















Bereaved families and communities nationwide came together this week (Sunday March 9) to reflect on and mark the fifth anniversary of the start of the COVID-19 pandemic.
The day was an opportunity to reflect on the sacrifices made, the impact on our daily lives, and pay tribute to the work of health and social care staff, front-

line workers and researchers during what was an unprecedented time.
Hundreds of events took place all over the UK, and spaces for reflection organised by communities remembered and commemorated those who lost their lives during the pandemic.
(CONTINUED ON PAGE 3...)


Editor
On March 9, the UK observed a Day of Reflection, marking the anniversary of the COVID19 outbreak. It was a moment to remember those we lost and to honour the extraordinary efforts of those who worked tirelessly to protect others.
For the adult social care sector, this day holds profound significance.
Care homes and care workers were on the frontlines of the pandemic, operating under unimaginable conditions with limited resources, inadequate PPE, and little support. Their sacrifices must never be forgotten.
The pandemic exposed the fragility of the UK’s social care system like never before. Care homes bore the brunt of the crisis, with residents accounting for a devastating proportion of COVID-related deaths.
The virus spread rapidly in these settings, intensified by close living quarters and the high level of care required for vulnerable residents.
For care workers, the pandemic was a harrowing experience. They worked long hours, often without adequate PPE, to provide care and comfort to residents while putting their own health at risk.
Many staff members slept in care homes on camp beds, isolating themselves from their families to protect residents. The emotional toll was immense, with workers forming deep bonds with residents only to lose them to the virus.
The trauma of the pandemic continues to affect the sector. Staff and residents alike are still grappling with the mental health fallout, including anxiety, grief, and burnout.
The crisis also highlighted systemic issues such as chronic underfunding, workforce shortages, and the lack of integration between health and social care.
In 2022, I attended a seminar where care providers and staff were invited to share their experiences. It was one of the most profound and harrowing events I have ever witnessed. I listened as people fought back tears, struggling to relive
responsibility for any effects, errors or omissions therefrom. All rights reserved, reproduction is forbidden
their experiences.
The lack of PPE and information was a recurring theme, with staff recounting how they improvised with bin bags as aprons and slept in care homes to avoid spreading the virus to their families. These stories have stayed with me, and I often recount them because they serve as a stark reminder of the sacrifices made by those who “walked the walk.”
As Professor Martin Green, Chief Executive of Care England, rightly states in our lead story: “We owe it to them to do more than remember; we must act.” Social care cannot continue to be an afterthought. It must be recognised as fundamental to the health and wellbeing of our nation. Governments must invest, reform, and support care services to ensure that we never again see the devastation experienced during the pandemic.
A new report by Community Integrated Care highlights another pressing issue: the persistent pay gap between social care workers and their NHS counterparts.
The charity is calling on the government to uplift care worker wages, arguing that fair pay is not only affordable but a crucial investment in economic growth and the long-term sustainability of the NHS.
As the sector faces the double whammy of increased National Insurance Contributions and the National Minimum Wage, it is more crucial than ever for the government to step in and underwrite these costs.
The sector has been lobbying for more funding to pay staff fairly, but as the ProvidersUnite protest on February 25 confirmed, it remains critically underfunded. We need an additional £8.4 billion to meet future demand, improve access to care, and cover the full cost of care by the end of the year.
ProvidersUnite own analysis suggests that the real impact of these increases on employers may exceed projections by over £2 billion. With just weeks until the changes take effect, the government must act swiftly to clear a mess of its own making.
The Day of Reflection is not just about remembering the past; it is about shaping the future. Let us honour the sacrifices of the care sector by demanding the investment and reform it so desperately needs. This is the only fitting way to ensure that the lessons of the pandemic are never forgotten and that those who gave everything to protect others receive the recognition and support they deserve.
I would encourage our readers to sign up for our bi-weekly digital newsletter at www.thecareruk.com and follow us on social media for all the latest news.
I can always be contacted at editor@thecareruk.com


Speaking as the day approached, Culture Secretary, Lisa Nandy said: “The pandemic impacted us all in different ways, with many sadly losing loved ones and others making great sacrifices in their lives. This COVID-19 Day of Reflection will allow people the space and time to reflect, and I would encourage everyone to take part in a way that feels right for them.”
Chair of the UK Commission on Covid Commemoration, Baroness Morgan of Cotes said:
“It is right that, as a country, we take the time to remember the COVID-19 pandemic, to reflect on what happened, remember those whose lives were impacted in so many ways and honour those who tragically lost their lives. Today is an opportunity for communities to come together to reflect and commemorate their loved ones.”
DEEP GRIEF
Prime Minister Sir Keir Starmer said: "As we mark five years since the outbreak of the Covid-19 pandemic, I know for many there is deep grief and loss that may never be relieved."

In London bereaved relatives, led by a Highland piper, joined well-wishers to walk beside the National Covid Memorial Wall.
They passed 3,000 photographs of the faces of some of those who died, which represents just over 1% of the total death toll from Covid in the UK, organisers said.
Between March 2020 and July 2022, an estimated 180,000 people died after contracting COVID in England and Wales, according to figures published by The King's Fund thinktank..
The day was particularly poignant as the nation paused to remember the lives lost , including so many people who relied on care – whether in care homes, home care, supported living, or other social care settings – and those who dedicated their lives to caring for others.
UNSUNG HEROES
Care homes became the epicentre of the crisis, with residents accounting for a significant proportion of COVID-related deaths, as the virus spread rapidly in these settings, exacerbated by the close living quarters and the high level of care required for vulnerable residents.
Care workers, so often described as the unsung heroes of the pandemic, faced immense challenges, working long hours, often without adequate PPE, to provide care and comfort to residents while putting their own health at risk.
Many care homes were forced to operate in isolation, with staff cut off from their families and residents unable to see loved ones for months on end.
SACRIFICES AND STRUGGLES
The lack of PPE was one of the most critical issues during the early stages of the pandemic. Care homes
struggled to secure essential supplies, leaving staff and residents exposed to the virus. Despite these challenges, care workers showed remarkable resilience and dedication, continuing to provide high-quality care under the most difficult circumstances.
The emotional toll on both staff and residents was profound. Families were unable to visit their loved ones, leading to feelings of isolation and loneliness among residents. Care workers, many of whom formed close bonds with residents, faced the heartbreak of losing those they cared for while also dealing with their own fears and anxieties.
The day was a solemn reminder of the pain, grief, and sacrifices endured by families, care workers, and communities across the country.
For those working in the care sector, the pandemic was not just a crisis, it was an unrelenting battle. Care workers stood on the frontline, often without the protection, recognition, or support they deserved.
COURAGE AND COMPASSION
Many risked their own health and lives to ensure that those they cared for remained safe. Others endured the heartbreak of being the only ones by the bedside when family members couldn’t be there, offering comfort in the final moments.
The courage and compassion shown by the social care workforce during that time must never be forgotten.
Professor Martin Green OBE, Chief Executive of Care England, said: “Remembrance alone is not enough.
Successive governments must acknowledge, understand, and respect social care as the pillar of our nation that it truly is. The pandemic exposed the deep-rooted vulnerabilities of our care system; underfunded, undervalued, and too often overlooked in national decision-making. It is unthinkable that, five years on, many of the same challenges remain.”
“We cannot allow history to repeat itself. The pressures and pain witnessed during the pandemic must serve as a turning point, not a forgotten chapter. The care sector must be strengthened with proper the right funding and meaningful reform that ensures it is never again left exposed in a time of crisis. Only by making social care a true national priority can we honour the sacrifices made and protect those who rely on care today and in the future.”
INVEST, REFORM, SUPPORT
“The Day of Reflection is a moment of collective remembrance; of lives lost, of sacrifices made, and of the extraordinary resilience shown by the care sector. Too many people paid the ultimate price, and too many care workers carried an unbearable weight on their shoulders. We owe it to them to do more than remember; we must act.”
“Social care cannot continue to be an afterthought. It must be recognised as fundamental to the health and wellbeing of our nation. Governments must invest, reform, and support care services so that never again do we see the devastation experienced during the pandemic. This is the only fitting way to honour those we have lost and those who gave everything to protect others.”


By Fozia Iqbal, Senior Business Immigration Solicitor at law firm Harper James (www.harperjames.co.uk)
Reports of exploitation, including unfair wages and poor working conditions, have drawn increased government attention to the treatment of overseas workers in the care sector.
With a critical staff shortage, many businesses depend on international recruitment to fill vacancies, adding to concerns about worker welfare.
The Home Office has intensified its crackdown on non-compliant employers, with severe consequences for those who fail to meet legal and ethical obligations. Compliance with immigration and employment laws is no longer just an administrative requirement but an essential strategy for protecting business operations, reputations, and, most importantly, the wellbeing of workers.
To hire overseas care workers legally, care business owners must navigate a complex regulatory framework. They must obtain a sponsor licence issued by the Home Office, through which they can sponsor overseas health and care workers for a Skilled Worker visa, which is the primary route for recruitment, but this visa comes with strict sponsorship obligations. Employers must make sure that all hired workers have valid visas and are working in compliance with their visa restrictions and their sponsorship. Employers would need to implement correct right to work check policies and ensure they are meeting minimum salary requirements, can provide work that meets the contractual hours of work offered, and the employees are undertaking duties which fall strictly within the role for which they have been sponsored.
Additionally, all employers must ensure that their employees’ employment conditions align with legal requirements, for instance, providing safe working environments, adequate training, and following proper recruitment procedures. Fundamentally, overseas workers must receive their full rights and entitlements such as fair pay, breaks and leave, with no discrimination. Any deviation from these standards can place a business at significant risk.
The UK government is taking decisive action against care providers who fail to protect overseas staff. Increased inspections and audits are being carried out, with penalties ranging from significant fines to licence revocations and outright business closures. Employers found guilty of exploitation or modern slavery
offences face criminal prosecution, and businesses that lose their sponsor licences will lose their sponsored workers and be unable to hire overseas staff in the future.
In addition to heightened inspections, the Home Office is working closely with other regulatory bodies to share intelligence and data on non-compliant practices. This collaboration enhances the government’s ability to detect irregularities and enforce penalties swiftly, ensuring that any rogue employer faces immediate consequences. Such coordinated efforts not only deter potential offenders but also reassure compliant businesses that the sector is being rigorously monitored.
This increased enforcement underscores the necessity for care home owners to maintain high standards of employment practice. Failing to comply with legal obligations does not only jeopardise individual businesses but also tarnishes the reputation of the sector as a whole.
Beyond legal obligations, treating overseas workers ethically is a crucial element of running a successful business. Providing fair pay, ensuring reasonable working hours, and fostering a safe and supportive environment contribute to higher job satisfaction and better staff retention. In an industry where continuity of care is essential, a stable and motivated workforce is invaluable.
Ethical employment also enhances a business’s reputation. Care businesses known for fair treatment of staff find it easier to attract both workers and clients. By proactively adopting fair employment practices, organisations safeguard their operations from legal risks and cultivate a more committed and engaged workforce.
TAKING
To protect your business and your staff, you should regularly review your employment practices. By conducting internal audits, training staff on compliance obligations, and seeking professional legal guidance, you can help ensure ongoing adherence to the law. Being proactive in compliance not only mitigates legal and financial risks but also encourages a positive workplace culture.
Looking to the future, it is vital for care providers to establish a culture of continuous improvement in compliance. Regular training sessions, clear communication of legal updates, and robust internal controls can help your business stay ahead of regulatory changes. Embracing technology to monitor recruitment and employment processes further supports transparency and accountability, ultimately benefiting both your staff and the reputation of your business.
As the government continues its strict stance on non-compliance, you should take immediate action to ensure your recruitment and employment processes align with legal and ethical standards. Now is the time to assess your business’s current practices, implement necessary improvements, and secure the future of your business by treating overseas workers with the fairness and dignity they deserve.
When Pam Pryor moved into a care home, she was delighted that the team not only supported her to continue her passion for painting, but also organised art workshops so she could share her hobby with others.
Pam, who moved to Sanctuary Care’s Chyvarhas Residential and Nursing Home in Callington last year, has held a stall to sell her paintings at the home’s winter fete and is proud to see several of them displayed around the care home.
“I feel very happy to be able to continue my hobby here and to get the support of the staff,” Pam explains.
“It is very important that we are encouraged to continue our hobbies or activities we used to enjoy, and the team really do support us. We have art workshops, which not only encourage me to pick up the paint brush, but also other residents who may have never painted before.” Pam, who is 90 years old, loves to paint landscapes and flowers at the home, which provides residential, nursing, dementia and respite care.
“I take a lot of my inspiration from the garden here,” she explains. “I

am very proud that some of my artwork is displayed in the home, it makes me feel so valued.
“Being here is a new community to call home and these activities give me the feeling of purpose.”
Surprisingly, Pam didn’t take up her hobby until she was 60.
“I love the freedom of painting,” she explains. “The way it just flows out of you. You start with a blank canvas, and you don't know where it is going to go.”
For Pam, being part of the community at Chyvarhas means so much to her. “We all work together to ensure Chyvarhas is a happy place, away from the troubles in the world. The staff are first class - they are so caring and nothing is too much for them.”
Home Manager, Michael Dickinson-Smith, added: “We are proud to enrich the lives of our residents each and every day, and a big part of that involves us working with them to continue much-loved hobbies, creating a sense of continuity and belonging.”
Former teenage codebreaker turned burlesque dancer, 100year-old Hilda Green had the surprise of her life when she was presented with a Certificate of Contribution by the World Burlesque Academy.
Hilda now lives at Castleford Lodge Care Home in West Yorkshire. Hilda’s story is one worthy of a Hollywood movie – at the age of 15 she worked as a codebreaker at Bletchley Park during World War II, helping to decipher German messages; the collective efforts of the intrepid team there undoubtedly shortened the war by years.
After the war she was attracted to the bright lights of Paris and dazzled audiences as a burlesque dancer, before returning to the UK to embark on a career as a bookkeeper.
Last October Hilda celebrated her 100th birthday with a party at Castleford Lodge, where she has lived for almost three years. Recently World Burlesque Academy representative and gradu-

ate, Wakefield burlesque artist Ozara Sapphire, alongside the CEO of the academy, Sapphira, visited Castleford Lodge to present a Certificate of Contribution to Hilda for her years spent as a burlesque dancer.
The pair put on their finest feathers and treated the residents of Castleford Lodge to a performance that couldn’t help getting people singing and dancing along with them.
Ozara said:”’Castleford Lodge was a welcoming and homely space, it was a delight to sing for the residents and make them smile with our feathers!”
Sarah Golden-Hill, Home Manager at Castleford Lodge Care Home, said: “Hilda was overjoyed to be recognised by World Burlesque Academy, she was beaming with pride! We wanted to say a huge thank you to Ozara Sapphire and Sapphira for coming to visit us – our residents and colleagues loved seeing you.”
Searches carried out by care seekers on care directory company Autumna, show that catering, the range of activities, environmental commitments and even pet policies are scrutinised more often than the ratings awarded by the Care Quality Commission (CQC).

“Our analysis of searches on our platform in 2024 confirms that CQC ratings aren’t relevant to those looking for care – they are too out of date and do not provide information on the criteria that matter to families.”
Last year, the most popular care home information sought out was fees, with nearly one in five users (18.2%) checking the fees of care homes that met their search criteria. The next most significant information looked for were rooms, checked out by one in ten care seekers (10.2%), followed by admission criteria (9.2%).
However, only 3.3% looked for more detailed information explaining the rating a care home had been awarded by the CQC.
By contrast, two and half times as many care seekers researched the dining choices (8.8%), while twice as many checked out the environmental commitments of care homes they were considering (7.2%). The choice of activities was also more important to self-funding families, with 5.75% investigating this.
With 3.6% of visitors checking out care homes’ pet policies, even the ability to take a furry or feathered friend proved to be more relevant for care seekers than the official ratings of the quality of care that they or their loved one could expect to receive.
“Fees are always the biggest concern for selffunding families looking for care, and they also want to know that they, or mum or dad, will feel at home,” comments Autumna’s Managing Director, Debbie Harris, “so it’s no surprise that fees and rooms were the most interrogated information on the Autumna website in 2024.”

“But the fact that only one in 30 people clicked to find out more details about the regulator ratings of the care homes they were looking at highlights just how irrelevant these are for people looking for care.”
“With inspections often woefully out of date – up to seven years in some cases – the CQC is failing to provide care seekers with information they can rely upon about the quality of care offered by providers. The regulator also doesn’t assess the things that matter most to families: detailed information on the type of care available, the quality of food, the range of activities, environmental policies – and whether pets are allowed. “
“While we welcome the admission by the CQC’s new chief executive, Sir Julian Hartley, that the regulator is not delivering, Autumna’s insights shows that it will never be able to provide all the information that care seekers need to help them choose care –and, crucially, that providers need to be able to evidence the quality of their care, facilities and service.”
“Our analysis shows that even if the CQC is able to turn itself around, the private sector will continue to have a vital role to play in ensuring care seekers can easily find information about the things that they or their loved ones need to feel truly at home in a care home.”





By David Dominy, CEO at Royal Alfred Seafarers'

Caring for someone with dementia means finding ways to connect, even when words fail. A favourite song from their youth, the feel of a textured fabric, or the gentle glow of soft lighting, these small sensory experiences can spark recognition, comfort, and joy. With dementia cases on the rise, care homes are embracing sensory therapies to help residents feel more engaged and at ease in their surroundings.
According to Alzheimer’s Society, an estimated 55 million people were living with dementia in 2024, with numbers projected to reach 139 million by 2050. As the condition becomes more common, care providers must continue exploring new ways to improve residents’ quality of life. One of the key ways to do this is through sensory care - providing mental stimulation in a way that is calming, engaging, and tailored to each individual.
Research shows that providing sensory care for older adults living with mild to moderate dementia can do wonders for their mental well-being. In late 2024, we introduced a specialised sensory room at Belvedere House for residents with dementia. The interactive space uses projections to offer a variety of activities, including games and arts. These features are designed to stimulate, engage, and enhance the cognitive skills of impacted residents, as well as being fun.
Technology in dementia care is showing great results, but care must be tailored to each individual, there's no one-size-fits-all solution. Interactive sensory experiences can make a real difference in dementia care, helping to bring comfort, spark memories and encourage engagement. Dementia can be incredibly isolating, so creating opportunities for social interaction is essential. At our care home, we’ve seen first-hand how games and activities bring residents together in ways that feel natural and enjoyable. In some cases, residents in later stages of dementia, who had become withdrawn, have shown noticeable improvements in mood and behaviour, attentiveness and interaction with their surroundings. Alongside our new sensory room, we continue to offer music sessions and live performances, both of which have proven to be incredibly valuable for our residents. The therapeutic benefits of music for individuals living with dementia are well-documented. Our ability to listen is one of the most powerful senses we have, and so music can serve as a powerful prompt for reminiscence and stirring up memories. It also reduces stress and feelings of

isolation while allowing residents to express their feelings and ideas in ways that don’t require verbal communication.
To further encourage engagement and social interaction the Society, with support from partners, is investing in interactive screens that offer a variety of activities and games to stimulate, engage, and enhance the cognitive skills of impacted residents. They also provide easily accessible ways to make calls to loved ones. Providing a variety of options supports the tailoring of our care to the needs and preferences of the individuals.
Recognising and accepting the brain changes that cause dementia can help carers to adopt suitable responses and methods of communication. Whether through music- in all its formsart, or interactive games, these alternative forms of expression can help bridge communication gaps that oftentimes arise due to dementia.
Providing great dementia care isn’t just about meeting daily needs, it’s about understanding the condition, adapting to challenges, and helping residents feel safe, supported, and valued. That’s why well-trained staff are at the heart of truly person-centred dementia care. Care homes must make sure their teams have the specialised knowledge and practical skills needed to support residents with dementia. When staff understand not just the physical needs but also the emotional and cognitive challenges of dementia, they can provide the right care, create meaningful moments and significantly improve residents’ quality of life.
In 2011, we opened the UK’s first specialist dementia unit for seafarers at our Belvedere House nursing home, after staff identified that 40 per cent of residents at the time had some form of dementia or cognitive impairment. The care unit has provided valuable insights into the benefits of early diagnosis and various types of therapy, physical and mental.
During this time our dedicated care workers have implemented various techniques to support our residents, including the use of memory boxes and personalised one-on-one therapy sessions. In recognition of the diverse needs of our residents, specialised training even extends to our catering team. This ensures that residents requiring texture-modified diets receive appropriate and nutritious meals tailored to their needs. Coloured food plates at mealtimes have also seen great success, encouraging independence and reducing confusion and stress.
By providing cognitive stimulation through various sensory experiences, care facilities can offer meaningful interactions and engagement opportunities for their residents.
As dementia care continues to evolve, integrating sensorybased therapies will become even more essential. At the Royal Alfred Seafarers' Society, we are committed to continuing to provide innovative, resident-centred care that ensuring that those we support receive dignity, joy, and connection every day.
Chiltern Water & Environment was established in 1991 by Robert Hunt after gaining 25 years' experience as an operational and analytical scientist in the water supply industry. The company gained engineering and further management knowledge when David Hunt joined in 2012. Since then, other water industry professionals have added to the breadth of knowledge and experience within the company.

