
5 minute read
Happenings
from May 2021 O&P Almanac
by AOPA
RESEARCH ROUNDUP
Army Scientists Develop Rate-Activated Tethers for Orthoses
U.S. Army researchers have debuted an orthotic device design that features adaptable coupling elements and rate-activated tethers incorporated into elastic materials, comprising the body of orthoses. The tethers are “cable-like devices that are filled with fluid and filaments,” according to an announcement from the DEVCOM Army Research Laboratory, and are made from materials that are both elastic and able to seal fluid inside, such as rubber, silicone, polymer, or latex.
The filaments inside the tethers are made of steel, polymer, glass, or carbon; these filaments may be either free-floating or attached to one or both sides of the tethers.
Orthoses made using the new design provide variable support, depending on the wearer’s speed and movement intensity. Because they can stretch and recover quickly during movement, they provide a unique balance of comfort, performance, and support, according to the research team. Used in an ankle brace, for example, the tethers will support regular daily activities without causing the joint’s weakening, but will limit motion during fast movement to prevent supination of the ankle, according to the researchers.
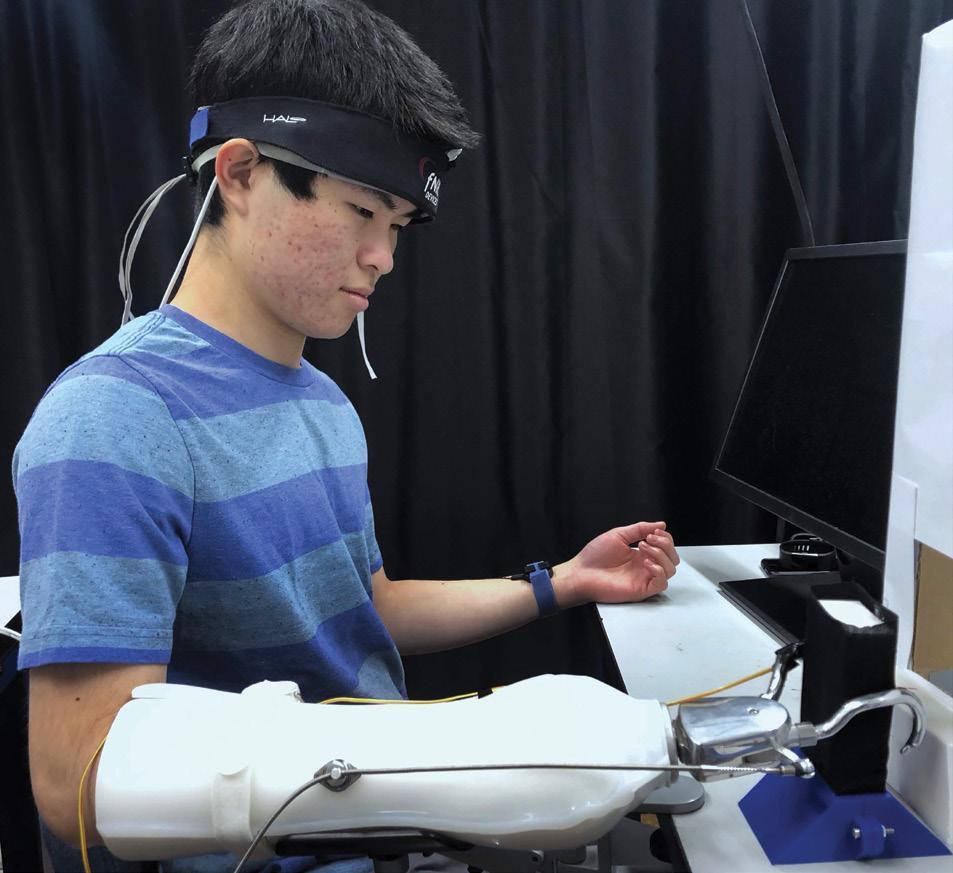
Researchers Study Benefits of Prostheses Integrated With Haptic Sensory Feedback
Focusing on the mental effort of users operating prostheses, a research team from Johns Hopkins University and Drexel University is studying whether adding haptics, or an artificial sense of touch, to upper-limb prostheses reduces the mental effort required to operate the device. “Normally, vision is heavily used to successfully operate a myoelectric prosthesis, and this can cause high mental fatigue,” explained researcher Jeremy D. Brown, PhD, an assistant professor of mechanical engineering at A study participant tests a prosthesis featuring haptic feedback. Johns Hopkins. “Haptic feedback that whose stiffness were difficult to differsubstitutes for vision can reduce this entiate,” according to the researchers. cognitive load, which helps bridge the “This research suggests that future gap between the function of the healthy upper-limb prosthetic technologies limb and that of a prosthetic limb.” need to incorporate haptic feedback in
Brown and his team proposed wear- their design,” said Brown. “In addition, able, wireless functional near-infrared this research provides a framework spectroscopy (fNIRS) neuroimaging for using brain imaging techniques to provide a continuous direct assess- like fNIRS to evaluate the cognitive ment of operator mental effort during load of new prosthetic technologies use of prostheses. Study participants in a variety of natural scenarios and were asked to differentiate objects in environments.” The findings were three distinct ways: using their natural published in April in IEEE Transactions hand; using a traditional myoelectric on Human Machine Systems. prosthesis without sensory feedback; Future projects for Brown’s team and using a myoelectric prosthesis with include investigating how haptic haptic (vibrotactile) feedback of grip feedback and automated grip control force. Results indicated that “discrim- can enable a prosthesis wearer to ination accuracy and mental effort are operate their prosthesis without visual optimal with the natural hand, followed observation. “An example scenario by the prosthesis featuring haptic would be the ability to watch TV while feedback, and then the traditional simultaneously picking up the TV prosthesis, particularly for objects remote out of view,” said Brown.
