).
Similarly, the access circuit primary patency was significantly higher for the Wrapsody CIE vs. PTA (72.6% vs. 57.9%; p=0.015). No significant difference in the safety outcome was observed between treatments.
At 12 months, the Wrapsody CIE remained significantly higher than PTA for both target lesion primary patency (70.1% vs. 41.6%; p<0.0001) and access circuit primary patency (58.1% vs. 34.4%; p=0.0003).
The Wrapsody CIE received premarket approval from the Food and Drug Administration (FDA) in December 2024.—Urmila Kerslake

Caution: Federal (USA)
INDICATIONS FOR USE


to Directions for Use and/or User Manual provided with the product for complete Instructions, Warnings, Precautions, Possible Adverse Effects and Contraindications prior


By Marlen Gomez
The Vascular Research Initiatives Conference (VRIC) will spotlight the crucial role of mentorship in advancing the fields of vascular surgery and research during its upcoming event on April 22. This year’s conference will run concurrently with the American Heart Association’s Vascular Discovery 2025 Scientific Sessions, themed “From Genes to Medicine,” which will explore the pathway from genetic discovery to clinical application.
This year’s conference theme is “Deploying Multiomics to Reveal New Therapeutic Targets in Vascular Biology.” Conference organizers have noted that contributions on topics like chronic limb-threatening ischemia (CLTI) and aneurysms will be a significant part of the discussions, emphasizing the importance of fundamental biology within cellular environments.
Kathryn L. Howe, MD, a surgeon-scientist at the University Health Network in Toronto, Canada, and chair of the SVS Basic and Translational Research Committee, has been an enthusiastic attendee of the VRIC since 2016. Her journey to the conference began with a mentor’s recommendation, underlining the event’s significance for emerging vascular surgeon-scientists.
Reflecting on her inaugural experience, Howe described it as “mind-blowing” and emphasized the importance of early participation in the event to foster community connections. “I can’t say enough about the importance of going early and then being part of that community feeling, building upon it every year that you go,” Howe said.
This year, the VRIC promotes robust discussions on cuttingedge basic science and translational research topics while ensuring that conversations remain rooted in current evidence-
based practices and science. Mentorship and collaboration are at the forefront of this initiative, exemplified through Howe’s partnership with her mentee, Sneha Raju, MD, a third-year vascular surgery resident at the University of Toronto. Raju recently completed her PhD research on endothelial cell communication in atherosclerosis and expressed her excitement about engaging with various vascular pathologies at the conference. “It’s inspiring to see vascular surgeon-scientists not only surgically manage vascular pathologies but also tackle the biological challenges behind these diseases to enhance patient diagnostics and treatments,” Raju said.
Having first attended the conference during the COVID-19 pandemic, Raju noted the uplifting atmosphere that emerges when leaders in the field come together to address vascular disease. “[VRIC] is a great place to build collaborations and advance scientific questions by recruiting insights from members with varied experiences,” Raju said.
With its emphasis on exchanging knowledge in basic and translational vascular science, VRIC encourages thoughtful dialogue to explore solutions to vascular patients’ pressing issues. Howe emphasized the crucial need for these discussions in today’s research climate: “When it comes to making sure that our science is seen and heard and valued, and therefore we have a platform to continue to advocate for additional funding, this is crucial.”
“I can’t say enough about the importance of going early and then being part of that community feeling, building upon it every year that you go”
KATHRYN L. HOWE

THE SOCIETY FOR VASCULAR Surgery (SVS) Foundation, in partnership with the SVS Young Surgeons Section, has launched the VOYAGE Scholarship Program. This initiative will provide $1,000 scholarships to assist early-career vascular surgeons during their formative years in the profession.
The recipients can use the funds to continue medical education courses, professional development events, and other relevant educational pursuits that will help them build their professional networks and connect with the vascular surgery community.
Applications were due by Tuesday, April 1. Eligible courses for funding include a range of educational events, such as VRIC, the Vascular Annual Meeting (VAM) and the SVS’ Complex Peripheral Vascular Intervention Skills Course, which is set to take place in Rosemont, Illinois (Sept. 20–21).
To qualify, applicants must be active members of the SVS Young Surgeons Section. Vascular trainees, residents and medical students are not eligible to apply. Each applicant is eligible to receive one VOYAGE Scholarship per calendar year.
Learn more about the scholarhsip program at vascular.org/VOYAGE



How likely are your surgical patients to have disruptive bleeding?
Compiled
THE SVS HAS DEVELOPED A COMPREHENSIVE member toolkit to equip healthcare professionals, particularly vascular surgeons, with essential resources through its “Highway to Health: Fast Track Your Vessel Health” campaign.
With millions of Americans at risk for developing vascular conditions, awareness about these potentially life-threatening issues remains alarmingly low. The Highway to Health campaign seeks to address this gap by encouraging individuals to engage in timely evaluations and treatments.
The Member Toolkit includes materials such as a fact sheet, frequently asked questions, a template press release, social media content and newsletter/ web copy for individual use.