We have always provided high-quality consultancy, testing and remedial services in a professional but personable manner. Our steady growth has reflected our clients' trust in our services. Our current clients include large housing associations, pharmaceutical companies and facilities management companies, as well as individual landlords and small businesses. We ensure all our customers receive the same level of care and attention to detail.
Duty Holders of all commercial and public building premises are legally required to assess the risk from legionella to anyone using the water systems and put in place legionella control measures if required. The HSE has produced ACoP L8 and HSG274 as guidance for Duty Holders obligations. We have clients throughout the South East, London and the Midlands, and carry out water tests nationally and internationally. We currently provide regular water sampling and testing for over 500 sites.
Tel: 01844 347678
Email: info@chilternwater.co.uk www.chilternwater.co.uk

A new report launched by the independent national charity, Community Integrated Care, today (Wednesday 12th March) exposes a persistent pay gap between social care support workers and their NHS counterparts. The charity is calling on the Government to take immediate action by uplifting care worker wages, arguing that fair pay is not only affordable, but a crucial investment in economic growth and the long-term sustainability of the NHS.
‘A Caring Economy – Unfair To Care 2025’ is the fourth edition of Community Integrated Care’s acclaimed Unfair To Care report series. It uniquely compares the pay of social care support workers to their NHS equivalents paid under Band 3 of the NHS Agenda for Change framework.
Using exclusive measurement by global leaders in job evaluation, Korn Ferry, the charity has determined that the role of a social care support worker is a skilled, accountable and complex one, revealing that the average care worker, currently earning £12.00 per hour, would take home £7,120 a year more doing a comparable sized role in the NHS.
The charity says that the consequences of this pay disparity are severe, including high turnover rates of 26.5%, equivalent to 285,000 leavers a year, combined with vacancy rates of 9.4% or 112,000 roles. These challenges create a cascade of far-reaching and negative impacts across society – reducing quality of life for people who access or work in care, undermining the viability of care providers and the efficiency of the NHS, and constraining economic growth.
Recent unfunded increases to employer National Insurance Contributions and the National Living Wage, totalling around £2.8 billion, have further exacerbated the problem, creating financial strain on care providers, with many having to make difficult choices to hand back contracts to local authorities, or in some cases, leave the care market entirely.
The release of this report comes at a critical moment as the Government reviews national social care policy, including proposals for a Fair Pay Agreement for care workers – acknowledging the urgent need for improved wages and the impact of low pay on the NHS. However, with the agreement not expected until 2027, at the earliest, Community Integrated Care warns that delaying action will only deepen the crisis; they claim that it will exacerbate workforce instability, continue to disrupt the lives of millions who depend on and deliver social care, and fatally undermine one of the Government’s three big shifts: moving care from hospitals to the community.
The charity argues that immediate action is needed and that increasing social care pay is both achievable and essential. Their estimates show that a 50p per hour uplift for the 1.29 million frontline care workers in England, would cost just £723 million per year (net) – a small proportion of the annual £32 billion in public spending on adult social care, and a fraction of the recent £25.7 billion NHS funding boost in the Autumn 2024 Budget. In return, fair pay would reduce costly staff turnover, improve retention, and enhance care quality – benefiting the entire health and social care system.
Previous reports have shown that providing parity of pay between social care workers and their NHS equivalents creates a ‘Social Care Triple Care Win’, improving economic growth, as lower paid workers reinvest additional wages in the local economy, increasing NHS capacity and efficiency, and transforming the lives of people who work in and draw on social care.
Teresa Exelby is the Chief Corporate Services & People Officer at Community Integrated Care, which employs over 6500 colleagues and delivers 10 million hours of publicly-funded support to 2500 adults with learning disabilities, autism, mental health conditions and complex needs. She said: “Once again, this year’s figures highlight the persistent undervaluing of one of society’s most vital workforces. Social care support workers are highly skilled, accountable, and emotionally resilient, delivering transformational care and support every day.
While steps toward a fairer pay framework are welcome, we cannot wait for 2027 for that to happen. That’s why we are urgently calling on the Government to fund an immediate interim pay uplift – not just because it’s the right thing to do for those working in and accessing social care, but because of the benefits it brings for wider society and the economy too.
Within our charity we’ve seen the transformational impact of raising pay and investing in carers – achieving an 80% retention rate, which is above the sector average. This stability enables us to reinvest, expand our impact, and support our teams to deliver high-quality care, but sustained progress requires proper funding. With the right investment, social care can thrive – offering sustainable, rewarding careers, empowering people to live their best lives, and driving economic growth and productivity.”
Phil Hope, former Minister of State for Social Care and co-author of the report, said: “A ‘Caring Economy’ is a two-way street – a strong economy funds the delivery of care and support, and the social care sector, in turn, drives economic growth and enhances NHS productivity.
The sector is vast and expanding, contributing an estimated £62.1 billion to gross value added in England. Yet, despite its undeniable impact, improved care worker pay remains a contentious issue, often deemed unaffordable. This report not only challenges that perception but also highlights the substantial economic returns it can offer – reducing welfare spending, creating employment opportunities, and stimulating spending in low-income communities.
In reality, the cost of increasing care worker pay could be far lower than assumed. Better wages lead to a more stable workforce, lower recruitment costs, and greater investment in training and innovation. It’s time to recognise social care spending as an investment in our economy and society – not just an expense.”


• We specialise in the sale and purchase of quality used wheelchair accessible vehicles and ambulances.
• They can be bought as seen or refurbished and sign-written to your own requirements.
• Fully serviced, new mot & warranty
• Engineers inspection supplied if required.
• Free delivery service available
• All buses comply with new legislation
•
• Lease hire and purchase


By Kathryn Smith OBE, Chief Executive of

A major shift is underway at NHS England. With Dr. Penny Dash set to succeed Richard Meddings as Chair and Sir James Mackey set to succeed Amanda Pritchard as Chief Executive, an entirely new leadership team will now be responsible for developing and delivering the Government’s 10-Year Health Plan.
This transition comes at a crucial time—for both the NHS and social care. As Lord Darzi's investigation observed, the NHS’s financial and operational sustainability cannot be achieved without strengthening social care. Health and social care cannot function effectively in silos; they are interdependent—and adopting a holistic approach that considers someone’s journey across the health and social care systems is essential.
Social care plays a crucial role in alleviating the immense strain on NHS high-acuity services by reducing discharge delays and preventing unnecessary (and costly) admissions and readmissions—but also, and more importantly, allowing people to live rich and fulfilling lives. According to recent NHS England data, patients who are medically fit for discharge occupy 13,767 hospital beds per day.
The path forward is clear: Achieving the NHS reforms will depend on a parallel investment in social care services. This is the case for all three policy shifts expected in the NHS 10-Year Plan.
Through local care services we can deliver personalised, high-quality, and financially sustainable services that meet the care needs of people in their communities and allow them to live independently for longer— thus improving NHS efficiency.
What’s needed is tangible investment and prioritisation of all community services to relieve the strain on local health and care systems.
However, in its current state, the social care sector faces significant and critical challenges: inflation, demographic and epidemiological changes, falling recruitment and retention, and rising demand are placing immense pressure on care and support services and impacting their quality and availability. As a result, the
sector relies heavily on unpaid carers who, sadly, often do not get the recognition or support they deserve.
As the new figures in the NHS leadership team settle into their posts, we encourage them to look backwards in order to pave a way forward. During the COVID-19 pandemic, SCIE observed both health and care leaders working more collaboratively. We found that NHS-funded post-discharge care packages significantly improved the timeliness of hospital transfers and reduced lengthy hospital stays.
The human case for joint investment is critical. Take intermediate care, for example. Intermediate care services are provided to patients, usually older people, after leaving hospital or when they are at risk of being sent to hospital. Our research indicates that 70% of people who received intermediate care after a hospital stay returned to their own homes, while 72% did not move to a more dependent care setting—giving them the crucial opportunity to maintain their independence, dignity, and quality of life.
The economic case for investment is also compelling: wider sector research demonstrates that every £1 invested in earlier action and support, including intermediate care, achieves an ROI of, on average, £3.17. Acting on known interventions shouldn’t depend on where the benefits accrue. We should consider the effects on ‘whole systems’ instead.
Beyond funding, we also need to find new ways to deliver social care more efficiently and effectively. For example, there are substantial opportunities to enhance post-discharge assessments and care, particularly through reablement services. Reablement is a short-term, intensive intervention aimed at helping individuals regain or maintain their independence after events like hospital admissions.
SCIE published a series of evidence-based and practical recommendations in 2024 in our ‘Supporting client and family engagement with reablement’ resource to address the barriers that can prevent people from fully benefiting from reablement. Resources like this can help streamline care delivery, ensuring that support is targeted, timely, and productive.
The Government’s vision is for an NHS that is both resilient and sustainable—but turning that vision into reality requires decisive action. The adult social care sector, employing approximately 1.59 million people and contributing approximately £68.1 billion to our economy annually, is a ‘sleeping giant’ of largely untapped potential.
If we get future reforms right, we can tackle the pressures facing both health and social care and create systems that are fit for the future.
Opticians could play a key role in identifying people at risk of dementia by spotting distinctive patterns in the back of the eye linked to early signs of the condition, according to new research funded by Alzheimer’s Research UK.
An artificial intelligence (AI) tool has identified differences in the shape and size of blood vessels at the back of the eye that correspond to cognitive health, according to research led by scientists at City St George’s, University of London.
The study, funded by Alzheimer’s Research UK, could open the door to a new diagnostic tool that experts say could complement existing tests, like brain scans, to help ensure people get the full picture of their dementia, and the support they deserve, more quickly.
The AI tool, called Quartz, can analyse eye scans in seconds, identifying key differences in the shape and size of tiny blood vessels in the retina – known as arterioles and venules. These blood vessels in the eye serve as an extension of those in the brain, providing a unique, non-invasive window into brain health.

Using Quartz, researchers at City St George’s scanned the eyes of more than 63,000 people aged 40 to 69. They then compared the images with cognitive test scores measuring memory, reaction time, and intelligence.
The researchers found that those with retinal blood vessels that had reduced width and had particular patterns of twisting were linked to lower scores in tests for memory, reaction time and intelligence.
Scientists believe changes in retinal blood vessels may be due to reduced blood supply in the brain, which in turn may be an early cause or consequence of diseases such as Alzheimer’s.
Social Care TV continue to fly the flag for highest quality online training for Health and Social Care, after unwavering commitment to excellence within the sector for over 25 years.
Their widely-used health and social care specific courses - produced and edited in-house - are expertly designed to make learning engaging, informative and, therefore, highly effective for learners.
Accredited by CPD and endorsed by Skills for Care, training with Social Care TV is quality assured, comprehensive and relevant.
As one of the leading online training providers in the health and social care sector in the UK, they supply training for local authorities, recruitment agencies, care home groups and other health and social care organisations.
Their feature-rich Manager platform has further been enhanced this year with the introduction of several new Manager tools designed to aid with compliance, reporting and trainee management. Features now available include:
• Compliance Dashboard with Traffic Light System
• Downloadable Trainee Matrix
• Custom Bundles
• Trainee Groups
• Bulk Uploads
Prof Chris Owen, lead author of the study, said the technique could one day be “seamlessly embedded” into the daily routines of high street opticians and eye clinics.
“It would provide an easily accessible, low cost and quick way to flag people who are at risk of developing neurodegenerative conditions in the future without the need of invasive tests.”
Prof Owen now plans to use Quartz in other studies and populations to see how it could be used more widely in the healthcare sector.
Currently, a dementia diagnosis involves a series of tests which assess memory, thinking and overall wellbeing. Sadly, many people with dementia don’t ever receive a formal diagnosis. In fact, around one in three people over 65 with dementia in England remain undiagnosed.
David Thomas, Head of Policy and Public Affairs at Alzheimer’s Research UK said this must change.
“People are waiting too long for a dementia diagnosis, often struggling to even get through the NHS front door. Detecting early signs of dementia, for example through a routine eye test at your local optician, would be a gamechanger. Integrating these scans with existing tests, like brain scans, would ensure people get the full picture of their condition, and the support they deserve, more quickly.”
Thomas also highlighted that this innovation aligns with government ambitions to shift more healthcare services into community settings.
“The upcoming 10-year health plan must ensure the NHS is able to rapidly pilot and adopt new innovations such as eye scans into routine healthcare settings,” he added.

• Bulk Enrolment Onto Custom Bundles
• Course Enrolment Notifications
• Course Reminders
SCTV regularly release new and updated high-quality courses. Previews for all courses can be viewed at: Courses - Social Care TV (www.social-care.tv/courses/course-details)
To enhance their learners' experience further they have created free, comprehensive subject-specific workbooks which were rolled out across all courses this year. This unique addition provides excellent value and a fully robust training package.
SCTV are delighted to have won several awards over the last 12 months including:
• Best Online Health and Social Care Learning Platform’ – Global
Health & Pharma Social Care Awards 2024
• ‘CPD Provider of the Year’ – The CPD Awards
• Social Care Training Provider of the Year’ - Corporate Livewire
Innovation & Excellence Awards
Gold standard customer service remains a core staple of the business, with expert support and guidance provided via telephone, email and live chat. They place great importance on the training and development of their customer services team to ensure that they continue
to provide a personal, friendly and knowledgeable service.
Their much-loved ‘Care Worker of the Month’ award recognises and rewards the selfless dedication shown by care workers across the UK and they proudly support the Care Workers Charity who aim to advance the financial, professional and mental wellbeing of social care workers.
SCTV believe that high quality training should be accessible to all and offer regular, free courses which include a digital certificate accessible via their website.
The company stands behind a clear mission and set of values which define their ethos and their dedication to both the Care Sector and those within it. These can be viewed at: Mission Statement and Core Values - Social Care TV
(www.social-care.tv/about/mission-statement-and-core-values) Social Care TV are a responsible business, committed to ensuring that their actions have a positive impact on their employees, customers, the wider health and social care community and the environment.
Above all, SCTV consistently strive to make a meaningful contribution to the wellbeing of those being cared for.
For more information please see: Homepage - Social Care TV (www.social-care.tv) and see advert on the facing page.
An investigation has uncovered a link between “rock bottom” care home fees and bed blocking in Welsh hospitals.
The research was conducted by social care champions Care Forum Wales (CFW), who say that elderly people who should be in care homes are taking up desperately needed beds and “creating an even worse crisis in an already beleaguered NHS”.
According to CFW, who represent around 500 independent providers, the study discovered that the Health Board areas with the highest rates of patients awaiting discharge were those where local authorities paid the least for care.
The Health Boards with the highest rates of patients awaiting discharge to a care home are Betsi Cadwaladr in North Wales and Hywel Dda in South West Wales, both hovering around the 70 per cent mark. Care Forum Wales Chair Mario Kreft MBE has written to Senedd Members drawing their attention to the report.

He said: “It shows there is a strong correlation between inadequate fees and high levels of delayed hospital discharges.
“That is affecting not only those individuals who need to be cared for in a more appropriate environment, but those with acute medical conditions waiting for vacant beds.
“Local authorities are protecting budgets at the expense of keeping people in hospital.
“At the same hospitals where these beds are being blocked there are lengthening queues of ambulances outside, waiting to discharge patients. These patients who are bed blocking can be safely placed in care homes.
“In those queuing ambulances people are dying while they wait for a bed in a hospital to become free. “It’s the simple joining of the dots and if we are to become serious about getting people out of hospital and into the appropriate care setting then we need to have a different mindset to this budget-driven nonsense.
“Local authorities are protecting their budgets at the expense of people’s lives – it makes no sense to have a system like that.
“The result is elderly people are unnecessarily staying in a hospital bed at a cost of £500 a day to the public purse while there are many available beds in care homes for less than £200 a day.
“It needs to be radically reformed but no-one in Wales seems to be able to make that decision.
“We fear there will be many more care home closures and redundancies from April, when the UK Government is set to increase employer National Insurance Contributions in what amounts to a tax on people’s care.
“This could mean the number of available beds decreasing. Social care is the solution to the NHS crisis and should be protected.
“We are calling for immediate action to avoid redundancies and closures of the vital care home and domiciliary care services underpinning the NHS.” CFW’s league table showing how much local authorities pay for care, five of North Wales counties are in the bottom six places showing the lowest payers.
According to CFW, it is no coincidence that two of those authorities, Gwynedd and Anglesey, over 80 per cent of bed blockers are waiting for places in care homes.
Just above them and firmly in the bottom half of payers are Neath Port Talbot, Swansea and Carmarthenshire where care home bed blockers account for over three-quarters of the patients awaiting discharge.
In contrast in the Aneurin Bevan Health Board area fewer than 18 per cent of patients awaiting discharge are going to care homes and three of their five local authorities, Newport, Torfaen and Blaenau Gwent, are in the top five care home fee-payers.
Cardiff, first, and Vale of Glamorgan, seventh, are top 10 fees payers and only 26 per cent of their outgoing patients are waiting for care home places while sandwiched between them is the Cwm Taf Morgannwg where the fees are lower and the picture is different.
Meanwhile, Bridgend Council, where 80 per cent of bed blockers are waiting for places in care homes, and Rhondda Cynon Taf, 63 per cent, are 14th and 12th in the table and Merthyr, 56.4 per cent, are tenth.
Mr Kreft added: “These figures are publicly available from the NHS Wales website and they show a very stark picture.
“In most areas costs for care providers are broadly the same so wherever the local authorities are paying very low fees most care homes will be charging the families of residents top-up fees.
“Providers trying to run a sustainable business naturally struggle with the low fees set by these authorities and have to resort to additional fees from families to cover the funding shortfall.
That leads to a situation where the local authority is restricted in finding suitable care beds, especially where additional family payments are not available.
“You end up in the ridiculous situation where large number of beds costing less than £200 a night are empty while there are people stuck in hospital beds, which cost £500 a night, waiting for a care home place.
“It’s short-sighted and counterintuitive. The NHS is paying out a fortune for people in hospital beds costing two and a half times what a care home bed costs and outside ambulances are waiting hours in car parks for a bed to become free.”


The Care Workers’ Charity (CWC) has published a landmark report summarising key insights from a series of roundtable discussions on the future of adult social care in England.

Held in November 2024, these discussions brought together care workers, people drawing on care, unpaid carers, care providers, commissioners, and advocacy groups to examine the challenges facing the sector and ideas for reform.
The report outlines key priorities for reform, including the need to elevate the status of care work, ensure sustainable funding, and embed the voices of care workers and those drawing on care at the heart of decision-making. Any transformation must be properly resourced to be effective.
Participants also called for a wider national conversation on how society values care, ensuring that reforms move beyond crisis management towards a system that supports dignity, autonomy, and fulfilling lives.
Among the core themes highlighted in the report:
• Centring Care Voices – Social care reform must be shaped by those most directly impacted: frontline care workers, people drawing on care, and unpaid carers. Their voices must be at the heart of decisionmaking.
• Workforce pay and conditions remain a critical issue, with strong support for a £15 per hour minimum pay standard, career development pathways, and better training opportunities.
• Professionalisation of the sector, with calls for a national registration system and professional body for care workers.
• Funding reform is essential, with a need for multiyear financial settlements and equitable commissioning practices to ensure sector stability.
• Social care must be recognised as a distinct sector, working alongside, but not secondary to, the NHS.
• Addressing structural inequalities within social care, ensuring equitable access and working conditions for all.
Karolina Gerlich, CEO of The Care Workers’ Charity, said:
“This report is a call to action. Now could be a turning point for social care, but only if it is backed by sustained investment and shaped by those on the frontline. Our roundtable discussions demonstrated the urgent need for reform—not just in funding, but in how we value care as a society. This is about creating a system that works for care workers, for people drawing on care, their friends, family and wider community now and for the future.”
The Full Report is available to download here


Signature Senior Lifestyle celebrated International Women’s Day by spotlighting the incredible journey of Anya Salisbury, who has risen through the ranks to become Senior Procurement Partner at just 22 years old.
Having joined Signature at just 16, Anya has navigated challenges, embraced opportunities, and carved out a thriving career in procurement – an industry where women remain underrepresented.
Reflecting on her journey, Anya shares: “Procurement is a dynamic field, and that’s precisely what I love about it. Every day presents new challenges and opportunities, making each day unique. I’m proud to be in a role where I can contribute directly to Signature Senior Lifestyle’s success while working with incredible teams across the business.”
Anya’s rapid rise has been shaped by a diverse range of experiences. In early 2022, she took a brief detour into events management, a career path she had long envisioned for herself. However, despite strong support from her line manager and the organisation’s commitment to her development, she quickly realised that her true passion lay in procurement.
Returning to the field, Anya found herself at the heart of Signature Senior Lifestyle’s transformation. In mid-2023, during a period of significant company change, she transitioned from a five-person procurement team to working alongside just one other colleague, facing an entirely new level of responsibility. She recalls: “Without the guidance of someone with prior experience, I had no choice but to embrace the challenge and learn on the job.”

Six months later, Anya was working on key development projects, including Signature’s opening of its prestigious flagship Signature at Highgate care home, an experience that she describes as a turning point in her career. She says: “That was the moment I went from raising purchase orders to making an impact. After weeks of chaos and long hours, I realised I was capable of more than I had ever imagined.”
Beyond day-to-day operations, Anya has played a pivotal role in shaping Signature Senior Lifestyle’s pro-
curement strategy, overseeing collaborations with esteemed brands such as TBCo, and Amarante. She also led the transition to a new uniform supplier, enhancing comfort for frontline care colleagues, and partnered with IT to develop an in-house support portal app for Client Liaison Managers.
Her work has also sparked a keen interest in Environmental, Social, and Governance (ESG) initiatives—an area she is now proud to influence as a member of Signature’s ESG board. “Some of my biggest achievements are currently in the works and set to be implemented in Q2 of this year,” she shares.
Anya’s story is a powerful testament to the importance of finding your own path –a message she hopes will inspire other young women considering careers in procurement: “It’s easy to feel pressured to follow a path that looks glamorous or popular, but what truly matters is finding a role that makes you feel fulfilled. I thought I had my whole career mapped out, only to realise my passion lay somewhere completely different. It doesn’t matter if your ‘dream job’ isn’t what you expected – what matters is that you find something that excites and challenges you.”
Procurement, she believes, is an exciting and high-impact field where women can thrive and lead: “This is a career where you can work across multiple disciplines –sales, marketing, hospitality – whatever interests you. It’s about problem-solving, creating value, and making a difference. If you find a company that trusts you to do what you specialise in, the opportunities are limitless.”
As she continues to advance her career, balancing a full-time role while pursuing CIPS Level 4 accreditation, Anya remains committed to lifelong learning and professional growth. She shares:
“Short-term sacrifice for long-term success is something I live by. There’s always more to learn, and being open to education is one of the best things you can do for your career.”
Her journey, marked by perseverance, adaptability, and a drive to challenge expectations, serves as an inspiration this International Women’s Day – not just to women in procurement, but to anyone striving to make their mark in their chosen field.
This winter, Recreo VR is offering care homes an exciting opportunity to enhance resident wellbeing through the power of Virtual Reality (VR). By signing up for one of our 24-month Recreo Theatres packages, you’ll receive a free VR headset and staff training.
Our platform provides person-centred, budget-friendly activities that are fun, engaging, and accessible, especially for residents who are bedbound or socially isolated. Co-created with Alzheimer’s Society and individuals with dementia, our service empowers staff to deliver personalised reminiscence and one-to-one sessions that promote memory recall and connection.
Our VR headsets have been recognised as good practice by the Care Quality
Commission (CQC), further validating their impact on care. Regular use of Recreo VR has a proven positive effect on wellbeing, with residents reporting increased activity, engagement, and social connection, often leading to a reduction in the need for PRN medication.
Whether combating loneliness, promoting relaxation, or enhancing cognitive health, VR offers a non-pharmacological solution to enrich care and elevate quality of life. Don’t miss out! Take advantage of this exclusive offer and see how VR can transform your care home experience.
For more information, visit recreovr.co.uk. Or contact us at info@recreovr.co.uk or 01482 526940.




