Provider Beliefs May Impede KT Referrals
Perceptions of nonadherence are a key issue
BY NATASHA PERSAUD
KDIGO GUIDELINES advise health care providers to refer patients on dialysis with past nonadherence to transplant centers for evaluation as possible kidney transplant candidates, yet not all qualified patients are referred, investigators reported at the 2023 American Transplant Congress in San Diego.
In some cases, providers delay referral or opt not to refer based on their idiosyncratic and subjective beliefs about patients’ nonadherence.
“We believe most providers at dialysis centers and at transplant centers want all
eligible patients referred for kidney transplantation,” said lead investigator Jenny McDonnell, PhD/MPH candidate, of Emory University’s Rollins School of Public Health in Atlanta, Georgia, who conducted the study with senior author Adam S. Wilk, PhD, and other collaborator. “The problem is that there is no clear or universal understanding of what ‘eligible’ means in this context.”
To better understand how providers respond to patient nonadherence and make transplant referral decisions, she and her team conducted a qualitative study including 39 in-depth
ED Drugs Cardioprotective
BY JODY A. CHARNOW
PHOSPHODIESTERASE-5 inhibitors (PDE5i) reduce the likelihood of major adverse cardiovascular events (MACE) in men with both coronary artery disease (CAD) and erectile dysfunction (ED), according to study findings presented at the American Urological Association’s 2023 annual meeting in Chicago.
In addition, investigators found that the cardiac benefit of PDE5i is more pronounced with tadalafil than sildenafil.
In a retrospective study of 41,287 men with CAD (but not pulmonary hypertension) and ED, Albert Ha, MD, of Columbia University’s Irving Medical Center in New York, New York, and colleagues found that men who took tadalafil and sildenafil had a significant 33% and 22% lower 5-year risk for heart failure, respectively, compared with men who received no PDE5i treatment after propensity-score matching. Tadalafil and sildenafil recipients had 25% and 12% lower 5-year risks for myocardial infarction and 41% and 35% lower 5-year risks for overall mortality, respectively.
interviews with dialysis clinic providers in Georgia, North Carolina, and South Carolina. The investigators interviewed 24 social workers, 6 nurses and nurse managers, 4 clinic managers, 3 dietitians/nutritionists, and 2 nephrologists/ medical directors.
SGF Increases Risk of Graft Failure, Death
BY JODY A. CHARNOW
SLOW GRAFT function (SGF), a less severe form of poor kidney function than delayed graft function (DGF), is independently associated with worse long-term graft outcomes and patient survival compared with immediate graft function among recipients of kidneys from living and brain-dead donors, investigators reported at the 2023 American Transplant Congress in San Diego.
“Slow graft function appears to have an important impact on longterm outcomes,” lead author Karthik Venkataraman, MBBS, of the Royal Adelaide Hospital and the University of Adelaide in Adelaide, Australia, told Renal & Urology News. “Interventions that reduce slow and delayed graft function thus could improve patientcentered clinical outcomes. Transplant registries should consider collecting and reporting on slow graft function.”
“Providers often organically brought up patient nonadherence as a barrier to transplant candidacy,” McDonnell explained. “How dialysis providers responded to patient nonadherence was affected by how they made meaning of
continued on page 13
IN THIS ISSUE
4 Cranberry products may protect against urinary tract infections
7 Surgeons are planning to perform the first human bladder transplant
8 New medications for IgAN offer promise for better outcomes
9 Statins may increase diabetes risk in kidney transplant patients
12 Post-kidney transplant AFib risk varies by dialysis modality
12 Bladder cancer progression is less likely among users of 5-ARIs
13 Febuxostat may lower the risk for CI-AKI in CKD patients
Although the adverse effect of DGF, which is the requirement for dialysis
continued on page 13 continued on page 13

SUMMER 2023 n n n VOLUME 22, ISSUE NUMBER 3 n n n www.renalandurologynews.com
The cardiac benefit is more pronounced with tadalafil than sildenafil, data show.