MEDICAL MATTERS
AHA Proposes Strategies To Decrease PAD Amputation Rates
The American Hospital Association (AHA) has released a policy statement featuring recommendations to improve limb outcomes and drive U.S. amputations rates down 20 percent by the year 2030. Published in March in Circulation, the AHA statement, written by AHA Writing Committee Chair Mark A. Creager, MD, and his team, seeks to lower the number of Americans requiring amputation due to peripheral artery disease (PAD).
Stakeholders, including clinicians, researchers, patients, family members, regulatory agencies, and the healthcare system, should work together to make appropriate changes “to take steps that will reduce the likelihood that someone with peripheral artery disease will progress to the point that they develop critical limb ischemia and need an amputation,” said Creager.
The AHA offers several suggestions for improving public awareness of PAD and increasing use of effective PAD management strategies, such as smoking cessation, use of statins, and foot monitoring/care in patients with diabetes. To facilitate the implementation of these recommendations, AHA proposes “several regulatory/legislative and organizational/institutional policies such as adoption of quality measures for PAD care; affordable prevention, diagnosis, and management; regulation of tobacco products; clinical decision support for PAD care; professional education; and dedicated funding opportunities to support PAD research.” The AHA statement notes that if the recommendations and proposed policies are implemented, “we should be able to achieve the goal of reducing the rate of nontraumatic lower-extremity amputations by 20 percent by 2030.”

FAST FACT
Paralympic Games Will Feature Record Media Coverage
More than 290 athletes across 22 Paralympic sports are expected to represent Team USA in the Tokyo Paralympic Games August 24September 5. NBC Universal will air a record 1,200 hours of Paralympic coverage from the Tokyo Games, including the first NBC primetime broadcasts in history. NBC also will air U.S. Paralympics Trials coverage on June 27.
O&P ATHLETICS
Academy Partners With OPAF To Provide Administrative and Support Services
The American Academy of Orthotists and Prosthetists has announced a partnership with the Orthotic and Prosthetic Activities Foundation (OPAF). The Academy will provide administrative support to help OPAF fulfill its mission of serving those with physical and mobility challenges and raising public awareness of physical disability, limb loss, and limb difference. The partnership follows a July 2020 decision by the OPAF Board to enter a state of dormancy in light of the COVID-19 pandemic, to reduce operating costs and allow the board to focus on restructuring. Academy President Jared Howell, MS, CPO, FAAOP, said the Academy’s mission is “hand in glove” with OPAF’s: “Many in the O&P community were deeply disturbed by the thought of there being no OPAF to serve the O&P patient population,” he said. “The Academy is thrilled to support the OPAF mission as it positively impacts the lives of the patients [that] we as O&P practitioners serve.” The partnership allows OPAF to remain as an independent 501(c)3, with a focus on fundraising and program development, while the Academy will help administer the day-to-day operations of the OPAF financials, marketing, events, and website. “On behalf of the OPAF Board of Directors, we are so excited to announce our partnership and bring our programming back to the communities that we serve,” said Travis Young, CPO, president of OPAF. “Since its inception, OPAF has served as the philanthropic arm of the orthotic and prosthetic community, and we look forward to the expanded relationship with the Academy and the opportunities that it will bring. We are grateful for the support of all of our partners, instructors, and participants over the years and are thrilled for what the future holds.”