To mark International Women's Day, which took place on Saturday 8th of March, Sue McClean discussed her journey to becoming Director of Operations at Audley Villages (www.audleyvillages.co.uk) and the importance of balancing family and work.
I have worked at Audley for over thirteen years, starting as Club Services Supervisor and working my way up to Village Manager, General Manager, Regional Operations Director, and to now being Operations Director for the Group.
I began working at Audley when I re-entered the workforce after a number of years raising my children. I was fortunate to join their Operations Director Training Programme and am now leading the initiative, alongside the General Manager Training Programmes, to support the development of others within the company
In the late 90s, I took time out to raise my family. I had five children with the last two being twins so I decided I would wait until they were heading into Secondary school before going back into the workforce. It was important for me to not lose my identity and reclaim my former professional career. I never thought I would one day reach director level within my operations remit. My
Operations Director at the time gave me a book called ‘Start with why – How great leaders inspire everyone to take action’ which was incredibly inspiring to me. It sounds simple, but it really made me think about what I was doing and why I was doing it. I became focused on opening my mind to the fact that I wasn’t starting from scratch again; and was able to feel empowered that I had the skills to pick up where I had left off before I had my family. I pushed myself and continued to drive forward with the support of Audley. I am on the road one or two days per week visiting a number of the villages across the country so no two days look the same but I always try to create an ongoing circular route to keep my commute to a minimum. I like to make sure my commute is productive for thinking time so once I arrive I can spend time with the village team and homeowners.
As a child, I wanted to be a librarian, but as I’m one of the most energetic people on the planet, my mum told me that was ridiculous. I’m a people person, and I thrive in a busy environment, so I’d say my career path has brought me to exactly where I should be.
International Women’s Day is all about accelerating action for gender equality. I truly believe that if it wasn’t for the people in my life and the inspiration I took from that book all those years ago, I would not be where I am today. Raising a family is incredibly important and something that statistically weighs more heavily on the woman, but this does not mean you have to sacrifice your career and professional goals. I am incredibly grateful to be in the position I am in and hope other women will continue to find that balance of raising a family and working.
Royal Air Force veteran Gerry Cassidy, 91, is among those living at a recently certified “Veteran Friendly” care home in North Yorkshire.
Gerry is one of several residents at Sycamore Hall Care Home, on Kearsley Road, Ripon, benefitting from the enhanced care and support provided to those who served in the armed forces.
The care home has now received Veteran Friendly Framework (VFF) status for its care provision, part of an armed forces charity backed scheme being rolled out across the country.
The VFF initiative was launched in 2023 with the aim of tackling loneliness and isolation and delivering improved health and wellbeing outcomes for over 25,000 veterans living in care homes across England.
It is a collaboration between Armed Forces charities Royal Star & Garter and Royal British Legion, and NHS Veterans’ Covenant Healthcare Alliance (VCHA), with funding support from the Armed Forces Covenant Fund Trust.
At Sycamore Hall Care Home, staff, residents, family members, charity representatives, veterans, and local dignitaries all gathered to celebrate the care home receiving VFF status.

Among those at the celebratory afternoon tea was Ripon Mayor Cllr Sid Hawke and his wife Mayoress Linda Hawke, alongside North Yorkshire Council Cllr Kevin Foster, Armed Forces Champion for North Yorkshire.
Guests also included Mike Chambers MBE, president of the Royal Air Force Association Ripon branch,
The pobroll® is the invention of Pat O’Brien, a physiotherapist, Moving and Handling trainer, and Conflict Management tutor with over two decades of experience in care homes and nursing homes
Care home managers often face challenges in delivering intimate care while balancing efficiency and managing costs, particularly when these essential tasks provoke behaviours that can be challenging to safely manage. Traditional methods—especially for bed-bound residents—often lead to lengthy processes and frequent linen changes, driving up costs and consuming valuable staff time. The pobroll® provides a transformative solution that supports dignified care, achieves significant cost savings, and reduces the need for additional staffing.
The pobroll® is an innovative bed-bathing wrap specifically designed to enhance comfort and dignity during personal washing for individuals who require in-bed care. Centred on the resident’s experience, it minimizes distress by providing sensory comfort. Crafted with two layers of high-quality cotton-terry toweling and a waterproof layer in between, it delivers a soothing, calming experience while keeping the bed completely dry. Sized for a standard single bed, the pobroll®’s dual-layer design offers warmth and a sense of security and privacy, allowing residents to maintain comfort and dignity during bed-based bathing routines.
BOOSTING COST SAVINGS AND OPERATIONAL EFFICIENCY
Smith, chair of the
branch, and Jim Phillips, chair of the Royal Engineers Association, alongside other members of the veteran organisations.
Jules Walker, VFF support project officer for Royal Star & Garter, was also among the guests, which included the care home’s own veterans and veteran champions.
Ewelina Sosnowska, home manager at Sycamore Hall Care Home, said: “We are incredibly proud to have been recognised as a veteran friendly care home. This award reflects our unwavering commitment to honouring and supporting those who have served in the armed forces.
“At Sycamore Hall we strive to create a welcoming environment where veterans feel valued and understood, tailoring our care to their unique needs and experiences. This recognition is not just an achievement, but a reminder of the vital role veterans play in our community, and we remain dedicated to ensuring they receive the respect and care they truly deserve.”
Kathryn Glass is the VFF project lead at Royal Star & Garter and responsible for supporting and assessing care homes going through the scheme.
She said: “The applications submitted by Sycamore Hall Care Home was of an exceptionally high standard and a testament to the dedication, passion, and commitment they have for providing high-quality person-centred care for their residents.”

pobroll® provides an effective solution that supports both economic and environmental goals.
Managing resident agitation—particularly for those with dementia—often requires specialised training in restraint techniques. The pobroll® significantly reduces the need for physical intervention by providing a warm, secure covering that alleviates resident distress. This gentle approach minimizes aggressive or defensive reactions, reducing the number of staff needed for these interactions. As a result, facilities can potentially lower staffing levels without compromising care quality, yielding substantial cost savings. Additionally, reduced dependence on physical intervention decreases training costs associated with restraint techniques. By simplifying the process of intimate care, the pobroll® reduces the need for specialised training, making onboarding smoother and lowering turnover-related training expenses.
The pobroll® supports compliance with restraint reduction guidelines, helping facilities minimise documentation burdens and regulatory liabilities linked to physical interventions. This non-invasive solution improves safety for both residents and caregivers, fostering a culture of dignity and respect that boosts satisfaction among residents and their families.
CONCLUSION: A VALUABLE ASSET FOR QUALITY CARE AND COST MANAGEMENT
The pobroll®'s waterproof design enables caregivers to provide a complete wet wash without the risk of soaking the bed, minimising the need for frequent linen changes. This leads to fewer laundry loads, reducing labour and utility costs, as well as wear on linens. By reducing logistical tasks, caregivers have more time to focus on direct resident care, enhancing productivity overall. Additionally, reduced reliance on disposable wipes results in further cost savings and supports environmentally sustainable practices. With its durable, reusable design, the pobroll® maintains hygiene standards and allows for extended use across multiple residents. As care homes face increased pressure to adopt sustainable practices, the
For care homes, the pobroll® represents a strategic investment, offering measurable savings by reducing reliance on disposable products, lowering laundry and training costs, and enabling efficient staffing. Most importantly, it prioritises resident dignity and comfort, setting a high standard for compassionate, personcentred care. For facilities seeking to enhance financial performance and care quality, the pobroll® is an invaluable addition to their resources.
Fof further information, see the advert on the facing page.
The National Institute for Clinical Excellence (NICE) published further draft guidance for public consultation that continues to not recommend Alzheimer’s treatments donanemab and lecanemab.
NICE said that its independent committee said last year that the medicines showed too little benefit to justify the significant additional cost to the NHS of providing and administering them.
The committee asked for some additional evidence to be provided, which has now happened, and the committee has considered this. Unfortunately this has confirmed that the medicines are not currently cost effective and the committee’s recommendation remains that they should not be provided on the NHS at this time.
NICE draft guidance will allow stakeholders to comment on the key new conclusions the independent appraisal committee reached at its second meeting, and will be providing the companies and other stakeholders the opportunity to submit new evidence or commercial proposals that might address the issues that have so far been a barrier to the use of these new treatments in the NHS.
The cost-effectiveness estimates for donanemab and lecanemab remain substantially higher than we can consider an acceptable use of taxpayers’ money and NHS resources.
The evidence presented so far shows neither donanemab nor lecanemab provide enough benefit to justify the substantial resources the NHS would need to commit to implement access to them, even with a managed access arrangement.
Stakeholders are particularly encouraged to comment on the committee’s latest conclusions regarding managed access arrangements and evidence requirements.
Managed access arrangements can allow NHS patients to use promising and potentially cost-effective medicines for a fixed period, at a discount to manage the uncertainty to the NHS, while further evidence is gathered on how those medicines can be provided and how well they work outside clinical trials.
The public consultation on our draft guidance on donanemab and lecanemab will close on 27 March 2025. The independent committee will consider all responses, including additional analyses, at a third committee meeting before producing its final draft recommendations.
Professor Fiona Carragher, Chief Policy and Research Officer at Alzheimer’s Society said: “These NICE recommendations will remain disappointing for people eager to see these treatments readily available, though we continue to respect the decisions of the regulator. We appreciate their rigour and flexibility in their review of the first disease modifying treatments for Alzheimer’s disease.”
“We hope that learnings from this process will pave the way for future treatments, and with over 120 other drugs in trials for Alzheimer’s disease we may see more drugs submitted for regulatory approval in the near future. Alzheimer’s Society will continue to be a voice for people affected by dementia in the appraisal of these emerging treatments.”
Residents at Riverdale Care Home in Chesterfield were wowed by the elegance of ballroom dancers Christine Wendy Cauldwell and John Stocks, who visited them recently.
The dynamic duo, who are social dancers and 'enjoy dancing with energy and love,’ dazzled their audience with their graceful moves, seamlessly switching between styles and encouraging residents to clap and sing along to the music.
Caroline Brownlow and Ashleigh DeGirolamo, two colleagues at the home, joined Wendy and John on the dancefloor, where they were quickly joined by several residents, and danced the afternoon away!
Wendy has been trained in ballet and tap dancing since the age of seven. She was Frecheville Carnival Queen in 1958 and was well known for appearing in pantomime and on stage shows in her younger days. She continued to tap dance and added line dancing to her repertoire in later life.
John meanwhile started ballroom and Latin dancing with his late wife Sheila in 1974. They became ballroom and Latin amateur dance champions

during the late 1970s and into the 80s, winning many competitions throughout England.
Shirley Eyre, who lives at Riverdale Care Home said: “It was brilliant to see the pair, they danced with such passion.”
Wendy Perkins, Activity Coordinator at Riverdale Care Home, said: “A massive thank you to John and Wendy for coming in and showing us their fabulous dancing, letting our residents and colleagues join in and teaching us all a move or two!”
Residents said afterwards they thoroughly enjoyed Wendy and John’s visit and looked forward to them coming back soon.
Riverdale Care Home is part of the Orchard Care Homes group, which operates 23 care homes across the Midlands and the North of England. Wendy and John’s visit is typical of both the home and the group’s dedication to enriching its residents' lives; with a commitment to crafting personalised and meaningful experiences that cater to each resident’s unique needs and preferences.

A leading care management software provider has released the findings of its 2025 Digital Social Care Record (DSCR) survey – highlighting major gaps in access to essential digital tools.
The report, published by PASS by everyLIFE, reveals that many care providers still lack access to key features such as GP Connect, electronic medication administration records (eMAR) and a friends and family portal, despite their potential to improve care quality, efficiency, and compliance.
This comes as DSCR adoption continues to rise, with government data showing that 72% of CQC-registered adult social care locations in England had a DSCR in place by July 2024 – up from 57.4% in July 2023.
While progress is being made, the survey findings highlight that simply having a DSCR is not enough, with providers needing access to the right digital tools to truly transform care delivery, especially amid ongoing challenges in recruitment, retention and funding across the sector.
The survey, completed by 447 care providers using various DSCR systems across the sector, found that confidence in digital systems is growing, with 48% of providers feeling secure in their care management technology. Many have embraced key digital tools, including digital care documentation, incident reporting and real-time care plans –demonstrating the sector’s commitment to safer, more compliant, and efficient care delivery.
However, the survey also exposes major gaps in access to essential digital tools:
• Only 38% of providers can access GP records digitally, despite GP Connect being live in England for seven years. This is a missed opportunity to improve safety with real-time access to prescriptions, allergies, and medical history.
• Just 39% use eMAR, meaning the majority still rely on non-digital medication administration, increasing the risk of errors and compliance issues.
• Nearly 40% of providers do not offer friends and family portals, despite

growing demand for transparency in care.
More broadly, core functionalities like digital rostering, GP patient data integration, eMAR, and care journey tracking remain underused, with fewer than half of providers leveraging these tools.
Overall, the findings reveal clear opportunities to improve efficiency, accuracy and safety through greater adoption of digital solutions.
Commenting on the findings, Duncan Campbell, Commercial Director at PASS and Marie Curie Advisory Board Member, said: “Better, more person-centred care should always be the goal – and technology is an affordable solution to help us get there. Our latest 2025 DSCR Survey shows great progress in digital adoption, but too many care providers still lack access to essential tools like GP Connect, eMAR, and family portals.
“I’m proud that at PASS, these features come as standard, with no extra cost to our customers. Real digital transformation is about making sure care teams have everything they need to work smarter, not harder.”
Other key findings included:
DIGITAL ROSTERING: A MISSED CHANCE TO IMPROVE EFFICIENCY
Only 30% of care providers use digital rostering, while 49% still rely on manual scheduling. This increases admin time and makes it harder to allocate staff effectively. Wider adoption could streamline workforce management and improve care continuity.
BODY MAPS: A VITAL TOOL FOR HEALTH MONITORING
42% of providers use digital body maps, while 41% do not. This means missed opportunities to track conditions like pressure ulcers. Digital body mapping enhances accuracy and early detection.
DIGITAL CHECKLISTS: A SMARTER WAY TO MANAGE COMPLIANCE
Only 37% of providers use digital checklists for onboarding and compliance, while 45% still rely on manual processes. This raises the risks of missed steps and delays. Digital tools ensure consistency and automate reminders.
24/7 SUPPORT: A SAFETY NET MANY CARE PROVIDERS LACK
42% of providers have 24/7 DSCR support, but 36% do not, leaving them vulnerable to system issues. Round-the-clock assistance reduces disruptions and ensures reliability.
CONFIDENCE IN CARE SYSTEMS: A MIXED PICTURE
48% of providers are confident in their care system, but 28% are not, and 24% are unsure. Gaps in usability and training may be affecting trust in digital tools.
Duncan continued: “The survey highlights digital adoptions within social care, while also identifying significant gaps. These areas need to be addressed to develop further efficiency, compliance, and quality of care. It is important to broaden digital solutions to deliver smarter, more integrated solutions that address changing sector needs.”
To learn more about the findings from the DSCR survey, check out www.everylifetechnologies.com/content-hub/2025-dscr-survey/ and to find out how PASS can support your care operations, visit www.everylifetechnologies.com
Approved at Full Council additional funding for adult social care includes £1.4m to increase the pay of the personal care assistants (over 400 staff) who provide care for Westminster residents through direct payments.
This will improve the quality of care for care receivers and help more people who use adult social care to employ the carer they want as they will now be able to pay a competitive salary. Direct payment recipients will now be able to offer an additional £1.50- £2.00 an hour salary for their personal assistant, so those who opt to receive direct payments to pay for their care needs will see their monthly funds increase.
An additional £1.2m is also being invested to level up the threshold at which people start to pay for their social care costs so that it is the same for everyone regardless of age. This will help over 460 residents aged under 65 to keep more of their income before paying care bills.
The approval of the budget at Full Council coincides with the launch of the new Fairer Westminster delivery plan, which outlines the council’s ambitions for the future of the city, and what it wants to achieve to make Westminster a great place to live. Led by voices and priorities from the community, the new plan aims to create meaningful change by providing effective, value-for-money services and accessible opportunities for all, so every resident in the city can thrive.
The budget sets out detailed spending plans for managing more than 20,000 local authority properties under what is called the Housing Revenue Account. The business plan includes total capital investment of £916m over the next 5 years and a total of £2.5bn over the full 30 years. The budget also sets out the business plan for funding the council’s fairer Westminster programme under its capital strategy. The Council is proposing a gross capital programme up to 2038/39 of £2.5bn, partially offset by nearly £1.2bn of income, giving a net budget of £1.3bn.
Despite the scale of new investment, the Council Tax rise equals just 48p a week for a Band D* property, which means Westminster still has one of the lowest Council Tax rates in the country. The Westminster City Council part of the Council Tax rises by 4.99 per cent overall – 2.99 per cent for council services and 2 per cent for the portion set aside for adult social care.
Cllr Adam Hug, leader of Westminster City Council, said: “Rising bills and cost of living pressures impact on everyone and I’m glad we have been able to ensure hundreds of Westminster residents no longer need to pay for their social care.
“We have also been able to look after the carers who will now receive increased pay – that is only right for people who often work long hours and provide a lifeline to vulnerable people.
“This Budget is providing security in three big ways – security of home, on the streets, and the safety net of a City Council that looks after you when you need care. This is what drives our mission to create a fairer Westminster.”
The Cleaning Show 2025 will return from 18-20 March at ExCeL, London, with industry leaders set to tackle the cleaning and hygiene industry’s biggest challenges in this year’s Conference programme. The 2025 theatre will see expert speakers from across the sector sharing insights on pressing topics from sustainability, education and workforce development to technological advancements and future preparedness.
Sustainability remains a top priority for businesses, consumers and regulators alike. The Cleaning Show 2025 will dedicate several sessions to exploring innovative solutions and practices to help the sector reduce its environmental footprint. Attendees will gain valuable insights into the practical steps required for compliance and the long-term benefits of adopting sustainable practices.
Education and development: building the workforce of tomorrow Recruitment, education and training remain pivotal for the growth and resilience of the cleaning and hygiene industry. This year’s programme will address the challenges of attracting and retaining talent and the importance of upskilling to meet future demands.

Delia Cannings, Chair of the British Cleaning Council (BCC), will open the show and announce the launch of a new website called the UK Cleaning Career Development Zone, a significant new initiative which will bring training and career development information from across the cleaning and hygiene industry sector together into one easily-accessible place, for the first time. TECHNOLOGY AND AI: EMBRACING INNOVATION
The rise of artificial intelligence (AI) and technology presents transformative opportunities for the cleaning sector. Attendees will discover how these advancements can enhance productivity, efficiency and innovation in the sessions “AI in the Cleaning Sector – Change is a Fact… But How Do We Embrace It?” and “The Evolution of Cleaning in FM”.
As the world continues to navigate the aftermath of COVID-19, the conference will also examine how the cleaning industry can be ready for future challenges.
In “Preparing for the Next Pandemic – Lessons Learned”, industry leaders including Neil Nixon, Conference Director of The Cleaning Show and Duncan Holdsworth, Head of Technical at GV Health, will reflect on the successes and shortcomings of the industry’s pandemic response and identify steps to improve resilience and readiness for potential future crises.
Paul Sweeney, Event Director of The Cleaning Show, said: "We’re proud to welcome the industry’s leading voices to the conference stage at The Cleaning Show this March.
From tackling recruitment challenges and embracing sustainability, to keeping up with technological advancements, it’s vital for businesses to learn from experts and apply these insights to their operations. This year’s Conference will deliver practical strategies to address the key trends and opportunities shaping the sector, and we’re excited to showcase the latest innovations driving the future of the cleaning and hygiene industry."

New Health Foundation analysis highlights the potential for a significant shortfall in NHS funding unless unprecedented productivity growth can be achieved.
The analysis, part of the Health Foundation’s response to the Treasury’s Spending Review, estimates the funding requirements for the NHS through to 2028/29 to meet the needs of a growing and ageing population with increasing major illness.
The government has allocated £183 billion for the NHS in England in 2025/26, with the Spending Review due to allocate funding up to 2028/29. The Health Foundation analysis projects funding needs under two productivity scenarios:
• If the NHS achieves 2% productivity growth from 2021/22 to 2028/29 (in line with the government’s target for improving productivity), the NHS revenue budget would need to rise to £198bn in 2028/29.
• However, if productivity growth is only 1% over this period (in line with the long run average), NHS funding would need to rise to £211bn by 2028/29
Lower productivity growth would add £13bn to the cost of the NHS in 2028/29.
The pandemic dealt a major shock to NHS productivity, which was 24% lower in 2020/21 compared to 2018/19. This has increased the costs of meeting rising care needs. The latest estimates from the Office for National Statistics (ONS) and NHS England suggest that productivity is still below pre-pandemic levels. While NHS England has recently reported productivity improvements in the hospital sector, sustained productivity improvements across the health service at or above 2% have not been achieved in recent times.
The Spending Review is a key moment for the government to ensure the right measures are in place to boost productivity. This includes ensuring any new funding is invested in the right places – including capital investment in buildings, equipment, technology and IT, as well as strengthening primary care and community-based services. Policy changes are also needed to strengthen the NHS’s capacity to innovate and improve, including support for staff to develop new ways of delivering services and a focus on data and management capabilities.
The Health Foundation has recently launched a new NHS Productivity Commission to explore solutions to the productivity challenge. Over the next 18 months, it will look at productivity across hospital, primary, community and mental health care settings, and develop recommendations on national policy changes to help drive long-term productivity growth.
The Foundation’s response to the Spending Review also reiterates the importance of capital investment. To match the capital investment levels of comparable countries and compensate for a decade of low investment, it estimates capital spending would need to grow by 10.2% annually between 2024/25 and 2029/30. Fixing the £14bn maintenance backlog is a key priority, and significant capital investment in tech-
nology will be needed if the NHS is to deliver the shift from ‘analogue to digital’ called for by ministers. Recent changes to Treasury fiscal rules to provide greater financial certainty for government departments, alongside new five-year capital budgets, are encouraging signs of a commitment to long term investment. The real test will be how far the government matches those ambitions with increased investment in the Spending Review.
The Foundation’s submission also highlights the need to take a long-term perspective to improve the nation’s health and support sustainable economic growth, calling for action to:
• Build on the welcome recent investment in the public health grant by restoring the grant to the real-terms equivalent of 2015/16 per person levels
• Allocate an additional £7.6bn for adult social care to meet rising demand and expand access to publiclyfunded support.
• Commit to undertaking the work needed to develop proposals to classify and protect spending on prevention by implementing a new category of public spending – Preventative Departmental Expenditure Limits or PDEL).
Anita Charlesworth, Senior Economic Advisor and co-chair of the Health Foundation’s NHS productivity commission, said:
“The government has set a huge task for the NHS to consistently deliver 2% annual productivity growth. Our new analysis underlines how important it is for the NHS to improve productivity and the potential funding shortfall that could emerge if it doesn’t. If the NHS is unable to meet the government’s target then this could create a significant fiscal headache for government who will be faced with either having to find the money from elsewhere or scale back what the NHS is able to deliver.
‘Capital spending on new buildings, equipment and technology in the Spending Review will be key to help boost productivity over the long term but reform to create the conditions for boosting productivity is just as vital. A key factor will be how quickly investment can be translated into service improvements.
‘Much is now riding on the forthcoming 10-Year Health Plan. The government’s ambitions to reduce waiting times, boost community-based services, increase the use of digital technology, and prevent ill-health are the right ones. But achieving these ambitions will require significant investment in the NHS in the forthcoming Spending Review, accompanied by a relentless focus on boosting productivity.’
Residents and colleagues from HC-One Mossdale Residence care home, in York, were delighted to attend a heartwarming community event hosted by The Rainbow Care Group at a local social club.
The gathering, designed to foster connection and celebrate community spirit, proved to be a memorable afternoon of music, dancing, and camaraderie for residents and members of the community. The event, extended by The Rainbow Care Group, brought together a diverse group of locals, offering a unique opportunity for the residents to engage in lively conversation.
The afternoon featured a mix of toe-tapping music, lively dancing, and a delicious spread of cakes and tea, ensuring everyone had a fantastic time. Attendees enjoyed a chance to form new friendships in a welcoming atmosphere.
As a token of appreciation, HC-One Mossdale residents presented The Rainbow Care Group with a card and gift, expressing their gratitude for the warm

welcome and generosity. Pauline Hagen, HC-One Mossdale Residence’s Wellbeing Coordinator, shared event brochures and details of Mossdale’s upcoming activities, including regular coffee mornings and Knit & Natter sessions.
These events offer opportunities for residents to engage, socialise, and participate in activities that enhance wellbeing and community involvement. HC-One Mossdale Residence also extended an open invitation for The Rainbow Care Group’s future events to be held at their care home, offering their space as a hub for continued community engagement.
Julie Banks, HC-One’s Mossdale Residence Care Home Manager, stated:
“We are incredibly grateful to The Rainbow Care Group for inviting us to such a wonderful event. It was a fantastic day filled with laughter, music, and great company, and we look forward to building a strong relationship with The Rainbow Care Group in the future.”
Athena Finance Director, Ben Wright, is embracing change in more ways than one. 2025 marks a pivotal time for both Ben and the company, with personal challenges shaping his outlook on health, resilience, and the future of Athena.
Last year, Ben’s family life took an unexpected turn when his father was diagnosed with aggressive prostate cancer.
Prompted by this, Ben and his brother decided to get tested themselves. While his brother received the all-clear, Ben was also diagnosed with prostate cancer. Fortunately, following surgery in November, he is now in remission and feeling incredibly grateful.
Ben is using his experience to highlight the importance of early detection and awareness.
Prostate cancer affects 1 in 8 men, and through a simple PSA blood test, many cases can be caught early. “Don’t be afraid to see your doctor,” Ben urged. “Check out the Prostate Cancer UK website and find out your risk score. A simple test could save your life.”
Determined to turn his experience into action, Ben is taking on the March for March challenge, walking 11,000 steps every day throughout the month to raise funds for Prostate Cancer UK. His journey began this weekend with a family walk, he is always supported by his wife and three daughters, and working weekday will include a gym sessions in the morning followed by lunchtime walks.
If Ben visits your home this month, don’t be surprised if you spot him out and about, getting his steps in.