© TRISH233 / GETTY IMAGES
CAREGIVERS’ PERSONAL views affect how they assess transplant candidates.
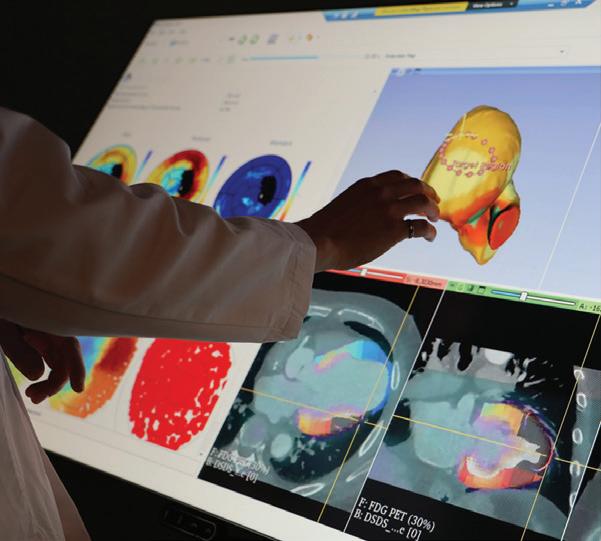
Large multi-touch interactive displays could facilitate doctor-patient communication. PAGE 16
EDITORIAL ADVISORY BOARD
Medical Director, Urology
Robert G. Uzzo, MD, MBA, FACS
G. Willing “Wing” Pepper Chair in Cancer Research
Professor and Chairman
Department of Surgery
Fox Chase Cancer Center Temple University School of Medicine Philadelphia
Urologists
Christopher S. Cooper, MD
Director, Pediatric Urology
Children’s Hospital of Iowa Iowa City
R. John Honey, MD
Head, Division of Urology, Endourology/Kidney Stone Diseases
St. Michael’s Hospital
University of Toronto
Stanton Honig, MD
Department of Urology
Yale University School of Medicine
New Haven, CT
J. Stephen Jones, MD
Chief Executive Officer
Inova Health System Falls Church, VA
Professor and Horvitz/Miller Distinguished Chair in Urologic Oncology (ret.)
Cleveland Clinic Lerner College of Medicine
Cleveland
Jaime Landman, MD
Professor of Urology and Radiology
Chairman, Department of Urology
UC Irvine School of Medicine
Orange, CA
James M. McKiernan, MD
John K. Lattimer Professor of Urology
Chair, Department of Urology
Director, Urologic Oncology
Columbia University College of Physicians and Surgeons
New York
Kenneth Pace, MD, MSc
Assistant Professor, Division of Urology
St. Michael’s Hospital
University of Toronto
Vancouver, Canada
Medical Director, Nephrology
Kamyar Kalantar-Zadeh, MD, PhD, MPH
Professor & Chief, Division of Nephrology, Hypertension & Kidney Transplantation
UC Irvine School of Medicine
Orange, CA
Nephrologists
Anthony J. Bleyer, MD, MS
Professor of Internal Medicine/Nephrology
Wake Forest University School of Medicine
Winston-Salem, NC
David S. Goldfarb, MD
Professor, Department of Medicine
Clinical Chief
New York University Langone Medical Center
Chief of Nephrology
NY Harbor VA Medical Center
Csaba P. Kovesdy, MD

Chief of Nephrology
Memphis VA Medical Center
Fred Hatch Professor of Medicine
University of Tennessee Health Science Center
Memphis
Edgar V. Lerma, MD
Clinical Associate Professor of Medicine
Section of Nephrology
Department of Medicine
University of Illinois at Chicago
College of Medicine
Chicago
Allen Nissenson, MD
Emeritus Professor of Medicine
The David Geffen School of Medicine at UCLA
Chief Medical Officer, DaVita Inc.