The toolkit features training tips, a C-suite letter and a graphics/media library, all designed for use across personal social media channels, and at both internal and external speaking engagements.
The SVS emphasizes the importance of proactive health discussions, urging individuals to talk to their healthcare providers about potential vascular issues and to consider referrals to vascular surgeons.
The success of the Highway to Health initiative depends significantly on the engagement and advocacy of medical professionals who recognize the vital importance of vascular health, according to the SVS.
For more information and to access the toolkit, visit vascular.org/H2Hresources
by
Marlén Gomez
THE SVS HOSTED ITS LATEST webinar entitled “Harnessing AI in Vascular Surgery: Leading the Next Frontier” on March 27.
This event aimed to elevate awareness of artificial intelligence (AI) within the vascular surgery community, presenting not only the latest advancements in AI technologies but also encouraging healthcare professionals to engage in the ever-evolving landscape of AI-driven research and practice.
The webinar sought to enhance participants’ knowledge and expertise, ultimately fostering innovation in patient care and research.
Attendees took part in in-depth discussions on several critical topics, including emerging AI-powered tech-
nologies and research developments specific to vascular surgery, key terminology related to AI-based medical research, the challenges faced in implementing AI projects, and practical strategies to overcome these barriers.
Additionally, the session saw valuable insights on the regulatory landscape and ethical considerations surrounding the use of AI tools in medical practice and research.
Moderated by Shivprasad Nikam, MD, a vascular surgeon at Geisinger Wyoming Valley Medical Center in Pennsylvania, the webinar featured a distinguished panel of speakers, including Andrew A. Gonzalez, MD, Uwe Fischer, MD, Sharon C. Kiang, MD, William J. Yoon, MD, and Paula K. Shireman, MD.
Registration for the 2025 Vascular Annual Meeting (VAM 2025) is now open. This year’s meeting will take place in New Orleans, Louisiana, June 4–7. VAM 2025 will consist of three full days of education covering the latest updates in the vascular surgery field and two full days of a packed exhibit hall featuring the newest technology in the specialty and more. SVS members will see an additional discount on their rates when compared to those of nonmembers. Any nonmember wanting to take advantage of the member discount can apply for SVS membership by May 1 to receive the refunded difference, pending application approval. Housing for VAM 2025 opened March 5.
To register and get more information, visit vascular.org/VAM
Philips issues Class I recall for Tack endovascular system
PHILIPS ANNOUNCED THAT IT WILL NO longer sell its Tack endovascular system in the U.S. following a Class I recall issued by the Food and Drug Administration (FDA).
A Class I recall is the FDA’s most serious classification, which denotes that the continued use of the affected product could result in severe injury or death.
The FDA’s decision follows reports that the Tack endovascular system—designed to treat arterial dissections—has posed challenges for users, sometimes necessitating additional interventions to retrieve or remove the implant. The self-expanding device is composed of nitinol, a nickel-titanium alloy.
The FDA warned that continued use of the device could lead to significant health risks. Short-term complications include partial or complete blockage of blood flow, perforations in the artery’s inner lining or full-thickness arterial tears. Long-term consequences may involve pain, tissue loss, re-narrowing of the vessel and, in more severe cases, bypass surgery, amputation or death.
Philips has reported 20 injuries linked to the Tack system but has not received any reports of fatalities.
The Tack system was initially approved by the FDA in April 2020. It was developed by Intact Vascular, a cardiovascular company acquired by Philips for $275 million later that year.

Inari Medical, now part of Stryker, launches Artix thrombectomy system
INARI MEDICAL, NOW PART OF STRYKER, RECENTLY announced the launch of its Artix thrombectomy system. Purposebuilt for the needs of the peripheral arterial system, Artix is a combined aspiration plus mechanical thrombectomy solution.
Stryker notes that the Artix system builds on Inari’s venous thrombectomy devices and is its first entry into the arterial space.
Jonathan Bowman, MD, section chief of vascular surgery at Norwalk Hospital in Norwalk, Connecticut, performed the first commercial case with Artix on Oct. 19, 2024.
THE SVS FOUNDATION HAS various initiatives in place to celebrate Women’s History Month, including member profiles and patient-focused facts. New this year is fundraising for the launch of a new Vascular Care for the Underserved (VC4U) award, focused on women’s vascular health research.
For the first time, the Foundation and the SVS Women’s Section will collaborate to raise $30,000 from March 1–31 in order to fund the VC4U project grants.
“The VC4U project grants aim to address significant disparities in vascular surgery care across the U.S., and the funds raised for the grant will support projects that advance women’s health,” said Audra Duncan, MD, chair of the SVS Women’s Section Steering Committee.
A $20,000 grant will be awarded to an SVS or Society for Vascular Nursing (SVN) member for an innovative, community-based initiative that addresses the challenges faced by underserved populations affected by peripheral artery disease (PAD), emphasizing improving diagnosis, treatment and patient education.
Applications for the award closed on March 3.
To learn more, visit give.vascular.org/WHM25
Shockwave Medical announces US launch of intravascular lithotripsy catheter
SHOCKWAVE MEDICAL ANNOUNCED the U.S. launch of its Shockwave Javelin peripheral intravascular lithotripsy (IVL) catheter, a platform designed to modify calcium and cross narrowed vessels in patients with peripheral artery disease (PAD).
The platform is designed to modify calcium and cross calcified occlusive disease or extremely narrowed lesions where a wire will cross but devices might not.
Shockwave Javelin has a working length of 150cm and features a single distal emitter that creates up to 120 shockwave pulses. Each shockwave pulse creates a spherical energy field that extends beyond the tip of the catheter. This novel design delivers lithotripsy closer to calcium than the balloonbased platform, the company reports.
Despite the challenging nature of the calcified lesions studied, the clinical outcomes from the FORWARD PAD investigational device exemption (IDE) trial demonstrated that Shockwave Javelin has a similar safety and effectiveness profile to balloon-based Shockwave IVL catheters, a press release states.
2 0 2 5




A d v a n c i n g W o m e n i n
V a s c u l a r C a r e
F r i d a y - S a t u r d a y
M a y 2 - 3 , 2 0 2 5
W h e r e ?
M a r r i o t t C h i c a g o O ' H a r e
8



Continuously advancing aortic treatment — as your aortic ally, that’s our commitment. So, when you’re looking for case planning support, want to learn about a new registry or need materials to help educate your patients, we’re here to help you meet the moment.