The 2025/26 years is also a time of change and growth for Athena Care Homes. With the arrival of our new CEO, Lorna Rose, the company is positioned for a strong future. Lorna’s leader-
ship allows group Founder Mala to focus on expansion, ensuring Athena’s continued growth and success.
Despite these changes, the big four in finance remain the same, said Ben.
“Occupancy, private occupancy, average weekly fees, and agency usage. An increase in occupancy allows for greater investment in our people—both team members and residents—as well as improvements to our processes and systems.
“One of the key focus areas this year is enhancing our environments. We’re improving our gardens and resident spaces, with café areas currently being developed at both Cambridge homes.”
April 1st marks an important milestone, bringing a rise in the living wage and an increase in employer national insurance contributions. Alongside these changes, our private residents will see a fee uplift.
Reflecting on the past year, Ben acknowledges the difficulties and remains optimistic: “2024 felt like a dream—my dad’s diagnosis, my own, and then surgery.
But I’m one of the lucky ones. My cancer was caught early, and I avoided the need for radiotherapy. My dad endured 37 rounds, which was incredibly tough, but he’s now rung the bell, and we’re hoping for good news at his next consultant appointment.”
Ben’s March for March challenge is not just about fundraising—it’s about starting conversations. “Too many men are diagnosed late because they don’t realise they’re at risk.
Early detection is crucial. If something feels off, don’t ignore it—get checked.
“It’s an important message for every man working for us and every woman too,” said Ben, “Have the conversation with your fathers, partners, brothers and friends.”


The latest UK Care Homes Trading Performance Review 2024 shows occupancy levels rising to 88.3%, a positive sign of market recovery. However, while this progress is encouraging, it reveals significant untapped potential in how care homes attract and convert prospective residents.
Presenting care homes effectively is not just about showcasing services—it's about creating emotional connection and trust. Families are making difficult decisions in emotionally charged situations, which requires a sophisticated approach to relationshipbuilding and conversion. Care homes are offering something no one truly wants to need, making the challenge even greater.
To truly drive sustainable occupancy growth, care homes must focus on transforming the customer journey—from raising awareness to handling enquiries and guiding families through to admissions. Many providers are still missing key opportunities. Too often, care homes fall short in delivering the basics well, leading to lost enquiries and missed revenue potential.
CRITICAL AREAS NEEDING IMPROVEMENT INCLUDE:
Generating Quality Leads: It's essential to attract the right audience from the outset through targeted campaigns, high-value content, and strategic outreach across multiple channels, including community outreach, digital marketing, partnerships, referral networks, local events, print ads, and door drops.
• Empathetic First Contact: Enquiries must be handled with care, expertise, and emotional sensitivity, recognising the difficult decisions families face.
Personalised Tours: Showrounds should go beyond listing services, highlighting quality of life benefits such as personalised care plans, engaging activities, and the warmth of community life.

By Ali Powell, CEO and Founder at
Clear Value Communication: Families need transparent, outcome-driven explanations of the value of care— focusing on dignity, well-being, and peace of mind, not just amenities.
• Consistent Post-Visit Engagement: Many care homes neglect follow-up strategies after visits, losing potential residents who may need further reassurance or time to decide.
TRACKING THE RIGHT METRICS:
To ensure the customer journey is effective, care homes should track key performance metrics, including: Monthly Lead Generation: Number of leads that meet predefined criteria indicating genuine interest or fit.
Monthly Visits: The number of on-site or virtual tours conducted within the month.
• Monthly Admissions: The total number of new residents admitted each month.
Lead Source Performance: Breakdown of leads by marketing channel (e.g., online ads, social media, referrals, events) to identify the most effective sources.
Average Admission Cycle Length: The average time from initial lead generation to a confirmed admission.
Monthly Marketing Spend: Total amount spent on marketing each month.
Website Traffic: Total visitors to the website and engagement rates for the month.
Social Media: Total followers and engagement on platforms like Facebook, LinkedIn, and Instagram.
THE OPPORTUNITY:
Investing in marketing and relationship-building efforts is not a luxury—it's essential. The cost per acquisition is often minimal compared to the hundreds of thousands in lifetime revenue generated from new residents. By focusing on consistency and excellence throughout the entire customer journey, care homes can significantly impact both occupancy rates and short- and long-term growth. The data is clear: doing the fundamentals well is not just good practice—it’s essential for both immediate results and lasting success. It’s time for care homes to move beyond filling rooms and start focusing on creating an inspiring customer journey that builds confidence, trust, and emotional connection with families.
If you need an expert in this area, contact Ali at Commercial Acceleration—specialists in strategy and implementation for transformational and turnaround results.
ali@comaccel.co.uk | comaccel.co.uk
Chacombe Park Care Home in Chacombe, Banbury was full of animal magic when the lovely miniature ponies; Lollipop and Tinkerbelle trotted in to surprise the residents.
Residents at Chacombe Park were super excited to see their new little pony friends roaming around their home as the team from Lollipop Ponies Parties paid a visit. Activities Coordinator; Morgan Dowie said: “Today has
been so very special for all our residents, the ponies put a spring in all our steps!”
General Manager Shaju Paul said: “Our residents have really enjoyed their unusual visitors today. Our residents love all animals, the enjoyment and therapeutic influence animals can have on people is immediate, meeting Lollipop and Tinkerbelle today put the biggest of smiles on all our faces.”


Hickathrift House care home, in Marshland St James, Wisbech have invited residents, their loved ones, staff, locals and the wider community to join them to create a daffodil display for Marie Curie’s Day of reflection on the 9th of March.
Marie Curie is leading the nation in a UK-wide Day of Reflection on the 9th of March. The UK’s leading end of life charity is asking individuals and communities to remember the people who died, whatever the cause, and to show support for everyone who was bereaved.
Volunteers had been knitting daffodils to fill two dark blue dresses that had been donated. There are various shapes, textures and colours of yellow, orange and white, demonstrating the number of people involved in making this a unique piece, raising awareness of those on end-of-life care.

Julie, carer at Hickathrift and project lead said, “All the volunteers felt proud of their work and the residents and visitors’ reaction had been heart-warming when they saw the displays. It’s even better than I thought was possible. I feel privileged to have helped to create this”.
General Manager, Paula Melerski said: “We started this club for elderly people in the community who might want some time outside of the home and to make some new friends and it’s gone from strength to strength, creating meaningful projects together. We feel proud of the efforts that have gone into this display. It has been really lovely to see different generations getting involved, from a 90-year-old resident down to our 13-year-old Duke of Edinburgh volunteer, as well as all the family and friends of residents at Hickathrift, the staff and volunteers”.
Residents at HC-One’s Daneside Court Care Home, in Northwich, Cheshire, have been learning all about their local rivers and waterways.
In a lively and informative session, the home welcomed David Palmer and Simon Brooks, two passionate volunteers from the Canal & River Trust, who brought the rich history and natural beauty of Northwich’s waterways to life.
The volunteers presented an engaging talk about the town’s iconic River Weaver, its surrounding canals, and the remarkable Anderton Boat Lift, one of the seven Wonders of the Waterways.
This 150-year-old engineering marvel, the world’s first major commercial boat lift, continues to carry around 3,000 boats each year between the Trent and Mersey Canal and the River Weaver, lifting them 50 feet in the process. Sharon Lelonek, HC-One’s Daneside Court Wellbeing Coordinator, said: “It was an absolute pleasure welcoming volunteer`s David and Simon to our home who represent the Anderton Boat Lift, one of the seven Wonders of the Waterways.”

“It was very interesting learning about this unique piece of our living heritage, a 150-year-old structure that was the world’s first major commercial boat lift and currently transports around 3,000 boats a year between the Trent and Mersey Canal and the River Weaver Navigation some 50 feet below.
“Without the lift, boaters would be forced to make long detours. Our residents really engaged with the talk. Resident Jean Nield was able to add her knowledge of our town and the rivers, which impressed our guest speakers, while another resident, Peter Wilkinson, is a keen history buff who used to attend historical talks with his family, so this was an especially positive activity for him.”
“Other residents really enjoyed it, and there have been requests for a trip out to witness the Anderton Boat Lift in person. There was plenty of interaction and questions asked, it was a brilliant morning and everyone learnt a lot.”

A staggering new global survey of care workers reveals a deepening staffing crisis in the health and care sectors, with nearly 70% of workers frequently understaffed and over a third (36.4%) saying they are always working short-handed.
Released on the fifth anniversary of the W.H.O.’s COVID-19 pandemic declaration, the UNI Global Union report—based on responses from 11,233 workers across 63 countries—exposes a care system still in freefall.
Despite being hailed as heroes, care workers face chronic understaffing, poverty wages, and surging workplace violence, driving many out of the profession and leaving patients at risk.
Workers without union protections are affected by this trend even more intensely. The same failures that cost tens of thousands of lives during the pandemic remain dangerously ignored.
UNI warns that these conditions are driving workers away from the sector, exacerbating a crisis that governments and employers have failed to address. The survey shows that union membership and collective bargaining significantly improve worker retention and satisfaction.
Safe staffing levels are essential for high-quality care and safer work environments, but chronic shortages in hospitals and care homes undermine patient health – even causing preventable deaths. For care workers, understaffing leads to poor morale, increased workplace violence and injury rates, and high turnover.
“Five years after the pandemic, care workers are still being overworked, underpaid and exposed to dangerous conditions,” said Christy Hoffman, General Secretary of UNI Global Union. “This report is a wakeup call. Without immediate action to raise wages, improve staffing levels, and combat workplace violence, care systems will collapse.”
Increased public funding for the care sector to ensure quality services, fair pay and a workforce that can meet growing demands.
“There is no shortage of care workers—there is a shortage of care workers willing to endure low pay, chronic understaffing and unsafe conditions,” said Alan Sable, Head of Care for UNI Global Union. “The care staffing crisis cannot be solved simply by training new workers or recruiting migrant care workers. Unless we address the core issues

driving people out of the sector—low wages, understaffing and widespread violence and harassment—the cycle of worker shortages and declining care quality will continue.”
UNI Global Union is calling on governments and employers to act now with the following urgent reforms:
• Higher wages and better benefits to make care jobs sustainable and retain workers.
• Mandatory safe staffing levels to prevent burnout and protect patient care.
• Stronger protections against workplace violence and harassment, including ratification and enforcement of ILO Convention 190.
• Fair treatment and legal protections for migrant workers, who face disproportionate discrimination and unsafe conditions.
• Support for union representation and collective bargaining, which improve working conditions and job sustainability.
• Increased public funding for the care sector to ensure quality services, fair pay and a workforce that can meet growing demands.
WORKER TESTIMONIES: “WE’RE FAILING—AND NO ONE CARES”
Real-life accounts from frontline workers expose the human toll of this crisis:
United Kingdom ( Hospital worker) “People being bullied and people being racist in our department, and it’s always brushed under the carpet, and I believe this is done because we are so short-staffed.”
New Zeland (Caregiver, Aged Care Facility) – “I was sexually assaulted twice by a resident because I wasn’t listened to or protected by my manager or my work colleagues. That occurred because of being short staffed and I ended up having to provide care to the person who sexually assaulted me a year prior.”
Kenya (Hospital Nurse) – “It should not be like this. Working with so little equipment, resources, drugs and with such high expectations in the populace. We’re failing, badly. And the government doesn’t care.”
Canada (Aged Care Worker) – “Every government has promised to make Healthcare a priority, that definitely has not happened. I had hoped that after the horrible living conditions shown during covid in long term care that things would improve. They have not other than the extra paperwork and political bullshit. I want to see us just take care of these people. We need the staff and support to do that!”
Austria (Nurse, Aged Care Facility) – “I was really looking forward to this job. But reality caught up with me very quickly. I’m shocked at what the government/country has done with the healthcare system. Everyone has said that a massive wave of pensions is coming, but fewer and fewer people have been trained. I now know 8 colleagues who have given up the nursing profession (these colleagues had too much heart and passion for this profession, and that was their downfall).”
United Kingdom ( Health care assistant) “I get paid £1 more than minimum wage to be assaulted daily. The level of staff turnover is so high they struggle to replace them.”
UNI Global Union said its report makes one thing clear: “Without urgent action, care systems – already strained by an aging population and still under threat from another pandemic – will crumble, and lives will be lost. The COVID-19 pandemic exposed deep, structural failures in healthcare—failures that led to tens of thousands of preventable deaths. Five years later, those failures remain dangerously ignored.”
Staff and residents at Mallard Court care home in Bridlington have invited neighbours and friends from the local community to their free monthly cancer support coffee morning.
Members of the café spoke candidly about their experiences of cancer and how it touched them, Patricia a resident at the home said “I lost my Mum to cancer when she was 50 years old, it was no age to lose your Mum, from there I became a Macmillan volunteer at Bridlington and also Scarborough hospital offering support to others, it’s so important that people realize support is out there”
Betty another resident has endured skin cancer 3 times and said “it’s so important to accept help and support and to never suffer on your own”
Taking place every first Thursday of the month from 10.30am – 12.30pm, residents from within the local community will have a chance to meet and chat over tea or coffee and homemade cakes provided by the home. Guests will also have a chance to take a tour of the home, and ask any questions they might have about care.
General Manager of the home, Ange Dooley- Widd said: “Our Cancer Support Coffee Morning allows individuals from the local area to meet and connect with one another regularly. It’s a great chance to share stories, make new friends, and of course, enjoy our wonderful spread provided by our hos pitality team!”

The foundation of exceptional care home service lies in collaboration, efficiency, and reliability. For over a decade, Care Quality Pharmacy (CQP) has stood as a trusted partner for care homes across England, Scotland, and Wales. With a specialised approach to care home pharmacy services, CQP ensures residents receive timely and accurate medication, allowing carers to focus on what truly matters: quality time with their residents.
One of the most significant challenges for care homes is navigating missing or out-of-stock medications. CQP’s proactive system addresses this with precision. Their team checks prescriptions, liaises with GP services on behalf of the care home, and resolves discrepancies swiftly. Additionally, CQP’s access to national wholesale suppliers and long-standing relationships ensures a robust strategy for managing short supply issues, keeping residents’ needs a top priority.
Medication errors, often a stress point for staff, are almost eliminated thanks to CQP’s cutting-edge systems. Medications are picked using robotic technology, followed by a meticulous two-stage accuracy check by a pharmacist. This stringent robotic process has achieved an impressive error rate of less than two parts per million. Furthermore, integrations with market leading eMAR providers and coloured paper MAR entries are handled by CQP, reducing the administrative burden for care home teams.

Timely delivery is another hallmark of CQP’s service. Monthly deliveries are scheduled up to six days in advance, and their teams ensure precision and dependability making the booking-in process hassle free. For urgent needs, a 4pm interim cut-off guarantees next-day delivery, including Saturdays. CQP’s commitment to care extends beyond medication. Their open communication lines, available seven
days a week, foster seamless interactions. Moreover, their Quality Assurance Team conducts annual face-to-face compliance audits, enhancing regulatory compliance and resident satisfaction. Added services, such as guidance on covert medicine administration and homely remedies advice, showcase their dedication to meeting every need.
Leading national care home partners trust CQP completely to manage pharmacy services across their entire estates. This unwavering confidence is a testament to the expertise, efficiency, and reliability that CQP brings to the table. Care homes also benefit from no-cost residential returns collection and free online medication training sessions. CQP supports staff development, ensuring a high standard of care using the CQP systems and processes.
By embracing the ethos of collaborative working, Care Quality Pharmacy sets the benchmark for care home pharmacy services. Their efficiency, responsiveness, and focus on compliance empower care homes to achieve the best outcomes for their residents. In an ever-demanding sector, CQP remains a steadfast partner, proving that the right support makes all the difference.
NHS prescription item dispensing data from October 2024 shows CQP to be the
pharmacy in England and therefore possibly making it the largest independent
, online at cqpharmacy.co.uk/care or by contacting the National Partnerships
National care home only pharmacy operating since 2011, based in the Midlands – serving England, Scotland and Wales.
Missing medication? Our team checks all your prescriptions for you and informs you of missing medication - huge time and cost saving to the home, freeing up your quality time with your residents.
Out of stock medication? We manage the entire short supply and out-of-stock medication process. Medication errors? Our resident order is picked by robots, then a 2 – stage independent accuracy check by pharmacists ensures you have the right medicine, on time, every time.
eMAR Integrations - Our systems work alongside all major eMAR providers
Are your deliveries on time? Our monthly deliveries are up to 6 days in advance, giving you plenty of time to book in medication. Saturday deliveries included.
Open Communication - One direct communications team, answering calls & responding to emails giving you one SLA for all of your homes.
Compliance - Quality Assurance Team – guaranteed face-to-face annual compliance audits. Consistency of service and delivery with audit trail.
We are Specialists in care home only dispensingDouble labels, Covert administration and Homely remedies advice.
Free Residential Returns Residential home’s returns are collected – no cost implications to you.
Free Medication Training – Both online and face-toface options available.
Become part of the care home pharmacy delivering excellence in medication management across the country.
References available on request.
To organise an introductory meeting please contact National Partnerships Director, Patrick Bell: Email: patrick@cqpharmacy.co.uk
As 2025 gets into full swing, the social care sector finds itself grappling with the lingering challenges of a difficult 2024.
In response, Log my Care, the intuitive care management platform, has launched Shaping Social Care 2025, a new e-book full of expert perspectives and strategies to support the sector. This article by Mark Topps is an extract from the report, which features six additional chapters of predictions and advice from leading experts covering topics across legal, CQC, HR, complex care, and technology.
When discussing efficiency, we often focus on time savings, which shifts our attention from evaluating existing processes. Additionally, we must consider our teams and those we support, balancing efficiency with quality. Here are practical strategies to achieve both.
ADMINISTRATION AND EVALUATIONS
A large part of social care involves administration, making it an ideal area for streamlining. However, social care often lags in adopting digital tools and AI. While technology isn’t a cure-all, it’s an accessible way to improve workflows without hefty costs.
Many providers already use Digital Care Planning systems, but are these systems being fully utilised? Often, key features are disabled during setup, integrations face challenges, and tools go unused due to limited training. Revisiting these systems and addressing gaps can unlock untapped efficiencies. Proper training can save time, reduce manual work, and allow teams to focus on high-quality care. Here are some strategies and tools to enhance efficiency:
● Digital Care Planning and EHR Integration: Integrating Digital Care Planning systems with electronic health records (EHRs) ensures quick access to essential information, improves accuracy, and reduces time spent on communication with healthcare professionals.
● Digital Rostering: Tools like Log my Care’s Rostering add-on simplify rota creation, optimise staff deployment, and align carers with service users’ needs, improving both efficiency and care quality.
● Process Mapping: Visualise workflows to identify inefficiencies and bot-

tlenecks. Regular updates ensure relevance and provide clarity for teams.
● Simplify Workflows: Eliminate redundant tasks and combine actions where possible. Streamlined workflows save time and reduce errors. These strategies help create efficient systems, allowing more focus on delivering quality care.
Time management is crucial for productivity and quality care. Investing in training and development can significantly enhance efficiency. Consider the following:
● Time Management Training: Tools like the Eisenhower Matrix help staff prioritise tasks based on urgency and importance, ensuring critical items are addressed promptly.
● Goal-Setting and Task Management: Training staff to set realistic goals, break projects into manageable steps, and establish achievable deadlines fosters accomplishment and reduces burnout.
● Continuous Learning: Encourage staff to stay updated on best practices and emerging technologies. This keeps teams engaged, skilled, and ready for challenges.
● System Reviews and Innovations: Regularly evaluate current systems and explore new technologies to identify tools that enhance both efficiency and care quality.
Investing in these areas builds a proactive, capable team ready to meet the demands of modern social care.
While most claim to deliver person-centred care, it’s worth reflecting on whether unique needs are genuinely met. Consider the following:
● Reflect on Care Delivery: Imagine care without constraints like cost or staffing—what would you change? Use these insights to identify actionable steps, such as adopting new technology, reviewing care plans more frequently, or increasing staffing levels.
● Feedback Utilisation: Evaluate how feedback is gathered, analysed,
and acted upon. Effective systems not only highlight improvements but also show service users and staff their input is valued.
● Rethink Staffing Ratios and Rostering: Analyse staffing data to identify needs and explore different shift patterns or task-sharing opportunities. Involving staff in this process can lead to innovative solutions that enhance care and efficiency.
By reflecting, gathering feedback, and actively involving your team, you build a foundation for continuous improvement.
TEAM COLLABORATION AND COMMUNICATION
Streamlining communication is critical for operational efficiency:
● Consolidate Communication Tools: Using multiple systems can cause confusion and duplication. Centralising tools enhances coordination and reduces administrative burdens.
● Optimise Meetings: Regular, focused meetings with clear objectives are more effective than broad, infrequent gatherings. Purpose-specific meetings foster engagement and clarity.
● Collaborative Culture: Streamlined communication and purposeful meetings build trust and morale, empowering teams to work together effectively. This enhances processes and ensures exceptional personcentred care.
Efficiency in social care goes beyond saving time—it’s about maximising resources, eliminating unnecessary tasks, and streamlining processes.
The ultimate goal is improving outcomes for the people we support. By fostering collaboration, leveraging technology, and focusing on quality, we can create a system that balances efficiency and care excellence.
Scan the QR code to read the full ebook for free

North west businessman and philanthropist Sir Norman Stoller has praised the ‘amazing’ veteran care village where a wing is named in his honour.
The Stoller Charitable Trust donated £4m towards the £12.5m redevelopment of Broughton House Veteran Care Village in Salford, which was completed in 2022.
Broughton House has cared for more than 8,000 veterans since it opened its doors to the ex-service community in 1916.
Following its redevelopment, it is now a complex with a 64-bed care home, including two 16-bed households dedicated to veterans with dementia, as well as independent living apartments.
The home also has an Armed Forces Support Hub, which provides support for elderly and working age veterans living in the community.
Sir Norman toured Broughton House with Stephen Lowe, the charita-
ble trust’s project manager. The duo were shown round by the care home’s chief executive Karen Miller, trustee and former RAF fighter pilot Peter Curtis, and head of nursing Lore Popa.
Karen said: “The Stoller Charitable Trust’s generosity was instrumental in helping our charity realise our vision to create the wonderful facilities we have today. The trust has ensured we can continue to care and support veterans and their families for many years to come.
“Sir Norman was delighted to see the new Broughton House, and he was especially pleased to see first-hand the modern, comfortable and caring environment.
“He commented on how amazing the home is, and was pleased to see how his financial support has positively impacted the lives of so many veterans and their families and will continue to do so. We are forever grateful.”
Residents from The Haven care home in Boston enjoyed a fantastic time at Boston United’s last home game against Woking. Staff accompanied 4 residents from the home on Whitehouse Lane in Boston to enjoy the game on a sunny afternoon, which finished in a 2-2 draw thanks to a last-minute equaliser from Boston. The residents and staff watched the game from the comfort and luxury of an executive box, graciously loaned from Acorn Taxis. The residents and staff enjoyed a wonderful lunch and hospitality from the team at the club and received a matchday programme and lanyard to remember the day.
Philip Stocker, a resident at The Haven since October 2023 is a regular attendee of the Pilgrims’ games. He proudly wore his scarf and met his grandson at the game and an old friend who he hadn’t seen for many years.