Denver
Rulan Parekh, MD, MS
Associate Professor of Pediatrics and Medicine
University of Toronto
Robert Provenzano, MD
Associate Professor of Medicine
Wayne State University School of Medicine
Detroit
Vice President of Medical Affairs, DaVita Healthcare
Denver
The Inescapable Reality of Financial Toxicity
More and more studies are examining how out-ofpocket health care costs such as co-payments and deductibles affect patients. These studies typically find that many patients have difficulty buying the medications they need and paying their household bills. Numerous studies on the topic were presented at the recent annual meeting of the American Society of Clinical Oncology.
In one such study of 1108 patients with cancer who received charitable co-pay assistance (CPA), Jeffrey M. Peppercorn, MD, of Massachusetts General Hospital in Boston, and colleagues found that, despite having insurance, 17% and 18% reported delays in starting therapy and skipping medical services, respectively, due to cost. Further, prior to receiving CPA, 66% believed their insurance (mostly Medicare) would shield them from paying high drug costs. Three-quarters of study participants agreed or strongly agreed that doctors should be aware of costs when making decisions.
The problem of medication affordability is especially acute for patients with cancer, but it certainly is not limited to them. A study of 80,807 adult patients with type 2 diabetes and established cardiovascular disease found that those in the highest vs lowest quartile of out-of-pocket costs were 13% and 20% less likely to initiate a GLP-1RA or SGLT2 inhibitor, respectively, according to a recent report in JAMA Network Open. The researchers, led by Jing Luo, MD, MPH, of the University of Pittsburgh School of Medicine, categorized patients into quartiles of out-of-pocket costs for a 1-month supply of these medications. The mean costs for the highest vs lowest quartile were $118 vs $25 for a GLP-1RA and $91 vs $23 for an SGLT2 inhibitor. The median delay in initiation of these drugs for the highest vs lowest quartile ranged from 3 to 6 months, according to the researchers.
Renal & Urology News Staff
Editor Jody A. Charnow
Web editor Natasha Persaud
Production editor Kim Daigneau
Group creative director Jennifer Dvoretz
Senior production manager Krassi Varbanov
Vice president, sales operations and production Louise Morrin Boyle
National accounts manager William Canning
Vice president, content, medical communications Lauren Burke
Chief commercial officer James Burke, RPh
President, medical communications Michael Graziani
Chairman & CEO, Haymarket Media Inc. Lee Maniscalco
Despite the negative impact of financial toxicity on patients, research suggests that it is often ignored in medical practices. For example, in a survey of women with early-stage breast cancer and their physicians, 50.9% of responding medical oncologists indicated that “someone in their practice often or always discusses financial burden with patients, as did 15.6% of surgeons and 43.2% of radiation oncologists,” Reshma Jagsi, MD, DPhil, of the University of Michigan in Ann Arbor, and colleagues reported in a 2018 article in Cancer
In an article published online in Renal & Urology News, Daniel D. Joyce, MD, a urologic oncology fellow at Mayo Clinic in Rochester, Minnesota, said financial toxicity, like drug toxicity, should be included in physicianpatient discussions about treatment options. “Indeed, financial toxicity has been associated with worse quality of life, symptom burden, and even survival, further supporting its inclusion in shared decision-making.”
Allowing patients’ finances to guide treatment is not ideal, but that is the reality until ability to pay is removed from the therapeutic equation.
Jody A. Charnow Editor
www.renalandurologynews.com SUMMER 2023 Renal & Urology News 1
Renal & Urology News (ISSN 1550-9478) Volume 22, Number 3. Published quarterly by Haymarket Media, Inc., 275 7th Avenue, 10th Floor, New York, NY 10001. For Advertising Sales & Editorial, call (646) 638-6000 (M–F, 9am–5pm, ET). For reprint/licensing requests, contact Customer Service at custserv@haymarketmedia.com. Postmaster: Send address changes to Renal & Urology News, c/o Direct Medical Data, 10255 W. Higgins Rd., Suite 280, Rosemont, IL 60018. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means (electronic, mechanical, photocopying, recording, or otherwise) without the prior written permission of Haymarket Media, Inc. Copyright © 2023.
FROM THE EDITOR
ONLINE
this month at renalandurologynews.com
Clinical Quiz
Test your knowledge by taking our latest quiz at renalandurologynews.com/ run-quiz
HIPAA Compliance
Read timely articles on various issues related to keeping protected health information secure.

Drug Information
Search a comprehensive drug database for prescribing and other information on more than 4000 drugs.
Job Board
Be sure to check our latest listings for professional openings across the United States.
News Coverage
Visit our website for daily reports on the latest developments in clinical research.
Nephrology
4 AE Rates Increase as CKD Progresses
Dialysis patients have higher rates of serious infections and hyperkalemia compared with nondialysis-dependent CKD patients.
12 Atrial Fibrillation Risk After a Kidney Transplant Varies by Dialysis Modality
Patients on pretransplant hemodialysis vs peritoneal dialysis are at higher risk.

12 MAKE Risk Influenced by AKI Subphenotype
According to investigators, acute kidney injury is a heterogenous clinical syndrome with varying causes, pathophysiology, and outcomes.
13 Febuxostat Cuts CI-AKI Risk in CKD
The urate-lowering drug lowered the incidence of contrast-induced acute kidney injury in a study of patients with stage 3 CKD undergoing percutaneous coronary intervention.
Urology
4 Smoking Has No Effect on OS After IO-Based mRCC Therapy
Investigators report results from a study of 989 patients treated with first-line dual immunotherapy or immunotherapy plus a VEGF-targeted therapy.
5 BCG Response Linked to Tumor Microbiome Lactobacillus bacteria may be associated with increased internalization of the immunotherapy.
6 UTUC Unlikely After MIBC Trimodal Therapy
The malignancy developed in only 2.6% of patients who received the treatment.
7 First Human Bladder Transplant Planned
The history-making procedure will be part of a clinical trial launched by urologic oncologists. Co-investigator Nima Nassiri, MD, discussed the challenges in an interview.
CALENDAR
International Continence Society
Annual Meeting
September 27-29
Toronto, Canada
ASTRO 2023 Annual Meeting
October 1-4
San Diego, CA
American Society of Nephrology
Kidney Week 2023
November 1-5
Philadelphia, PA
LUGPA Annual Meeting
November 2-4
Lake Buena Vista, FL
IKCS: North America
November 9-11
Nashville, TN
Society of Urologic Oncology
Annual Meeting
November 29-December 1
Washington, DC
Editor’s note: The 2023 conference listings below include information provided by the sponsoring organizations on their websites as this issue went to press. Departments
1
3
15
16
Contents See our story on page 7
SUMMER 2023 n VOLUME 22, ISSUE NUMBER 3
2 Renal & Urology News SUMMER 2023 www.renalandurologynews.com
Pending a successful outcome, our trial aims to enroll 5 patients for bladder transplantation. The bladders will be recovered from brain-dead deceased donors…
From the Editor Physicians cannot ignore patients’ financial toxicity
News in Brief VTE risk factors in KT recipients identified
Renal Nutrition Update Dietary approaches to treating metabolic acidosis
14
Ethical Issues in Medicine The importance of giving and receiving feedback
Practice Management
promise of interactive data visualization
The
15
Short Takes
Wireless Device to Monitor Bladder Pressure Tested
A wireless technology called UroMonitor, the first device to enable catheterfree telemetric ambulatory bladder pressure monitoring in human beings, appears safe and well-tolerated based on a trial involving 11 women.
After baseline urodynamics, the UroMonitor was inserted into the bladder transurethrally. The device did not significantly alter capacity, sensation, or flow during urodynamics, a team led by Margot S. Damaser, MD, of the Glickman Urological and Kidney Institute at Cleveland Clinic, reported in The Journal of Urology It reproduced bladder pressure, capturing 98% voiding and nonvoiding urodynamic events.