Jean Stephenson who has lived at the home since September 2023 bumped into a relative at the game and at the age of 87 it was her first football match. Afterwards she spoke to her brother who lives in New Zealand who couldn’t believe she’d been to the game.
Freda Brown and Valerie Duck also had a wonderful time, cheering on the team and met old friends, spending time chatting and reminiscing.
Evangeline Girling, manager at The Haven thanked all those involved. “We’re always trying to try different things to do with our residents and to build long-standing relationships with our local community. We all had a brilliant time and would like to thank Mick Small, Sandra and Paul Richmond, who carry out all the fundraising for the club and to Bev Jenkins, our Activities Co-ordinator from The Haven for organising the afternoon.”

Avery Healthcare has once again been recognised as one of the top care home providers in the UK, securing its place in the prestigious Top 20 Large Care Home Groups at the 2025 Carehome.co.uk Awards.
The Carehome.co.uk Awards are a significant recognition in the care sector, celebrating the best care providers across the UK.
These awards are based on genuine reviews and feedback from residents and their families, making them a valuable measure of the quality of care offered.
Carehome.co.uk is the UK’s leading online directory for care homes, providing a platform where families and individuals can find information and reviews to help them choose the right care provider.
This year, over 2,117 care home groups were evaluated, making Avery’s ranking in the Top 20 an outstanding accomplishment.
Avery Healthcare operates 102 care homes and four retirement communities across the UK, offering a wide range of care services including respite, residential, and dementia care across all its homes.
Many of these locations also offer nursing care, ensuring that residents receive the most appropriate support for their needs.

This award reflects Avery’s dedication to providing exceptional care, state-ofthe-art facilities, and a person-centred approach, ensuring the highest quality of life for its residents.
Founded in 2005, Avery Healthcare has grown significantly, always focusing on tailored care solutions that meet the diverse needs of its residents.
Sadie Deveraux, Director of Communications and Marketing at Avery Healthcare, said,
“We are incredibly proud to be recognised once again as one of the UK’s top care home groups. This award is especially meaningful because it is based on feedback from residents and their families, reflecting the dedication of our teams in delivering outstanding, person-centred care.”
“At Avery, we are committed to providing not only the highest standards of care but also a warm and welcoming environment where residents truly feel at home.”
Amanda Hopkins, Reviews Manager of Carehome.co.uk, said,
“It is a huge achievement to be named as a Top 20 care home group by the residents and their families, who have experienced for themselves the quality of care and support given at the care home.
“We would like to congratulate Avery Healthcare on being a top care home group! Our awards, celebrate the excellent care given by care home groups and show Avery Healthcare gives first-rate care throughout its homes.
“These top performing care home groups are making a profound difference to residents’ lives, by putting compassion, respect and dignity at the centre of their care.”
Residents at Paternoster House care home in Waltham Abbey experienced a special literary treat when students from Upshire Primary Foundation School paid them a visit to celebrate World Book Day. Led by Headteacher Mr Jones, the young visitors arrived in colourful costumes representing their favourite literary characters—from Ghostbusters and witches to Maze Runner, Dog Man, and Charlie from Charlie and the Chocolate Factory!
The excited young readers spent quality time with residents throughout the home, visiting all communities and talking to residents in their rooms and communal areas. They spoke about their favourite books and updated everyone on the characters, authors, and their joy of reading.
“Our residents all love to read or be read to,” said Activities Coordinators Cathy and Angie. “Celebrating World Book Day alongside

the Upshire school children created a wonderful opportunity for intergenerational connections through our shared love of books.”
Corina Popescu, General Manager at Paternoster House, added: “It was wonderful to see the children’s excitement as they brought their favourite stories to life chatting to our residents and guests.”
Before departing, each child received a chocolate treat to say thank you for visiting and Mr Jones was presented with several books specially designed by Barchester Healthcare in collaboration with the Alzheimer’s Society, including “Visiting Gran” and “Grandad’s New Home” by Virginia Ironside—resources created to help children understand dementia.
The event highlighted the power of books to bridge generational gaps and create valuable community connections.

The care sector is no stranger to challenges. With an aging population, increasing demand for services, and financial pressures, care providers are constantly battling to stay ahead. Add to this the need for positive public perception in a media environment often fixated on crises, and it’s clear that strong communication isn’t just a nice-tohave—it’s essential. That’s where DAPS Agency Ltd comes in, a specialist communications agency helping care organizations navigate these turbulent waters and emerge stronger.
DAPS Agency is no ordinary PR outfit. Founded by seasoned communications professionals Anneli Lort and Firgas Esack, the agency has carved out a niche for itself by understanding the unique hurdles faced by care providers, from technology innovators to care home operators.
“The care sector is about more than delivering services; it’s about creating meaningful experiences for residents, building trust with families, and supporting staff,” says Anneli Lort, co-founder of DAPS. “But these stories often get buried under the day-to-day pressures providers face.”
One of the biggest hurdles for care organizations, whether they’re home groups or care technology suppliers, is visibility. With so many competing voices in the sector, standing out is no easy feat. Providers need to balance the operational challenges of driving occupancy and adapting to new technologies while maintaining strong relationships with stakeholders. According to Firgas Esack, this is where targeted and tailored communications can make all the difference.
“Visibility is critical,” Esack explains. “We help care providers showcase their unique strengths, whether it’s innovative resident care programs or cutting-edge technology that’s changing how the sector operates. Our aim is to make sure their voices are heard where it matters most.”
PUTTING CARE PROVIDERS IN THE SPOTLIGHT
DAPS excels at elevating their clients’ profiles by crafting narratives that resonate. Whether it’s securing positive press coverage or positioning an organization as a thought leader through white papers and industry commentary, the agency’s strategies are rooted in authenticity.
“Care home groups face enormous pressures to attract and retain residents while maintaining financial sustainability,” says Esack. “We’ve worked with clients to highlight innovative approaches they’ve taken to deliver high-quality care on a budget, securing media coverage that positions them as forward-thinking leaders.”
The team’s expertise isn’t limited to traditional care providers. In an industry increasingly driven by technology, DAPS has also helped care tech companies gain recognition for their solutions. From illustrating how a software tool is transforming care home operations to showcasing new assistive technologies that improve residents’ quality of life, DAPS knows how to translate technical innovation into stories that matter. TACKLING THE TOUGHEST ISSUES
The care sector is not without its share of crises—media scrutiny, financial difficulties, and regulatory challenges can arise at any moment. This is where DAPS’ experience in crisis communications comes into play. Having run global press offices and handled high-stakes issues for clients, the agency offers a steady hand when it’s needed most.
“When a crisis hits, it’s easy to feel overwhelmed,” says Lort. “Our role is to step in, take control, and guide our clients through the storm while safeguarding their reputation.”
Their work doesn’t just stop at damage control. Proactive thought leadership—opinion pieces, keynote speeches, and lobbying efforts—ensures that their clients are shaping the narrative, rather than simply reacting to it. By working closely with stakeholders, DAPS ensures that their clients’ voices are heard at both local and national levels.
What sets DAPS apart is its unashamedly remote working model. Lort and Esack believe this approach allows them to deliver exceptional results without the traditional overheads of a bricks-and-mortar agency.
“Every penny our clients spend goes toward achieving results,” says Lort. “And because our team is made up of senior professionals, clients know they’re always working with experts who understand the complexities of their sector.”
This lean, results-driven ethos has helped DAPS build a reputation as a trusted partner for care organizations of all sizes. Whether working with a large care home group or a niche technology provider, the agency’s approach is the same: tailored, proactive, and relentlessly focused on outcomes.
One of the most rewarding aspects of DAPS’ work is celebrating the positive stories that come out of the care sector. In an industry that’s often under scrutiny, shining a light on success stories is vital.
“Whether it’s a care home running an innovative intergenerational program or a technology provider making a measurable difference in residents’ lives, we make sure these stories get the attention they deserve,” says Esack. “We want to celebrate the people and innovations driving the sector forward.”
This focus on positivity isn’t just good PR; it’s also good for morale. Recognizing and sharing achievements boosts confidence within organizations and strengthens their reputation with external stakeholders.
As the care sector continues to evolve, the need for strategic, impactful communications will only grow. For care providers looking to amplify their voice, tackle challenges head-on, and secure their place as leaders in the sector, DAPS Agency offers the expertise and passion to make it happen.
“We’re here to tell the stories that matter,” says Lort. “The care sector does incredible work, often under tough circumstances, and it’s our job to make sure that work is seen, understood, and celebrated.”
In a sector where the stakes couldn’t be higher, DAPS is proving that the right communications partner can be transformative. Whether navigating a crisis, celebrating a success, or shaping the future of care, this dynamic agency is helping its clients rise to the occasion.
To book a free, no-obligation one hour consultation with DAPS to discuss your communications challenges and needs, go to daps.life/DAPS60 www.dapsagency.com
Hospice UK has welcomed the announcement of the allocation of the first £25m of additional government funding for the hospice sector in England, following the announcement late last year of an £100m funding package.
Toby Porter, CEO of Hospice UK, said: “The announcement before Christmas of £100m of additional funding for hospices in England was a significant boost, and today’s news of the allocation of the first £25m of this funding will be a huge relief for our members.
“Several years of rapidly rising costs have curtailed the extent to which hospices have been able to investin their infrastructure for the longer term. This additional support will enable them to do so – and relieve the immediate pressures on hospice finances.
“The hospice sector is ready to support the government’s ambition to shift more care into the community. This couldn’t be more important for people approaching the end of life, when it’s vital to have the right care, in the right place.
“The greater stability provided by the government’s funding injection this year and next gives us a golden opportunity to now reform the palliative and end of life care system, so it’s fit for the future.”
The initial £25m funding, which is being distributed via Hospice UK to eligible hospices this financial year (2024-5), will be followed by a further £75m next financial year (2025-6).
The capital funding is designed to help hospices improve their physical environment, improve efficiency by investing in digital technology, and increase hospices’ capacity to care for patients at home. The funds will help alleviate significant budget pressures in the sector.
Paul Bytheway, Chief Executive of Birmingham
Hospice, said: “This additional funding is a boost after a very challenging year for Birmingham Hospice. We appreciate the government’s acknowledgement of the significant operating pressures the hospice sector has been under, and we welcome any investment that helps us to continue delivering services to those in our communities who need it most.”
Elinor Eustace, CEO of St Giles Hospice, in Lichfield, Staffordshire said:
“We are incredibly grateful for this vital funding from the government, which comes at a crucial time for St Giles Hospice. This support will enable us to make meaningful improvements to our Inpatient Unit, enhancing the experience for patients and their families during what can be an incredibly difficult time. From upgrading patient facilities to improving our family spaces, this investment will help ensure we can continue providing the highest quality endof-life care for our local community.”
“While this immediate funding is essential and deeply appreciated, we remain focused on working with partners to develop sustainable long-term solutions for hospice care funding. Every pound invested in hospice care makes a real difference to families across our region when they need us most.”
Lisa Hunt, Chief Executive of Garden House Hospice Care in Letchworth, Hertfordshire, said:
“Our costs have been increasing significantly in recent years as we grow our services to address the inequalities in accessing palliative care.”
“The acknowledgement of this pressure from the government is welcome and will make a real difference – helping us achieve our goal to keep patients out of hospital. We are eager to continue supporting the government’s mission to move more care into the community.”












New analysis has backed up government proposals for the creation of new unitary councils in England – but new authorities must cover areas of ‘at least’ 500,000 people or more in order to save billions and free up investment into local services.
In December, the government’s English Devolution White Paper outlined plans for a radical overhaul of council structures, with government committing to end ‘two-tier’ local government, replacing 185 county and district councils with new unitary authorities in 21 areas.
Ministers have set out new unitary councils should have a population of 500,000 or more. However, they have also suggested ‘flexibility’ on this number, with district councils across the country subsequently proposing new councils with populations of 300,000 or lower.
The County Councils Network’s (CCN) new report, which draws on new data produced by PwC, reveals that replacing the two-tier system with a new wave of councils with minimum populations of 500,000 could save at least £1.8bn over five years.
However, the CCN report also shows those savings from reorganisation reduce dramatically if county and district authorities are replaced with multiple smaller councils – potentially costing local taxpayers hundreds of millions.
The analysis shows that splitting two-tier areas into 58 new unitary authorities based on a minimum population of 300,000 would cost £850m over five years and deliver no savings.
This is because the greater the number of new unitary councils and the smaller the size, the more costs are incurred from ‘disaggregation’ – the process of splitting up and duplicating county council social care services into multiple new authorities – alongside higher one-off transition costs and lower long-term efficiency savings.
CCN say the analysis backs up the government decision to include
the minimum half a million benchmark, with the figures showing an ‘unsustainable’ increase in the costs of reorganisation from creating dozens more unitary authorities below this population mark.
But with the Local Government Minister Jim McMahon recently indicating proposals for unitary councils below the 500,000 population number could still be acceptable, CCN is warning that it is ‘absolutely essential’ the government now stick to the 500,000 minimum population threshold while ensuring no upper limit on the size of new councils.
The network says that failure to do so will mean the government fall short in their promise to end the ‘two-tier’ financial premium and create ‘billions’ in efficiency savings, while creating hundreds of millions of new costs for care services.
Using this data and applying different population thresholds for new unitary councils to each of the two-tier areas in England, CCN’s new report reveals:
• Replacing the two-tier system in England with 58 new unitary authorities based on a minimum population of 300,000 would cost local taxpayers £850m over five years.
• Under this scenario no long-term efficiency savings would be delivered, meaning it would be more efficient to retain the current two-tier system in England.
• This is because creating unitary authorities of this size would result hundreds of millions in additional costs each and every year from splitting up social care services into multiple smaller councils. The annual recurring cost of disaggregation could reach over half a billion pounds, while the ‘one-off’ transition costs would cost over £660m.
• In contrast, creating 29 new unitary councils based on a minimum population of 500,000 would save £1.8bn over five years, and an annual saving of £500m thereafter. This is because annual disaggregation
costs reduce dramatically by almost three quarters (73%), while one-off transition costs are 28% lower.
• The level of savings increase further if a minimum population threshold of 600,000 was applied, resulting in a net-saving of £2bn over five years from creating 27 unitary councils. The savings increase further if all 21 two-tier areas were replaced with single unitary councils, with a net-saving of £2.9bn over five years.
Cllr Tim Oliver, Chairman of the County Councils Network, said: “Today’s new analysis by the County Councils Network (CCN) shows local government reorganisation could unlock billions in efficiency savings to be reinvested in frontline services. But it can only do this if new councils have populations of at least of 500,000 or more.”
“While it may be necessary for some areas to create more than one new council, this analysis shows that splitting county councils into multiple small unitary councils with populations as small as 300,000 will create hundreds of millions of new unsustainable costs, piling further strain on already under pressure care services.”
“It is absolutely essential that the government now stick to the statutory criteria they have set out, treating the 500,000 as a minimum not an optimum population scale. This will ensure we create new councils with the scale and capacity to deliver substantial savings to be reinvested in frontline services to the benefit of local taxpayers. Failure to do so could mean the government fall short in their promise to end the ‘two-tier’ financial premium.”
“CCN are not being dogmatic over whether an area chooses to reform into one or more unitary authority. It is ultimately up to local areas to choose which option to pursue, considering both the financial implications and other impact factors. However, they must do so mindful of the costs and risks involved in the reorganisation process.”
Since 2022, Carlton Court has been proudly partnering with Hertfordshire University to provide nursing students with an enriching six-week placement in community care. This collaboration offers students a unique opportunity to engage with residents, build meaningful relationships, and gain hands-on experience in delivering compassionate, person-centred care. During their placement, students from the university's nursing degree program learn how to connect with residents and provide empathetic care in a supportive environment. Through these interactions, students develop essential communication and interpersonal skills, creating a solid foundation for their future careers in healthcare.
One of the key aspects of the placement is the opportunity to explore the differences between hospital-based care and community nursing. Students witness firsthand the challenges faced by community nurses, managing diverse residents’ needs in a less structured environment. They gain invaluable experience caring for residents with different types of dementia, learning to tailor care plans to meet

the specific needs of each individual. This exposure enhances their understanding of dementia care, builds their clinical skills, and helps them confidently manage complex, long-term conditions.
The placement also encourages students to think critically and grow in leadership. By assessing residents’ needs, making informed decisions, and taking initiative, students improve their clinical judgment and their ability to collaborate effectively with multidisciplinary teams.
This partnership not only benefits the nursing students but also enhances the work environment at Carlton Court. Team members are encouraged to reflect on their own practices and benefit from training sessions offered by the university, covering the latest care techniques and research.
Ultimately, the collaboration strengthens the quality of care at Carlton Court while providing students with the tools they need to become skilled and compassionate nurses, ensuring the future of high-quality care in the community.

WHAT’S ON THE AGENDA?
UK Care Week is an event exclusively for care professionals, designed to empower and equip you with the skills to enhance the lives of those in care. This event provides a vital platform to explore industry-leading content, innovative solutions, and hands-on product demonstrations.
With 100+ CPD-accredited sessions, innovative products from 150+ top suppliers, and tailored guidance at the CQC Inspector Hub, you’ll find resources to meet the highest standards. Dive into interactive features like the Virtual Dementia Tour and expert-led training to elevate care.
The event features an impressive lineup of sessions, workshops, and opportunities to engage with the latest developments in the care sector. Key highlights include: THE CARING VIEW THEATRE
Hosted by the passionate team behind the Caring View Podcast, this theatre promises engaging discussions and insights into the latest care practices and strategies.
Meet over 150 exhibitors showcasing solutions designed to stimulate business growth and help implement sustainable care models. Discover cutting-edge technologies and practical tools to elevate your care services.
Attend interactive seminars hosted by industry experts. These sessions tackle real-world challenges in
care settings and offer actionable solutions to overcome them. Gain up to 12 CPD points across 2 days.
CQC INSPECTOR HUB
Book a 1-2-1 meeting with a CQC Inspector to discuss any queries you may have; local inspectors will be able to answer any queries, as well as dealing with registration advice.
CO-LOCATED EVENTS
Gain access to additional CPD sessions and resources through co-located events, including The Alzheimer’s & Dementia Show, Neuro Convention, and Naidex. These events create a collaborative environment that unites aspects of health, social care, rehabilitation, inclusion, and diversity.
EXCLUSIVE TRAINING OPPORTUNITIES
In partnership with Training2Care, co-located event The Alzheimer’s & Dementia Show offers unique experiential training sessions tailored to dementia care:
• Virtual Dementia Tour: £60 + VAT per session
• Dementia Interpreters Workshop: £45 + VAT per session
• DIET, Dining Immersive Experiential Training: £60 + VAT per session
• Autism Reality Experience: £60 + VAT per session
Spaces for these sessions are limited, so early booking is highly recommended. Uk Care Week visitors can book onto these sessions via the Alzheimer’s & Dementia Show website - www.alzheimersshow.co.uk/training DON’T MISS OUT! Join us at UK Care Week 2025 and take part in this essential gathering of care professionals. Connect with experts, explore innovative solutions, and access tools to drive care excellence. Register for your free ticket today

New survey insights reveal the far-reaching impact caregiving can have on physical and mental well-being, with over half (54%) of caregivers reporting weekly back, joint or muscle pain, and 1 in 5 (19%) experiencing daily stress or anxiety.[i] Dr Dawn Harper shares her tips to help cope.
There are approximately 4.7 million unpaid carers in the UK,[ii] defined as those who provide unpaid care for someone who is ill, disabled, older, has mental health issues or struggles with addiction. However, this figure excludes the many who regularly care for children, neighbours or friends and family needing support beyond the traditional definitions. Carers UK estimates that the number of unpaid carers could be as high as 10.6 million, highlighting a significant lack of personal and societal recognition of what it truly means to provide care.[iii]
A new survey, commissioned by GOPO® Joint Health – a leading supplement proven to reduce pain and stiffness and improve mobility – polled 1,001 self-defined caregivers. The findings reveal the true impact of caregiving on mental, emotional and physical health. Over one-third (37%) have experienced significant strain, discomfort or injury to their joints as a result of assisting or lifting the person they care for, and almost half (47%) frequently endure persistent aches, stiffness or pain that lingers long after caregiving tasks.i As a result, one-third (32%) rely heavily on pain medication, putting their own long-term health at risk.