Benzbromarone Reduces
CKD Risk vs Allopurinol
Benzbromarone significantly reduced the risk for chronic kidney disease
(CKD) by 41% compared with allopurinol in a study of adult patients with asymptomatic hyperuricemia, Chiu-Shong Liu, MD, China Medical University in Taichung, Taiwan, and colleagues reported in the European Journal of Internal Medicine
Using the 2003-2015 National Health Insurance Research Database in Taiwan, the researchers propensityscore-matched 9107 benzbromarone users to 4554 allopurinol users. All patients had asymptomatic hyperuricemia and were free of gouty disorders and CKD at baseline.
Second Primary Cancer Risk
Lower With IMRT vs 3DCRT
Intensity-modulated radiation therapy (IMRT) for prostate cancer does not increase the risk for second primary cancers compared with 3D conformal radiation therapy (3DCRT), according findings published in JAMA Oncology
Using a linked database of Medicare claims and Surveillance, Epidemiology and End Results (SEER) program registries, a team led by Sara J. Schonfeld, PhD, of the National Cancer Institute in Bethesda, Maryland, studied 65,235 2-year first primary prostate cancer survivors and 45,811 5-year survivors with similar demographic characteristics. Compared with 3DCRT, IMRT was significantly associated with a 9% decreased risk for solid cancers and did not differ significantly with respect to hematologic cancers.
Kidney Transplants on the Rise
Adding CN to Immunotherapy for mRCC Improves Survival
Cytoreductive nephrectomy (CN) performed before or after immunotherapy for metastatic clear cell renal cell carcinoma (mccRCC) improves survival compared with immunotherapy alone, according to data presented at the American Society of Clinical Oncology’s 2023 Annual Meeting in Chicago.
In a study of 7367 patients identified using the National Cancer Database, immunotherapy followed by CN and CN followed by immunotherapy were significantly associated with 63% and 47% decreased risks for mortality, respectively, compared with monotherapy alone, Maroun Bou Zerdan, MD, of SUNY Upstate Medical University in Syracuse, New York, and colleagues reported in a poster presentation.
The 5-year overall survival rate was 13.0% for recipients of immunotherapy alone compared with 43.2% for patients who received immunotherapy followed by CN and 34.0% for those treated with CN followed by immunotherapy.
VTE Risk Factors in Kidney Transplant Recipients Identified
Certain kidney transplant recipients, such as those with anemia, have increased risks of venous thromboembolism (VTE), investigators reported at the 2023 American Transplant Congress in San Diego.
Investigators matched 65 recipients at their institution who experienced VTE with 65 recipients who did not by age and year of transplantation. Median patient age at transplantation was 54 years. The median time until VTE was 58 days after surgery, Basma O. Merhi, MD, of Warren Alpert Medical School of Brown University and Rhode Island Hospital in Providence, and colleagues reported. VTE was most commonly found in the lower right extremity (29.2%) and in the graft (15.4%).
The likelihood of VTE was a significant 5.0-, 4.4-, 2.8-, and 2.6-fold higher among patients who underwent a second transplant, previously received hemodialysis, had hypertension, and smoked, respectively, in unadjusted analyses. Each 1 g/dL increase in hemoglobin level was significantly associated with 28% decreased odds of VTE.
ED Visits for Gout Rose After 2010 Colchicine Price Hike
Alarge colchicine price increase in 2010 led to a rapid decrease in its use that lasted for approximately a decade, according to a recent report.
From 2011 to 2019, emergency department and adult rheumatology visits for gout significantly increased by 40% and 11%, respectively.
The FDA discontinued lower-priced versions of colchicine in 2010 after it granted market exclusivity to Colcrys for 3 years. The mean price per prescription of colchicine increased from $11.25 in 2009 to $190.49 in 2011, Zirui Song, MD, PhD, of Harvard Medical School in Boston, and colleagues reported in JAMA Internal Medicine Average out-of-pocket costs increased from $7.37 to $39.49. These costs remained high through 2019.