The mental toll of caregiving is profound, with almost half (46%) of caregivers feeling emotionally drained by the relentless stress it brings. One in seven (13%) rely on support services for their well-being, while nearly half (44%) experience loneliness or isolation at least once a week, often facing the demands of caregiving alone.
Despite these challenges, almost half (49%) of respondents cannot remember the last time they practiced self-care, admitting that their own needs always come last.i While caregivers devote themselves to others, acknowledging the importance of self-care, and setting aside time for their own well-being is vital.
Dr Dawn Harper, formerly a caregiver to her mother, NHS doctor for over 30 years and author of ‘Live Well to 101’, comments: “Caregiving is a labour of love, but the selfless nature of the role puts many caregivers at serious risk of poor health. As a GP I see first-hand the impact that caring can have on both physical and mental ill health. To continue supporting others, it’s vital to care for yourself first. Just like the safety advice on an aeroplane – put on your own oxygen mask before helping others. Prioritising your own wellbeing ensures you have the strength, resilience and capacity to provide the care your loved ones need in the long-term.”
Dr Dawn Harper provides her top tips to support caregivers’ health and well-being: Seek support from peers: “It can be easy to lose your identity when providing care, so it’s important to connect with peers who are in a similar situation. If you are unable to leave the house often, online forums or virtual coffee sessions can provide an outlet to enable you to open up to someone who understands exactly what you’re going through. Their acceptance and understanding can be a great way to support your emotional health and leave you feeling less alone.”
Schedule self-care: “Caregiving often leaves little time for personal well-being, but selfcare isn’t a luxury, it’s a necessity. Schedule self-care just like any essential appointment and if you’re struggling to find the time, start with small manageable breaks of just 5-10 minutes and commit to doing one thing that makes you feel recharged. This could be as simple as having a cup of tea in silence or reading a few chapters of your favourite book.”
Build your mental resilience: “Mental resilience helps caregivers manage stress, maintain emotional balance and continue providing care without burning out. Incorporate techniques such as mindfulness, deep breathing, yoga or meditation, all of which can be practiced in as little as 15 minutes. If you are struggling with your mental health, make sure to reach out to mental health helplines or listening services, or discuss your feelings with your GP or pharmacist.”
Prioritise your physical health: “Caregiving is a physically demanding role, and these survey findings reveal the true toll caregiving can take on your physical health. Protect your joints and posture by using proper lifting techniques when assisting with mobility, and address any aches and pains early to help prevent chronic conditions from appearing later down the line. A joint health supplement such as the galactolipid, GOPO, a compound derived from rose-hip, may be of great benefit, with research indicating that it can effectively relieve joint pain.[iv] The natural anti-inflammatory properties of GOPO make it a viable replacement to pain killers,iv without the risk of harmful side effects, and a sustainable way to manage pain long-term.”
Extensive studies involving over 400 patients with chronic pain conditions, such as osteoarthritis, have shown that GOPO® produces significant and consistent pain relief and improved joint function. In one study, 8 out of 10 patients reported a significant reduction in pain after just 3 weeks of GOPO®.[v]
GOPO® Joint Health is available from Boots, Amazon, and independent chemists and retailers nationwide. Visit www.gopo.co.uk for further information.
[i] GOPO® Joint Health survey on 1,001 caregivers in the UK. January 2025.
[ii] The Kings Fund. 2024. What are unpaid carers, who are they and how often do they provide care? Available at: https://www.kingsfund.org.uk/insight-and-analysis/data-and-charts/unpaid-carersnutshell#:~:text=According%20to%20the%202021%20Census,females%20from%20the%202011%20Census. (Accessed: January 2024).
[iii] Carers UK. 2023. Annual Report 2022-2023. Available at: https://www.carersuk.org/media/ynfpnjwk/carers-uk-annual-report-22_23 (Accessed: January 2025).
[iv] Winther, K et al. “A powder made from seeds and shells of a rose-hip subspecies (Rosa canina) reduces symptoms of knee and hip osteoarthritis: a randomized, double-blind, placebo-controlled clinical trial.” Scandinavian journal of rheumatology vol. 34,4 (2005)
[v] Winther, K et al. “A powder made from seeds and shells of a rose-hip subspecies (Rosa canina) reduces symptoms of knee and hip osteoarthritis: a randomized, double-blind, placebo-controlled clinical trial.” Scandinavian journal of rheumatology vol. 34,4 (2005)
[vi] Rein E, Kharazmi A, Winther K. A herbal remedy, Hyben Vital (stand. Powder of a subspecies of Rosa canina fruits), reduces pain and improves general wellbeing in patients with OA – a double-blind, placebo-controlled, randomised trial. Phytomedicine 2004.
[vii] Christensen R et al. Does the hip powder of Rose canina (rosehip) reduce pain in osteoarthritis patients? – a meta-analysis of randomised controlled trials, Osteoarthritis Cartilage (2008)
[viii] Schwager J, Richard N, Wolfram S. Anti-inflammatory and chondro-protective effects of rosehip powder and its constituent galactolipids GOPO Poster presentation at the World Congress of Osteoarthritis (OARSI) 2008
Representatives from the sports club and care home met for a discussion about sport, opportunities and challenges for women and International Women’s Day Footballers from Launton Ladies visited residents and team members at Langford View care home to present a framed football shirt for their 2024/25 and 2025/26 seasons.
The care home in Bicester, run by The Orders of St John Care Trust (OSJCT), is sponsoring the local team as part of a partnership to promote intergenerational connections between the two organisations.
Claire Finn, who coaches the team, visited the home with footballers Lizzie, Naomi, and Pippa to discuss the importance of women’s sport and how it helps build confidence and empowerment.
Langford View’s Activities Co-ordinator, Terri, shared her experience of playing for Fulham Ladies’ youth team as a teenager. She said: “I was thrilled to join the Fulham Ladies’ youth team. It was a place that took women’s football seriously, unlike

school, which at that time prioritised football for boys.”
Claire said: “We are delighted that OSJCT Langford View is supporting our football club. Enabling sport for women promotes confidence, teamwork, and resilience, helping them take more opportunities and reach for their dreams. More and more, I see women achieving career and personal highlights that would have been unheard of in recent decades.”
Farida Ait-Tales, Home Manager at Langford View, added: “This was a very uplifting conversation. It made me reflect on working in care, where I’ve seen women take opportunities to progress in their careers. We are making some exciting plans for this new partnership with Launton Ladies, including a football charity day in the summer—a wonderful opportunity for our residents, team members, and friends of Langford View to participate in some friendly sporting challenges.”
Taylor & Taylor, a group of family-owned residential care homes approached food procurement experts, allmanhall to achieve scalable cost savings and efficiencies to support their growth plans. They needed to ensure no detrimental impact to the excellent quality of their food offering and their residents’ dining pleasure.
Their desire was to achieve a 5% food cost saving and to ensure ongoing effective management of catering budgets and invoicing. Operationally, access to reports and insights were key, as was ease of ordering and management of stock and deliveries.
allmanhall undertook a like-for-like benchmark and identified achievable food cost savings of 11.4% - more than double the initial objective!
allmanhall delivered tech demos of the catering control platform for Taylor and Taylor, ensuring it met their needs and provided training for the team. As well as providing useful operational functionality like stock taking and standing orders, the catering control platform proposed would also give access to management reports and facilitate central billing and conversion of all supplier invoices in to 1 per month. Samples and on-site supplier meetings were also arranged on behalf of the homes, to confirm that the quality was to the required standard. allmanhall have also supported Taylor and Taylor with the launch of a community engagement event for one of their newest homes.
A few months into the contract, the actual results were found to be an 18% food cost saving! You can watch this short video on You Tube to find out more…
“From day 1, the care and attention provided by allmanhall has been exceptional. The team truly listen to us, to what our challenges are and are always willing to help in any way they can. Their approach is thorough and responsive, meaning we feel fully supported. Everyone we’ve met from allmanhall has been hands-on, down to earth, genuine and considerate.
I’ve been impressed by the savings we’ve already seen, the flexibility regarding suppliers and by the excellent quality. The consolidation of invoices into 1 per month is a huge win.
We have relationships and contact with people across the allmanhall team – all there to help and to advise or resolve depending on what we need. With challenges around labour shortages and food inflation, this is hugely valued. It frees up the team and gives us peace of mind.
I would wholeheartedly recommend allmanhall’s services to others in the care sector and I look forward to continuing to grow our offering and provide outstanding food for our residents, with allmanhall as our trusted partners.”
– Chris Rees, Group Executive Chef allmanhall is an owner-managed, award-winning and trusted food procurement partner for care organisations across the UK. We help clients with a range of needs, including cost savings, administrative efficiencies, supplier management, dietetics and nutrition support, and sustainability goals. Get in touch to find out


The Health and Social Care Committee has appointed five new specialists to its Expert Panel.
The specialists will work alongside the core members of the Expert Panel, chaired by Professor Dame Jane Dacre, as it undertakes an evaluation into the state of palliative care in England.
The Health and Social Care Committee established the Expert Panel to conduct independent evaluations of Government commitments in different areas of healthcare policy and enhance Committee scrutiny of the Government. Each evaluation leads to a published Report.
The five new members are:
• Anita Hayes, Clinical Quality Lead at Hospice UK
• Professor Vic Rayner OBE, Chair at Global Ageing Network and CEO at National Care Forum

• Dr Michael Tatterton, Chief nursing officer at Bluebell Wood Children’s Hospice and Clinical Associate
• Sir David Pearson, and
• Professor Stephen Peckham
Professor at the University of Bradford
• Dr Sam Royston, Executive Director for Research and Policy at Marie Curie UK
• Dr Sabrina Bajwah, Honorary Consultant Palliative Medicine at King’s Health Partners and Clinical Reader at Cicely Saunders Institute
The Expert Panel is chaired by Professor Dame Jane Dacre, Professor of Medical Education at University College London, former Director of the UCL Medical School, a consultant physician and rheumatologist, and a former President of the Royal College of Physicians.
The Panel’s core members are:
• Professor Emma Cave
• Anita Charlesworth CBE
• Sir Robert Francis QC
Care tech leader Sensio are proud to announce a strategic long-term partnership agreement with Lovett Care for their sensor technology RoomMate and digital Nurse Call system to be rolled out across their estate.
Sensio is a leading provider of care technology through pioneering software and products, solving today's and tomorrow's care challenges for the benefit of residents, relatives, care teams and society.
The long-term partnership agreement encompasses a roll out of Sensio’s digital Nurse Call system and the multi-sensor RoomMate and digital supervision to Lovett Care’s portfolio of care homes in 2025. Since Lovett Care acquired New Care in October 2024, the technology will also feature in all New Care facilities too.
RoomMate is a privacy first multi-sensor that alerts care teams when a resident is at risk of a fall and helps ensure staff are available to prevent a fall before it happens. RoomMate also captures valuable activity datat that is fed directly through to care planning software to enrich care plans and drive better quality evidence-based decision making.

The digital Nurse Call system is a wireless, silent nurse call system that transforms care home environments by removing noisy call bells. Sensio Nurse Call sends alerts directly through to care teams handheld devices, enabling teams to triage support to those most in need. Both of these solutions are designed specifically for those living with dementia where traditional forms of alerting are not always
appropriate or workable.
Lisa Delaney, Country Manager Sensio UK, says: “We are very excited to be partnering with Lovett Care and this is an important step for Sensio in the UK. We have really enjoyed working with the team so far and have been impressed by their eagerness to embrace new technology. I look forward to growing our partnership further over the next few months and help Lovett Care to deliver the best care possible for their residents.”
Following a successful pilot which demonstrated a significant reduction in falls, highlighted positive outcomes for residents, and fostered a better working environment for care teams, Lovett Care has made the decision to roll out the technology across its homes.
Keith Crockett, CEO of Lovett Care, commented: “Both Lovett Care and New Care are already leading care home operators in technology advancements, so adopting Sensio’s RoomMate and digital Nurse Call system will further enhance and improve our residents’ experiences. The trial was a success, and RoomMate proved to be highly effective in reducing falls. We’re excited to partner with Sensio to integrate this technology into our homes, further enhancing the safety and support we provide to our residents.”
For further information on Sensio please visit www.sensio.io
To find out more about Lovett Care please visit www.lovettcare.co.uk
If you’re involved in caring for others – whether you’re a care provider, a health and social care professional seeking the latest products and services, a family carer in need of support, or simply someone passionate about care – the Alzheimer’s & Dementia Show is the event for you.
As the UK’s leading dementia event, it offers a unique opportunity to explore a wide range of care exhibitors, hear from expert speakers, and experience innovative training sessions. This event is more than just an exhibition; it’s a platform for learning, discovering solutions, and connecting with people who share a commitment to improving dementia care.
Taking place at the NEC in Birmingham on 19-20 March 2025, the Alzheimer’s and Dementia Show provides a vital space for families, carers and healthcare professionals to access resources and knowledge that can transform the lives of those affected by dementia.
WHAT’S ON THE AGENDA?

The show is packed with insightful sessions designed to address key aspects of dementia care. Discover the latest diagnostic tools and treatment options that are revolutionising early intervention and improving patient outcomes!
CAREGIVER SUPPORT AND EDUCATION
Access practical strategies and resources that empower caregivers to provide compassionate and effective care, ensuring the well-being of those they look after.
DEMENTIA-FRIENDLY ENVIRONMENTS
Learn about innovative designs and technologies that create safer, more comfortable living spaces for individuals living with dementia.
WHY ATTEND?
For those seeking specialised training, the show offers sessions delivered by Training2Care. These experiential programs provide actionable insights tailored to dementia care. Sessions include: Virtual Dementia Tour: £60 + VAT per session Dementia Interpreters Workshop: £45 +
• Autism Reality Experience: £60 + VAT per session
Spaces are limited, so early booking is highly recommended. Book your space here - www.alzheimersshow.co.uk/training.
EXPERT-LED SESSIONS
Gain insights from top researchers, clinicians, and advocates. Key speakers include:
• Prof Fiona Ducotterd "Putting tools in the toolbox to treat dementia." Chief Scientific Officer, Alzheimer’s Research UK, UCL Drug Discovery Institute
• Hannah Gardner "Supporting children and young people living within families affected by dementia." Consultant Admiral Nurse for Children and Young People, Dementia UK
• Prof Nathan Davies "Supporting people living with dementia through to end of life" Professor of Ageing, Applied Health and Care Research, Colead Centre for Psychiatry and Mental Health, Queen Mary University of London 1-TO-1 DEMENTIA CLINICS WITH ADMIRAL NURSES
For personalized advice and support, visit Dementia UK’s Admiral Nurses. These 1-to-1 clinics provide tailored guidance to address your specific questions and concerns.
NETWORKING OPPORTUNITIES
Connect with a diverse community of caregivers, healthcare professionals, and innovators. Share experiences, exchange ideas, and build valuable relationships within the dementia care sector.
EXHIBITOR HIGHLIGHTS
Explore an extensive range of exhibitors showcasing products and services designed to enhance the quality of life for individuals living with dementia. From cutting-edge technologies to practical caregiving tools, find innovative solutions to meet your needs.
DON’T MISS OUT!
Running alongside UK Care Week, Naidex, and the Neuro Convention, the Alzheimer’s and Dementia Show unites interconnected aspects of health, social care, rehabilitation, inclusion, and diversity. This collaborative environment provides a comprehensive look at the broader care community. Find out more - www.alzheimersshow.co.uk







Commercial Kitchen and Laundry Solutions (CKLS) are one of the UK's leading suppliers of commercial kitchen and laundry equipment.

Whether you are a small sized residential home or large scale nursing home group, CKLS has the expertise and equipment you need to keep your operations running smoothly.
At CKLS, we understand that the success of your business depends on the quality of the equipment you use. That's why we've made it our mission to provide businesses across the UK with the highest quality commercial laundry and kitchen equipment available. We work with only the best manufacturers in the industry to ensure that our customers get the most reliable and efficient equipment possible.
Our commitment to our customers doesn't end with the sale of our equipment. At CKLS, we know that maintenance and repairs are crucial to keeping your equipment functioning at its best. That's why we offer
a full range of maintenance and repair services to our customers, including emergency repair services available 24 hours a day, 7 days a week.
We believe that our success as a company is measured by the success of our customers. That's why we're constantly striving to provide better products and services to help our customers achieve their goals. We're proud to say that our commitment to excellence has earned us a reputation as the go-to provider of commercial laundry and kitchen equipment in the UK.
So, if you're looking for reliable, high-quality commercial laundry and kitchen equipment, look no further than CKLS. With our extensive range of products and services, we're confident that we can help you find the right equipment to meet your needs and keep your business running smoothly for years to come.
Visit our website www.ckls.co.uk contact by phone on 01200 411914 or email at sales@ckls.co.uk.
Mobile Kitchens Ltd specialises in the hire or sale of temporary catering facilities and foodservice equipment.
Ideal for events or to provide temporary catering facilities during your kitchen refurbishment, our versatile units and equipment offer an efficient and economic solution to the caterers’ needs.
Production Kitchens, Preparation Kitchens, Warewashing Units, Dry Store Units, Cold Rooms and Restaurant Units are available as individual units in their own right or they can be linked together on site to form a complete complex.

Alternatively, we can offer modular, open-plan facilities, usually for larger, longer-term hires.
We offer a free design service, and project management from concept through to delivery and installation on site, plus full technical support throughout the hire period.
The standard specification of our smallest Production Kitchen unit includes a six burner oven range, salamander grill, twin basket fryer, upright fridge, hot cupboard, single bowl sink unit with integral hand wash basin, plus ample power points to plug in Microwaves, Food Processors, Toasters etc. Internal equipment can be interchanged and clients can effectively specify their preferred layout.
We have many tried and tested design layouts and would be pleased to put forward our recommendations for your project. So if you’re planning a refurbishment or need to cater for an event then why not give us a call and we’ll be happy to provide advice and put forward a competitive proposal. For further information or to arrange a site visit, email: sales@mk-hire.co.uk or call us on 0345 812 0800, or visit our website: www.mk-hire.co.uk


Infection control is critical in care homes, where laundry processes play a vital role in hygiene management. Care homes face increased pressure and scrutiny with changes to the Care Quality Commission inspection framework, and it is absolutely fundamental that care homes know how to safely ensure efficient infection control across all areas. CQC inspections place heavy emphasis on evidence-based infection control practices, including rigorous checks on laundry processes. Compliance with these standards is essential to safeguard residents, maintain trust, and achieve strong CQC ratings.
There are various way to ensure the right levels of hygiene control; you should employ thermal and/ or chemical disinfection. Ozone is one of the disinfection options that can be successful, but it is essential to adhere to HSE recommendations, take appropriate safety precautions, and use control measures as outlined by COSHH as use of this powerful oxidant does carry potential health risks. Forbes Professional offers care homes alternatives to Ozone systems, that still meet the most exacting hygiene requirements. Their

Miele commercial laundry machines enable sluice, thermal and chemical disinfection, to meet all the industry requirements of WRAS and CQC. When paired with Forbes’ advanced chemical detergents, which kill pathogens even at low temperatures, these commercial machines deliver a complete laundry solution for optimal infection control.
Forbes understands that care homes require tailored solutions. Their industry specialists work closely with operators to recommend the right commercial machines to meet their specific needs. Beyond installation, they offer award-winning service support to ensure ongoing compliance and operational efficiency.
For any care home, laundry is a key part of infection control. It is imperative that appropriate commercial laundry equipment is used within a care setting, and that there is a reliable partnership in place for service and maintenance. By choosing Miele’s technology and Forbes Professional’s expert support, care homes can safely and effectively meet stringent hygiene standards.
See the advert on the facing page for further information on Forbes.
MAG Laundry Equipment is a multi-award-winning supplier of commercial washing machines & tumble dryers that supports over 10,000 care homes across the UK. Clean laundry and bedding is critical for care homes, hospices, nursing homes, hospitals and other healthcare organisations. With a nationwide fleet of accredited engineers MAG Laundry Equipment has successfully assisted over ten thousand care homes with their products, services, information and support.
MAG’s product range includes commercial washing machines, tumble dryers, ironers, presses and detergents. For 100 years, since 1922, MAG’s products have been developed and improved to become some of the most reliable, energy-efficient and

the machines, and giving them a check-over, to see which parts, if any, can be carried over the refurbishment. Lavamac will only carry over the highest-quality parts from the machine from pre to post refurbishment. The machine then undergoes an extensive refurbishment, with almost all the parts being replaced, with the refurbished machines being given specialist parts based on the model type.
not only contributing to a greener way of
but also saving our customers money!
We have recently set up a specialist facility in St. Neots, near Cambridge, in which we are going ahead with this specialist refurbishment programme. This programme involves purchasing existing machines, and replacing the parts on them, so that they are as good as new, whilst retaining the look and feel that existed before, but with a massively increased lifespan, and a warranty on the machines that’s as good as a warranty on a new machine to go with the refurbishment too. Our refurbishment programme in our specialist facility includes stripping down

We recently have been awarded a bronze award in sustainability by the groundworks trust, affirming our commitment to the sustainability industry – however, as much of a compliment as it is, it does not mean that the hard work stops there! The next step on our journey is to hopefully be awarded the prestigious silver sustainability award! For this, we need to ensure that our carbon emissions are being cut down from our vans, continue our sustainability and refurbishment programme and to keep making green decisions within the company! 0151 317 3127 info@laundrytec.com www.lavamac.eu


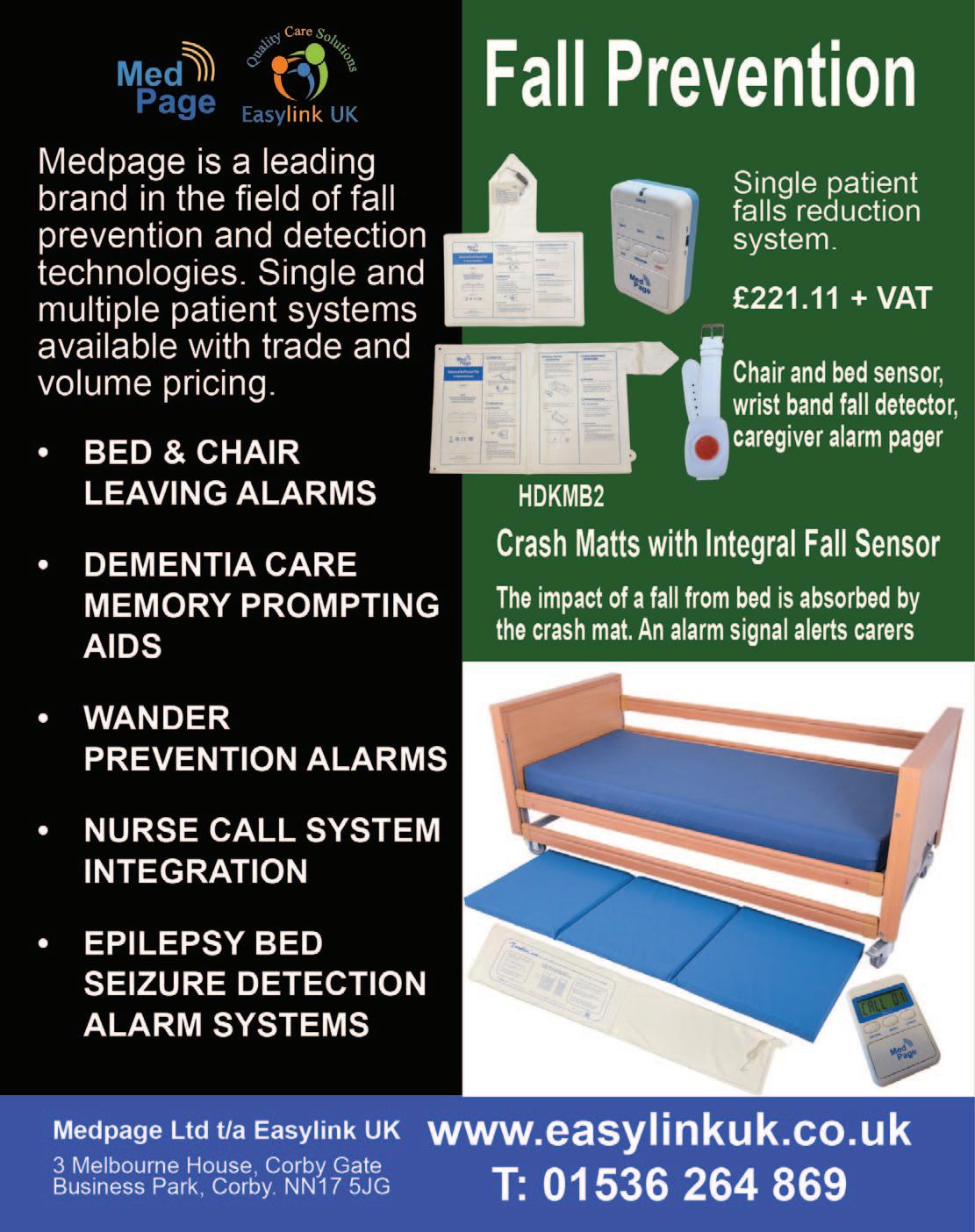
FALL SAVERS ® WIRELESS MONITOR

Eliminate all cables with our new generation falls management solutions!
Upgrade your falls programme with the latest technology from Fall Savers®. The
Fall
eliminates the
between the monitor and sensor pad. This results in less work for nursing staff, improved safety for patients and reduced wear and tear on sensor pads. Wireless advantages include the ability to use one monitor with two sensor pads simultaneously and support for many new wireless devices.
BENEFITS INCLUDE:
Safer for patients; less work for staff Bed and chair pads available One monitor works with two sensor pads Integrates with most nurse call systems A variety of options, including: Call button Pager


In the post pandemic world, we have all seen the effects of supply chain problems with the invasion of Ukraine and other alarming global factors, ever increasing costs of living and other more local issues which have driven up the rate of inflation over the last few years. The impact of this meant that most manufacturers of electronic products had to increase their prices as costs spiralled. This, of course, has impacted the end user. The most dramatic impact has been on the Care Industry. An industry that has lacked the support it desperately needs in these trying times.
Courtney Thorne, at the same time, took a strategic decision to take a close look at our core products, right down to component level, the objective being to make us less vulnerable to future global supply chain issues, and to reduce the cost of each product with the amin of ensuring that we deliver the same high quality product at a cost protected price. We had to ensure that this would happen without jeopardising the superb lev-

els of support we provide to our valued customer base.
This ground up review involved all departments from Research and Development right through to the Field Service team (and everything in-between). This in-depth collaboration took time as we had to ensure that each and every element was refined, perfected and tested to our (and our customers) rigorous requirements.
Whilst many organisations have limited-time or end of product line offers, we are very pleased to announce a price reduction on our core Connect and Connect Health Nurse Call system ranges. With flexible terms, full integration with Care Apps, celebrated service delivery and the most reliable and robust solution now at a new lower price, there has never been a better time to talk to us about a new nurse call system.
For more information email us at: info@c-t.co.uk or see the advert on this page.
Blaucomm’s Nurse Call Messaging Service (NMS) is the market leading solution to remove the dependency on noisy nurse call panels and pagers, through its intelligent software, which delivers the alerts straight to the care staff who need them. Care homes are rapidly introducing smartphones for digital care planning and eMarnow, the same devices can be used to receive the nurse call alerts they need for the residents under their care.
Furthermore, Blaucomm NMS is deeply linked into Person Centred Software MCM, so call bell data is linked straight to care plans. This unlocks a huge benefit to care homes to enhance the staff performance with how they accept and respond to residents, which ultimately promotes better response times and visibility for management to audit their performance.

The best part is that Blaucomm NMS links into your existing nurse call system - we work with all major
brands such as Aidcall, ARM, Courtney Thorne, C-TEC, ENS, Intercall, Medicare, SAS and TeleAlarm.
Care operators are constantly recognising Blaucomm NMS for its reliability and dependability to their care operations, which is why we’ve been chosen time and time again over other solutions.
Head of IT Trudi Harrow at WCS Care had this to say about Blaucomm NMS:
“We find Blaucomm is a genuinely fantastic company with a reliable product.
"We would highly recommend this to anybody who wants to replace expensive pagers and silence those annoyingly loud nurse call screens!”
To find out more about Blaucomm NMS, visit
www.blaucomm.co.uk/healthcare
See the advert page 5 for more details.
Medpage Limited has collaborated with a leading UK manufacturer of crash mats to deliver a cost-effective tool for falls management strategies. The inclusion of the new TumbleCare full-length pressure mat sensor ensures that should a patient tumble out of bed, an alarm signal is generated to alert care staff to the incident, resulting in a recordable improvement to patient safety and service.
Crash mats act as a protective barrier, absorbing the impact of a fall and reducing the risk of serious injuries when a person tumbles out of bed. Beneficial for individuals who are at high risk of falling, such as older adults, patients recovering from surgery, or those with neurological conditions such as epilepsy.

Falls can pose significant risks, especially in healthcare settings and senior care facilities. Every year, thousands of people suffer injuries due to falls from beds and other furniture. To prevent these accidents and ensure the safety of patients and residents, it is essential to implement effective falls and safety management strategies.
Further details can be obtained by telephoning 01536 264 869 or emailing sales@easylinkuk.co.uk
See the advert on page 2 for details.

The care sector faces unprecedented challenges. A growing elderly population with increasingly complex needs, coupled with a shortage of qualified staff, puts immense pressure on care homes. But amidst these difficulties, technology offers a beacon of hope. We at 9Solutions, want to be at the forefront of tackling these issues, providing innovative solutions designed to empower caregivers and enhance the quality of life for residents.
Our location-based solution, with customizable safety zones and realtime alerts, allows for proactive intervention, ensuring resident safety while preserving their independence. Picture a fall occurring in a quiet corner. Instant notifications, pinpointing the exact location, enable staff to respond swiftly, minimizing potential harm.
Efficiency is key in today's demanding care environment. Care home staff are bombarded with alarms, leading to "alarm fatigue" and delayed responses. Our system personalizes alerts, directing them to the right caregiver, reducing workload and improving efficiency. One app manages calls, tracking, and tasks, allowing staff to focus on providing care.

Remote communication tools allow staff to check on residents virtually, reducing unnecessary physical rounds and minimizing disruptions. This frees up valuable time for personalized care and meaningful interactions – the heart of quality caregiving.
We understand that technology should be a support, not a burden. That's why our user-friendly system, developed with care professionals, combines diverse functionalities into a single intuitive platform. This min-
imizes the learning curve, allowing staff to focus on providing exceptional care. Crucially, it also integrates with Care Management softwares, ensuring smooth workflows and easy adoption.
BENEFITS OF 9SOLUTIONS TECHNOLOGY
Reduced workload: Automation and intelligent systems streamline tasks, easing the physical and emotional burden on caregivers.
Enhanced safety: Proactive alerts and location tracking ensure resident wellbeing and peace of mind for families.
Improved efficiency: Optimized workflows and personalized task management empower staff to deliver timely and effective care.
Increased resident satisfaction: Technology fosters independence while ensuring prompt assistance when needed.
The future of care is not about replacing human touch with technology, but about using technology to create space for more of it. It's about empowering caregivers, promoting resident well-being, and reimagining care in a way that prioritizes human connection.
Read more or contact us at www.9solutions.com or sales@9solutions.com

Technology has made people more connected with the world around them and the revolution in assistive care devices has made it possible for the elderly to spend their last years in a comfortable and familiar environment. These devices have also made it easier for home carers to provide quality care for their loved ones while managing their own lives. They allow you to care for your elderly whether they are travelling in the city for errands, staying alone at home, or staying in the same home as you. They are also helping nursing homes provide better care for them with discrete monitoring and quick responses to emergencies.

If you’re looking for these kinds of assistive care devices for your loved ones or nursing home, Frequency Precision produce some of the best systems available to help you with elderly care and mobility monitoring, ranging from bed, chair and floor sensor mats through fall monitoring and GPS tracking to fully integrated nurse call plug or wireless systems.
Phone: 01837 810590
Email: contact@frequencyprecision.com
Website: www.frequencyprecision.com


Since our founding in 2010, Activities to Share has been dedicated to enhancing the lives of those in care by providing thoughtfully designed activity products. Our mission is to support activity coordinators in delivering uplifting, engaging experiences that foster connection, joy, and well-being.
We achieve this by listening closely to your feedback and evolving with your needs. Whether over the phone, via email, WhatsApp, or Live Chat on our website, our team is always ready to offer advice and help you find just the right products to bring your ideas to life.
While we embrace the convenience of technology to expand our resources and share knowledge, we remain firm believers in the irreplaceable power of sensory

Angloplas are a UK manufacturer who specialise in producing dispensers for the health and hygiene industry. Although these are designed to keep the workplace tidy and uncluttered they are, more importantly, built knowing the control of healthcare-associated infections (HCAIs) are a priority for healthcare providers, and who are employing a combination of infection prevention and control strategies, including hand hygiene, cleaning, training and the adoption of new technologies, to tackle the problem. As a result, a wide range of infection control products and technologies are emerging on the market, including antimicrobial technology. Angloplas’ range of dispensers are produced in the world’s first proven Antimicrobial PVC with silver

ion technology and which is exclusive to Angloplas. This helps reduce the risk of cross infection by stopping the growth of bacteria and mould and works continuously for the lifetime of the product, reducing levels of bacteria such as MRSA, E Coli, Legionella, Salmonella and mould by up to 99.99%.
For non-clinical environments Angloplas has recently launched its new Budget Range of products which are made to the same exacting standards as the antimicrobial protected ones but with lower price tags.
You can order Angloplas products directly from its website at www.angloplas.co.uk See page 6 for details.
MOWOOT II – proven solution to chronic constipation without medication
Developed by a team of doctors and other healthcare professionals, MOWOOT II performs gentle abdominal massage to speed up intestinal passage in people experiencing chronic constipation.
Clinically proven, safe and effective, relaxing and sideeffects free, MOWOOT II Abdominal Massage Therapy System combats constipation and provides soothing relief to affected people.

Easy to use and comfortable, the MOWOOT II treats and manages constipation in people with spinal cord injuries, multiple sclerosis sufferers, Parkinson’s Disease patients and people with constipation related to prescription medication. MOWOOT II also helps to relieve idiopathic constipation experienced by menopausal and post-menopausal women
Consort Claudgen’s innovation in the electric heating industry takes another leap forward by introducing Wi-Fi-enabled heaters to their low surface temperature (LST) range. These cutting-edge heaters offer unparalleled convenience and efficiency. The heaters connect directly to Wi-Fi, enabling users to control heating through the digital control panel on the heater or via the Consort Connect app. With a comprehensive 7-day timer, which allows 24 individual heating periods per day, and features such as a lock function, open window detection, and custom automation, users can tailor their heating needs to their preferences. Adding to the ease of use, users can view the
and older and elderly people.
In clinical studies
MOWOOT II increased evacuation frequency, softened stools, improved regularity, reduced gasses, relieved bloating and eased off abdominal discomfort.
10 to 20 minutes daily of relaxing abdominal massage with MOWOOT II rapidly reduces symptoms of constipation. Evident results are experienced only a few days after the first treatment. Regular abdominal massage with MOOWOOT II ensures lasting health benefits and better quality of life.
MOWOOT II – effective solution to chronic constipation for better quality of life!
Supplied by Win Health Medical Ltd - 01835 864866 - www.win-health.com
See page 3 of this issue for other Win Health products.

energy consumption statistics of all connected heaters, providing insights into usage patterns and potential savings. The LST heaters with Wi-Fi and occupancy sensors have a self-learning control ability. They utilise inbuilt occupancy sensors to detect and learn a user’s weekly presence in a room, creating an intuitive heating schedule. When the space is unoccupied, the heater conserves energy by switching to a setback temperature or frost protection mode.
BIM (Building Information Modelling) objects for the heaters are available for download from Consort’s website. 01646 692172 | sales@consortepl.com | www.consortepl.com See the advert on page 6.
engagement. That’s why we continue to make our Reminiscence Kits and Sensory Bags with real, tactile items that stimulate the senses. Some experiences—like popping bubbles for the splash, breathing in a familiar scent, or piecing together a puzzle with others—simply can’t be replicated on a screen. These sensory moments are invaluable in encouraging storytelling, sparking memories, and fostering conversation.
Our values remain rooted in this commitment to meaningful connection. We’re here to partner with you—the professionals on the front lines of care—to create a sense of structure, well-being, and fun for those who need it most.
Are you longing for your activity diary to be full? Look no further www.activitiestoshare.co.uk are here for you! See the advert on page 7 or: customers@activitiestoshare.co.uk
0117 966 6761
07900 6751 50
C&S Seating Ltd have provided postural control equipment to residential homes, hospices, medical equipment services and NHS trust hospitals nationwide since 1991.
With 9 different sizes of TRolls and Log Rolls, in a removable and machine washable Waterproof Titex or Soft Knit material. These rolls are used to control posture and position of the body in either supine or side lying. Our Knee & Leg support wedges are

“Jolly
The new “Jolly Journey” from Little Islands is designed to simulate an old-fashioned travel carriage, featuring real wood panelled wall, brass luggage racks, ornate wall lights and table lamp, opposite-facing seating for four, including cushions, ‘First Class’ antimacassars and period memorabilia.
The Jolly Journey creates a familiar and stimulating environment for ‘passengers’ to return to their fondest memories, sparking conversations of time gone by. Reminisce about travel and holidays with loved ones

and furnish your opulent ‘First Class Carriage pod’ with all accessories and footage. All we require is 2.5M of clear wall space, a power socket and good access, to create your very own Jolly Journey. For more information please contact Little Islands: 01828 869802 or see the advert on page 5.


PASS supports over 1,000 care providers every day, giving them access to market leading care management tools hand in hand with unlimited 24/7/365 support from our dedicated and friendly PASS team.
Assured by NHS Transformation Directorate, PASS provides a secure platform that allows you to plan, record and evidence the care you deliver. The only assured solution built specifically for the home care sector, it provides comprehensive real-time functionality and allows you to share progress against outcomes with customisable, exportable reports.
CARE PLANNING AND ROSTERING FROM A SINGLE PLATFORM
To meet the wider needs of the PASS community All-in-one PASS has recently been launched , bringing advanced rostering functionality to our established digital care planning platform. As a result advanced staff scheduling, payroll and invoicing functionality is now seamlessly linked with care planning and reporting, reducing the technical complexity, risk and overhead associated with integrating two separate systems.
As a result, PASS now provides an all-in-one suite of digital care management tools, available from a single platform, designed to:
Save you time
Increase the efficiency of your teams
Improve the quality of care
Deliver better outcomes
INTEGRATED HEALTH AND SOCIAL CARE
Our commitment to the continual evolution of PASS is further illustrated by the addition of GP Connect. The first product of its type to offer this feature, PASS is still one of only a handful of digital care management solutions to have completed this NHS Digital integration, and is the only one offering it to the home care market. PASS GP Connect provides authorised social care staff with realtime access to their client’s GP records. It makes medical information available when and where it is needed, leading to improvements in both care safety and outcomes:
Visibility of allergies, vaccinations and medications, especially useful for clients unable to reliably share their personal information
Using medical information to inform care planning
Ensuring that the right medication is delivered to the right person in the timeliest manner. In one case, this allowed the administration of antibiotics on a Friday evening, aiding the service user’s swift recovery from infection
Available to all PASS users at no additional cost, PASS GP Connect is significantly more efficient than waiting for a GP response. It’s also a positive step forward on the path to the DHSC’s goal for widespread digitally enabled care and is in full alignment with their ambition for joined up care for everyone.
Get in touch: www.everylifetechnologies.com hello@everylifetechnologies.com
Envivo Group is at the forefront of care and support sector, driving innovation that enables people to live lives full of choices and opportunities. They have 202 locations that are now using Mainteno Facilities Management software.
“Our experience with Mainteno at TLC/Envivo Group has been really positive already. Since its rollout it has shown real and measurable benefits and has had a marked impact on the workload and assurance of our operations team.
"We can now raise issues whether large or minor, almost the instant they are spotted. We can denote the priority with which they need to be tackled and track the progress of works to rectify them. It has reduced almost completely the need to be directly contacting people to resolve issues. It has been obvious that the streamlined approach that it provides helps in prioritising works for maintenance teams and contractors, gives them plenty of detailed information
as to the exact issue and has given us an evidence base to show that issues are resolved in a consistent and effective timeframe.
"The details that are available once a job is logged are invaluable. We can evidence to regulators etc that there are plans to rectify any outstanding works that they may pick up. I've been very impressed with the details that are passed back to me through the platform as works are ongoing and also when they are completed. It's proved to be a valuable reference to ensure that we are not doubling up requests, working through tasks in a logical way and also to confirm the completion of works remotely.
"For a site of our size and complexity especially, a toolkit with this level of effectivity and scope has been an incredible help.”
Group Facilities Manager sales@redro.uk www.mainteno.com





The social care sector is evolving at an unprecedented pace, driven by increasing demand, tightened budgets, and the need to deliver exceptional care outcomes. At the heart of this shift lies digital transformation—a holistic approach to overhauling care operations, processes, and culture through the integration of modern technologies.
Far from simply replacing manual tasks, digital transformation reimagines how organisations operate. Tools like Digital Social Care Records (DSCRs) represent just the beginning. By adopting interoperable systems and cloud-based solutions, care providers can achieve seamless coordination across departments, optimise resource allocation, and ensure high-quality care. Processes such as care planning, rostering, compliance reporting, and data management become more efficient, freeing up teams to focus on providing person-centred care.
Digital solutions also offer significant benefits. Faster service delivery reduced administrative burdens, and more informed decision-making results in better care experiences for service users and care providers alike. For instance, interoperability enables real-time data sharing across platforms, reducing errors while providing a unified view of the organisation’s operations. This empowers leadership to make critical decisions backed by accurate, holistic insights. Additionally, tools like single sign-on (SSO) and multi-factor authentication bolster security, ensuring confidential data remains protected while reducing day-to-day inefficiencies for users.

For social care providers, the move toward digitalisation represents an investment in long-term sustainability. Enhanced efficiency helps reduce operational costs, allowing resources to be reinvested in vital areas such as workforce development or service user engagement. Standardised digital frameworks also simplify the complexities of acquiring new services or locations, ensuring continuity of care during periods of growth. Choosing a digital partner who understands the complexities of care is essential to navigating this transformation successfully and tailoring solutions to the unique needs of the sector.
However, the path to digital transformation requires a clear roadmap. Providers must assess their needs, define a vision, and secure stakeholder buy-in. Selecting the right software and delivering effective training is equally critical to ensuring a smooth transition. Continuous monitoring and adjustment allow providers to refine their approach, fostering a culture of improvement and resilience.
By adopting integrated intuitive software solutions, social care providers can not only stay ahead of industry challenges but also lead the way in delivering exceptional, sustainable services. Digital transformation may not solve every challenge, but its potential to enhance care quality, operational efficiency, and financial health is undeniable.
Visit OneAdvanced at stand H24 at UK Care Week to learn how we can support your journey or download our guide to digital transformation with the QR code.
SFIncS r/3 - A Fee Income System especially for Residential and Nursing Care Homes
Designed to deliver simplicity and ease of use coupled with speed, flexibility and accuracy, SFIncS r/3 (Simple Fee Income System release 3) has a proven track record of over 12 years in use.
Originally developed and prototyped as an MS Access database, since 2017 SFIncS r/3 has lived entirely on the cloud, so is available 24/7 from anywhere in the world.
As a completely bespoke package, born of necessity and collaboration between seasoned software consultants with ties to the care industry, SFIncS r/3 offers innovations and capabilities not found in any other system.
Separation of sponsor and service user responsibilities permits unlimited sponsor/service user relationships, and as any number of charge codes may be defined, this allows complete flexibility of service user/sponsor /charge code definition.
Its unique continuous billing function is the most efficient means possible of defining recurring charges (an entry is only required when a change occurs) and both an ad hoc charge function and a
cashbox module are available for incidental expenses (either or both can be used).
Use of the balance forward accounting principle (which makes unnecessary invoice matching a thing of the past - though invoicing is included) plus super quick receipts entry using just ‘six clicks’ makes SFIncS r/3 almost effortless to use.
Paula, who owns and operates Monkstone House Residential Home in Porthcawl testifies to it’s incredible prowess: “With 41 partly private and partly sponsored service users, some of whom are multiply funded, it takes me only 30 to 40 minutes per week to keep both my accounts and fee income up to date! More importantly, I never need to worry about underpaid or overpaid fees - everything is always spot on. And the invoices and statements produced let me present the polished and professional image I need.”

SFIncS r/3 integrates easily with any accounting package, can be used by any type of care home and by single or multiple home operators alike.
For more information email benjones@intracare.co

Better by Design: A Fee Income System especially for Residential and Nursing Care Homes
We've analysed every aspect of fee income processing to the nth degree and developed a bespoke solution that delivers simplicity and ease of use coupled with speed, flexibility and accuracy – all in one outstanding application package.
SFIncS r/3 is the ultimate fee income management and control system.
• Unlimited sponsor and charge code assignments allow complete flexibility of service user billing profiles.
• Perfect for all types of care homes - Nursing, Residential, Mixed, Specialist.
• Unique continuous billing functionality provides the most efficient charge definition possible. Only charge start points need to be maintained and all sponsor charges for each service user (including historic) are shown on just one screen.
• Completely flexible invoicing. Invoice any sponsor at any time for any charges for any service user for any period of time.
• Super fast receipt entry including ‘Six clicks’ copy functionality.
• Balance forward accounting means you can forget laborious invoice matching.
• Ad hoc charges functionality.
• Cashbox module included.
• Works for multiple or single home operators.
• Integrates with any accounting system.
• Plus all the reports, views and graphs you’ll ever need.
• In use for over 12 years.
• Free training and help with system set up.
• Historic data loading option available (charges may apply).
• 30 day free trial.
For a demo, free trial or for further information please email benjones@intracare.co or visit https://intracare.co/

By Dr Angela Brown, Founder and Chief Executive Officer of Training

several quick and easy changes which the government
could swiftly implement to significantly improve the sector in the shortterm.
A start would be to focus recruitment on the individual progression plan of the care worker. Afterall, surely a sector which traditionally has poor pay and responds to ever changing societal needs, deserves some control over what are perceived are important skills.
The sector still relies on recruitment via word of mouth and offers low pay and low recognition of the skills required in adult care as an incentive. While the workforce needs to respond to the needs of employers, we have a duty to understand the needs of the carer by providing progression of their own career pathway.
The early years sector faced a similar challenge with public perception. Since no one needs a qualification to have a child, it was perceived by many – and even some in government – that the skills required to work in the sector simply came natural.
Although the early years sector has not yet chased all of its demons, public perception of the skills required undertook a change andlargely helped by the excellent Sure Start system - parents began to understand the value of having a skilled workforce to look after our children. It seems an alien concept to us now, but it is very much where we’re at with care, and it doesn’t need to be that way.
In care today, we’re constantly seeing headlines of endemic staff shortages and staff burnout, but this could be significantly improved if the expectations of the sector are proactive rather than responsive.
This is what the Commission may conclude, but in the short-term, we need to invest in the current army of the workforce whose goodwill and compassion is relied upon to respond out of decency rather than an identified societal need.
Demands on the NHS can also only be supported by an adult care sector which is respected for the skills they possess.
For 2025 to herald in some immediate change, let’s utilise Government skills funding and Department of Social Care workforce development programmes to really drive the sector forward.
Let’s find out what the people receiving care really want from their care plan and let them have a say in what the devolved authorities are spending on.
Let’s be ambitious and listen to the sector, use its expertise and plan for a service which not only works well in conjunction with the NHS, but one which is respected and rewarded.
Let’s make 2025 the year we start seeing real change in the care sector.

In the ever-evolving landscape of adult social care, it is essential to ensure that training initiatives not only equip care professionals with the necessary knowledge and skills but also nurture an environment where they feel confident and supported to deliver their best.
As a Registered General Nurse with over two decades of experience in the care industry, I have seen first-hand how thoughtfully designed training programmes can bring about meaningful changes that resonate with both staff and residents. These programmes, when aligned with the real-world needs of care professionals, have the power to transform not only the quality of care but also the overall morale and satisfaction within the care setting.
One of the key features of impactful training is its accessibility, relevance, and applicability to the challenges faced by care staff on a daily basis. From comprehensive first aid instruction to specialised courses on dementia care, well-designed training modules can provide care professionals with the tools and techniques required to respond effectively to a variety of situations. By prioritising the development of our staff's clinical proficiency, we enable them to deliver high-quality, person-centred care that focuses on the well-being and dignity of residents.
However, building confidence and capability goes beyond technical skills alone. It is equally vital to focus on the interpersonal skills that underpin meaningful relationships with residents and contribute to their overall happiness and fulfilment. Training programmes that emphasise relational care, for instance, can help care staff appreciate the importance of creating an atmosphere of trust and understanding. By
encouraging staff to focus on these human aspects of care, we cultivate a setting that radiates warmth and kindness, ensuring that residents feel valued and respected.
Moreover, to ensure that staff can consistently provide the best possible care, our training must remain adaptable and responsive to emerging trends and best practices in the sector. By implementing regular refresher courses, we reinforce foundational knowledge, address any skill gaps, and ensure that care professionals are up to date with the latest advancements. Similarly, ongoing supervision and performance evaluations play a vital role in identifying opportunities for professional growth, creating a framework of accountability and continuous development. This commitment to lifelong learning not only enhances the quality of care but also reinforces a sense of purpose and pride among staff.
The ripple effect of robust training programmes extends far beyond individual care professionals. When staff feel confident, valued, and well-equipped, they are better positioned to deliver exceptional care that is tailored to the unique needs and preferences of each resident. This, in turn, results in improved well-being for residents, greater peace of mind for their families, and stronger outcomes for the care community as a whole.
At the core of our training philosophy lies the understanding that empowered staff lead to empowered residents. When care professionals are equipped with the knowledge, skills, and assurance to excel in their roles, they are better able to encourage residents to maintain their independence, involve them in decision-making, and take the time to truly listen to their stories and concerns.
In conclusion, aligning training with the practical needs of both staff and residents goes far beyond fulfilling regulatory requirements—it is the foundation for fostering confidence, compassion, and excellence in adult social care. As we look ahead to the challenges and opportunities of the future, let us remain steadfast in our commitment to investing in our staff, enabling them to make a lasting difference in the lives of those they care for.
By Elena Martin, Director
of
Operations
and Commissioning, Langdale Care Homes Group (www.langdalecarehomes.co.uk)
By Daniel O’Shaughnessy,

You wouldn’t run a care home without a health and safety lead, and the same should apply to data security and protection leads. Losing access to critical data, even briefly, can be devastating for residents’ welfare and your business’s viability. If care plans and medication records are unavailable due to a cyber incident or software issue, residents’ wellbeing is at risk.
Finance system failures can disrupt payroll, invoicing, and payments.
While data protection is everyone’s responsibility, having a named individual to lead on data security and protection is essential. This role provides senior leadership and ensures good practices are followed across the organisation. At Digital Care Hub, we use the term data security and protection lead to describe this role.
The lead should champion data security policies and set an example. While daily tasks can be delegated, the lead ensures standards are met. This role doesn’t have to fall to the Registered Manager but should be assigned to someone senior enough to oversee responsibilities effectively. In larger organisations, aspects of the role can be shared – for instance, one person might manage risks while another handles information governance.
It’s vital that leads have the right knowledge and skills. To address training gaps, Digital Care Hub’s Better Security, Better Care programme has launched a free, open-access elearning course tailored for data security and protection leads. This complements an existing course for all staff, which we recommend completing first.
The course, launched in January 2025, supports continuing professional development (CPD) and meets the training requirements of the Data Security and Protection Toolkit (DSPT). It is the only free resource designed specifically for this role in adult social care.
The training reflects real-world scenarios across care homes, supported living, home care, and community services, covering all client groups. The course includes four modules:
1. Data protection rights and responsibilities
Covers the lead’s responsibilities, other specialist roles, and key skills and
support needed for the role.
2. Keeping data secure
Explores managing data, understanding personal data rights, access to data, Information Asset Registers, and Data Protection Impact Assessments.
3. Threats to data security
Focuses on recognising, preparing for, and recovering from cyber incidents; reducing threats to digital systems, devices, and supply chains.
4. Data breaches
Explains how to differentiate between breaches, incidents, or near misses; record and learn from incidents; and respond to and report breaches appropriately.
By completing this course, data security and protection leads will enhance their knowledge of data protection and cyber security, ensuring they can safeguard their organisations, staff, and the people they support.
For more information about the course and other resources, visit www.digitalcarehub.co.uk/elearning.


Leanne Silverwood is the Founder and Managing Director of Local
Care Force

As Local Care Force celebrates 20 years of business, we look back on two decades of momentous changes in the health and social care sector. From technological advances to ongoing recruitment and retention issues, supply chain management companies driving down prices and quality, and changes to the agency landscape, the health, and social care sector, post-pandemic, has not only had to adapt but has also needed to rise to meet these challenges.
In 2020 the health & social care sector faced a devastating crisis in Covid19.
Care home staff were under unimaginable pressure, working long hours, managing PPE shortages, and the emotional toll of caring for residents who were isolated from their families. We had to adapt quickly, deploying staff where they were most needed, while maintaining their safety, and that of the residents they cared for. It demonstrated the resilience and dedication of our workforce - and we are so incredibly proud of the commitment they showed throughout this difficult time.
Post pandemic the issue of recruitment worsened. In 2023 the health & social care vacancy rates stood at 152,000 roles (9.9%) substantially higher than the overall UK rate of 3.4%. It was a challenging time, to say the least. Alongside issues around recruitment, were problems with retention which significantly impacted the health and social care landscape, with 390,000 (28.3%) leaving the sector in 2022/23. (The Kings Fund 2024).
As a health & social care agency, Local Care Force has been at the forefront of this ongoing crisis. The ever-growing demand for qualified healthcare professionals has proven to be a difficult obstacle to over-
come. Our role in providing experienced, skilled, and compassionate staff has never been more critical, or difficult, and it is the reason we offer specialist in-house training led by our clinical lead nurse, who also acts as a mentor to our team.
The agency sector has not been immune to challenges post-pandemic. In the past, agencies were regulated by the CQC, but for several years now, they have been unregulated. This lack of oversight has led to a surge in "back bedroom" agencies, which supply staff without conducting the necessary checks to ensure resident safety. Additionally, these agencies often disregard tax regulations when paying staff, leaving care homes liable for tax shortfalls. Consequently, we advise all clients to question any £14 hourly carer charges, as it has become easier for anyone to recruit and place nurses in care homes. This trend is particularly concerning, as we pride ourselves on our robust recruitment and safeguarding processes to ensure the wellbeing of the residents our staff support.
The Work Rights Centre report has highlighted another troubling issue within the industry: the flawed sponsorship visa system and the exploitation of foreign workers in the health and social care sector.
Migrants constitute 32% of care worker roles in England, many of whom face excessive hours or underemployment, struggling to change visa sponsorship, and fearing reprisals if they voice their concerns. As an agency, we cannot recruit staff requiring visas. However, we are disheartened to see hundreds of people on sponsorship visas applying for work with us due to unscrupulous agencies exploiting legal loopholes. We frequently hear from individuals who aren't receiving enough work from their sponsors to sustain themselves, yet they cannot legally work elsewhere without invalidating their visas. The well-being of our workforce has always been paramount at Local Care Force. We firmly believe that protecting our staff, which in turn, protects the residents they support, a principle on which Local Care Force prides itself.
As we reflect on our two-decade journey, acknowledging the significant challenges we have faced, it's equally important to celebrate the positive advances we have made during this time.
We know that with dedication, collaboration, and a focus on innovation, we can continue to weather the storm. As we celebrate this milestone, we are committed to providing the highest standard of care and supporting the health & social care sector in whatever challenges the next 20 years may bring.
The delivery of safe care is the paramount responsibility of social care providers. Central to achieving this is the governance framework adopted by service providers. And at the core of this framework are policies and procedures. These enable the provider to comply – and evidence compliance – with relevant legislation and regulations, as well as facilitating best practices, supporting business needs, and assisting in recognising and managing risks.
Providers have a legal duty of care to the people they employ. Policies and procedures should provide clear guidelines to staff on how the organisation operates, as well as informing them of best practices and processes to be followed.
Policies should be reviewed annually as a minimum to ensure they are still fit for purpose and align with legal and regulatory requirements. They should be reviewed not only by employees of the business, but also by experts in various subject matters (e.g.,

infection control or medicines management).
For many small- to medium-sized providers, there may not be the in-house skills, knowledge, and experience to complete such a robust annual review. Many choose instead to purchase their policies and procedures from a reputable provider like W&P Compliance & Training, who will also complete reviews and ensure their policies and procedures remain up to date. This way a provider not only ensures they remain compliant; they also benefit from best practice policies and procedures that provide a solid foundation for safe working practices and – ultimately – protect and support service users and staff.
Ben Erskine – Director at W&P Compliance & Training www.wandptraining.co.uk | Tel: 01305 767104 See the advert on page 2 for further information.
Training care home staff is vital for delivering high-quality care, especially when managing complex resident needs such as dementia, frailty, and mental health challenges. However, traditional methods often fall short in engaging staff, leaving critical gaps in understanding and preparedness. Innovative approaches, such as game-based learning and peer-to-peer collaboration, are revolutionising training, particularly in addressing the ethical and legal challenges of restrictive practices.
Restrictive practices—measures that limit an individual’s freedom—are sometimes necessary to ensure safety. However, they must be applied with great care, adhering to legal frameworks and ethical guidelines to protect residents’ dignity. A groundbreaking digital training resource, codesigned by Queen’s University Belfast and Focus Games, exemplifies this innovation. The resource uses interactive, expert-driven content to help staff navigate restrictive practices responsibly and effectively.

Game-based learning plays a central role, transforming topics like restrictive practices into engaging,
real-world scenarios. Simulations allow staff to explore ethical dilemmas, practice decision-making, and test alternative solutions in a safe, low-pressure environment. This approach enhances critical thinking, teamwork, and retention of essential knowledge.
Peer-to-peer learning further strengthens the training by encouraging staff to share experiences and insights, fostering collaboration and practical problem-solving. This creates a dynamic learning environment where staff feel supported and empowered to deliver compassionate care. By integrating these modern approaches, care homes can elevate training into a meaningful experience, equipping staff to balance safety with residents’ autonomy and dignity. At Focus Games, we are proud to offer tools designed to empower care home teams through innovative training. Visit www.FocusGames.com or email info@focusgames.com to learn more about our Restrictive Practice resource and how it can enhance care home outcomes for
At Meaningful Care Matters, we have the privilege of working with health and care teams across the UK, Ireland, Canada, Australia and more recently Singapore.
It is no surprise that those who can embrace the culture change of our ‘Butterfly’ and ‘Dragonfly’ Approaches - in terms of reducing the institutional and task-focused aspects of care in favour of creating a sense of fun, friendship and true belonging - have leaders who are very self-aware and emotionally intelligent. What does that look like in practice? It involves being genuine as a person, being able to acknowledge mistakes, and taking time to really get to know your team members as individuals and what makes them tick. Our team are Authorised Partners in delivering the methodology of the DiSC personality profiling assessments and the Five Behaviours of a Cohesive Team™ programme (Lencioni, P) to help support teams to work together more positively and ultimately productively. Having been through the process myself, it was striking how accurate the analysis was of what motivates and what stresses me. It also helped me to know those stressors and motivators for my peers and how to adapt my approach to better look out for each other.

our own relationship with trust, based on experiences in our lives? Do we find it easy, or does it take us time? Being in touch with your own vulnerability is not about spilling out all your deepest, darkest secrets to the people you support! But it is about being able to reflect on times in your life when you have felt lonely, scared or lost, and for these reflections to enhance our empathy for those who are struggling. Once we have established trust and a sense of belonging in our teams, we can more easily be open about the things we disagree about, and for those differences or conflicts to be regarded as healthy rather than threatening to the stability of a team - provided they are talked about openly and kindly. Many teams flounder because there is an artificial harmony i.e. conflicts are under the surface and gossip and cliques can create an unsafe and unhappy work culture.
A recent social media post caught my eye which said “Your company culture is not words on your website or posters on the wall. It’s how your people feel on a Sunday night.”
What is your response to that question, and do you think you and your team might need some time and attention in 2025 to get back on track and unlock your full potential?
People working in care homes often experience the deaths of residents but this doesn’t mean each death is easier to cope with.
Hospice UK’s Compassionate Employers Programme deliver workshops to help care professionals manage recurring and often overlooked experiences of grief through their work.

Our next virtual session will be on: Wednesday 5 March 2025, 10.00 - 12.30
The cost is just £120 +VAT per person.
At the foundation of a good team is what Patick Lencioni describes as vulnerability-based trust, and this is something we talk about a lot in training for leaders and their teams. People who we care for, and their families put a lot of trust in us. So, what is
Sally Knocker is a Consultant Trainer with Meaningful Care Matters www.meaningfulcarematters.com

Book your space or find out more at: www.hospiceuk.org/coping-professionalgrief-workshop-march

In a landmark ruling, the High Court delivered a significant judgment on 14 January 2025, in favour of Hartford Care Group Limited (HCG), challenging the Secretary of State for the Home Department's (SSHD) decision to reject HCG's application for 70 Defined Certificates of Sponsorship (DCoS). This case, The King (on the Application of Hartford Care Group Limited) v. The Secretary of State for the Home Department, sets a crucial precedent for how the Home Office assesses applications for Defined Certificate of Sponsorship (DCoS), particularly in the care sector.
THE CASE BACKGROUND
HCG, a prominent provider of care services in the UK, has held a sponsor license since April 2019. On 8 January 2024, Aston Brooke Solicitors applied for 70 DCoS on behalf of HCG. These certificates are vital for nonUK workers to obtain a visa to work in the UK. However, on 29 January 2024, the SSHD rejected HCG's application, citing insufficient evidence to demonstrate a genuine need for additional staff.
Aston Brooke Solicitors swiftly initiated a Judicial Review, challenging the legality of the decision, which could have significant consequences for the care sector, heavily reliant on overseas workers to meet staffing demands and stating HCG contracts with their service users and the Local Authority did not state the number of hours.
THE LEGAL CHALLENGE
Aston Brooke Solicitors argued that the SSHD’s decision was unlawful, irrational, and inconsistent with the Immigration Rules. Aston Brooke Solicitors contended that the Home Office had imposed requirements not set out in the rules, relied on unpublished policies, and failed to assess the evidence properly. In particular, the SSHD insisted on receiving contracts that guaranteed specific hours of work, which Aston Brooke Solicitors argued were not standard in the care sector.
The SSHD defended its position by stating that additional information could be requested to validate the applications THE ADMINISTRATIVE COURT'S RULING
"23 years, operating 4 Devon Nursing homes, has been pretty tough, as anyone in social care, knows, only too well. And if it was hard already, after 2024 budget, it's just got harder.
Anyway, at heart, I am just customer of Eden Alternative, and it was a stroke of luck to come across this whilst on holiday in New Zealand in 2009. It started in USA in 1994 and now runs in 22 countries.
The fact that I am now involved with this not-forprofit organisation (in the UK area) came about when one of the 2 main UK directors died suddenly just before Covid. But it's something I have run with for 11 years to help make 'vision' a reality, not a struggle. So,
On 14 January 2025, the High Court ruled in favour of HCG, stating that it was irrational for the SSHD to require contracts with guaranteed hours to prove the genuineness of care worker vacancies. The Judge highlighted that flexible contracts are standard in the care sector, where the demand for staff can vary depending on factors such as local authority funding and service user needs.
The Judge also criticised the SSHD’s assumption that local authorities impose staffing quotas, pointing out that care providers have discretion over how many workers they need to meet demand. Furthermore, the Judge found that HCG’s evidence adequately demonstrated the genuine need for additional staff, rendering the SSHD’s rejection of the application irrational.
The Judicial Review application was supported by Care England and Professor Martin Green OBE chief executive of Care England stated after the verdict was delivered: “In winning the Judicial Review, Aston Brooke Solicitors has done a great service to the care sector because this victory will cause The Secretary of State for the Home Department to rethink how they behave towards the independent care providers. No one should be in any doubt that when we see unacceptable behaviour, we will be prepared to challenge it and use the law to enforce our rights.”
Gemma Melhuish, People and Culture Director at HCG said: “We are thrilled the court ruled in our favour and agreed their decision was unlawful as it is important for other Care Providers to challenge decisions that are morally not correct. We are now looking forward to welcoming new starters to our Homes from our overseas recruitment campaign undertaken last year and continuing to provide high-quality care to our residents. “
THE OUTCOME AND ITS SIGNIFICANCE
The High Court granted a quashing order of the SSHD’s decision, declaring it unlawful. Aston Brooke Solicitors will now reapply for the DCoS for HCG without the commercial risks associated with the initial rejection.
being both a customer and helping the admin seems quite natural.
It is a modern philosophy of care, but moreover, it's a programme that is straight forward, tried and tested for 30 years and really works.
Its member care organisations generally become trainers for their own teams, and run it themselves.
The programme is run in person over 2-3 days or online 1 hr a wk for 7 weeks. You choose.
It addresses loneliness, helplessness and boredom and operates through 10 principles to underpin 7 critical domains of wellbeing.

Moreover, it's effective, transformational and really works. As residents, and team members wellbeing, matter so much , it's a must, in my opinion.
Geoffrey Cox Southernhealthcare.co.uk eden-alternative.co.uk"

Kashif Majeed, Head of Corporate Immigration at Aston Brooke Solicitors said, “For the care sector, the decision has significant implications. It emphasises that the Home Office must assess applications based on realistic criteria that reflect the sector's operational practices. While the SSHD can request additional information to verify the authenticity of job vacancies, it cannot impose unreasonable or unattainable requirements, particularly when those conditions do not align with the realities of the care sector.”
THE BIGGER PICTURE: IMPLICATIONS FOR THE CARE SECTOR
This case highlights the essential role that international workers play in the UK’s care sector, especially in light of the growing demand for care services due to an aging population. The judgment provides clarity for care providers seeking to hire overseas workers, reassuring them that their flexibility in staffing and contractual arrangements will be recognized.
The ruling also sets a precedent for future DCoS applications, ensuring that care providers are not burdened with unrealistic requirements. This decision affirms that decisions made by the SSHD must be grounded in the reality of the care industry, where staffing needs are often dynamic and flexible.
The King (on the Application of Hartford Care Group Limited) v. The Secretary of State for the Home Department is a major victory for the care sector, ensuring that the Home Office’s decision-making process is fair and aligned with the sector’s operational realities. The case reinforces the importance of reasonable and consistent policies in assessing DCoS applications and provides a vital precedent for care providers looking to hire international workers to meet the UK's growing care needs.
For further information on Ashton Brooke see the advert on the facing page.
Global assists clients throughout the U.K. who specialise in the healthcare sector to achieve their objectives of purchase, development and refinance.
We have organised over £1.8bn for clients in the past 30 years, providing clients with competitively priced funding to refinance existing debt, ease cashflow and develop businesses further.
From helping clients make their first purchase through to allowing groups to
grow significantly in size we assist at every stage of your business expansion. Every proposal is individual and deserves to be treated that way, so we hope you will allow us to be of assistance to you and call us to chat through your plans and requirements, I am sure we will be able to tailor a facility to your requirements.
Call us on 01242 227172 or e-mail us at enquiries@globalbusinessfinance.net


• Sponsor Licenses
• Skilled worker Visas ( Carers, Senior Carers, Nurses)
• Commercial Property, Leases, Developments, Sales & Acquisitions
• Commercial contracting & negotiating with Local Authorities regarding fees
• Refinancing
• Partnership agreements
• Dispute Resolution & Litigation
• Advice on Care Quality Commission (CQC) processes
• Assisting Care Providers to make License Applications, Registrations and Representation with CQC
• Wills, Probate & LPAs