From 2007-2010 to 2011-2019, mean colchicine use declined significantly by 9.6 pills per patients in adjusted analyses, while allopurinol use rose significantly by 33.1 pills per patient and oral corticosteroid use by 1.5 pills per patient.
News
Please visit us at www.renalandurologynews.com for the latest news updates from the fields of urology and nephrology
in Brief
www.renalandurologynews.com SUMMER 2023 Renal & Urology News 3 Source: OPTN website: optn.transplant.hrsa.gov
The number of kidney transplants performed in the United States is on an upward trend, according to data from the Organ Procurement and Transplantation Network.
30000 20000 10000 0 25000 15000 5000 2022 2021 2020 25,500 24,670 22,817
AE Rates Increase as CKD Progresses
Researchers analyzed data from NDD-CKD and prevalent and incident dialysis patients
THE PREVALENCE OF comorbidities and adverse events (AEs) increase with chronic kidney disease (CKD) stage, especially once dialysis is initiated, a new study finds.
Using the 2004-2017 UK Clinical Practice Research Datalink, Dustin J. Little, MD, of AstraZeneca in Gaithersburg, Maryland, and colleagues identified 310,953 patients with stage 3-5D CKD based on estimated glomerular filtration rate (eGFR).
Patients with nondialysis-dependent CKD (NDD-CKD), prevalent dialysis patients, and incident dialysis patients had high baseline rates of hypertension (32.1%, 60.4%, and 61.5%, respectively) and diabetes (13.1%, 40.1%, and 41.3%, respectively), investigators reported in BMC Nephrology Comorbidities were more common, median hemoglobin values were lower, and C-reactive protein values were higher in the dialysis than non-dialysis groups. As eGFR
Cranberry Products May Stop UTIs
CRANBERRY PRODUCTS reduce the risk for symptomatic urinary tract infections (UTIs) in women with recurrent UTIs, in children, and in patients receiving interventions such as radiation therapy for bladder or prostate cancer, a recent review finds.
Elisabeth M. Hodson, MBBS, of The Children’s Hospital at Westmead in Australia, and colleagues conducted an updated systematic review of 50 randomized trials or quasi-randomized studies involving 8857 patients from multiple countries. In a metaanalysis of 26 studies, cranberry products significantly reduced the risk for symptomatic, culture‐verified UTIs by 30% compared with placebo or no treatment, the investigators reported in the Cochrane Database of Systematic Reviews Cranberry products significantly reduced the risk for UTIs by 26% in women with recurrent UTIs, 54% in children (without neurogenic bladder), and 53% in individuals susceptible to UTIs due to an intervention.
Event Rates Compared
Pneumonia/respiratory infections and urinary tract infections are among the most common adverse events in patients with nondialysis-dependent CKD (NDD-CKD) and prevalent and incident dialysis patients, with higher rates occurring in the dialysis groups.
particularly pneumonia/respiratory infection and UTI. In the NDD-CKD group, the most common AEs were pneumonia/respiratory infection (9.3) and UTI (8.2).
The hyperkalemia event rate was 0.67 per 100 person-years for the NDDCKD group compared with 4.4 and 5.0 per 100 person-years for the prevalent and incident dialysis groups, respectively. The rate of infection/sepsis was 1.0 per 100 person-years for the nondialysis group compared with 7.1 and 8.0 per 100 person-years in the prevalent and incident dialysis groups, respectively.
declined, the prevalence of comorbidities generally increased.
In the prevalent and incident dialysis groups, the most common AEs (rates per 100 person-years) were pneumonia/respiratory infection (18.0 and 19.9), urinary tract infection (UTI; 11.3
The certainty of the evidence was moderate.
Current data do not support the use of cranberry products in older adults residing in nursing homes and other long-term care facilities, patients with neuromuscular bladder dysfunction and incomplete bladder emptying, or pregnant women, Dr Hodson, editor of Cochrane Kidney and Transplant, and colleagues reported. Cranberry products included cranberry juice, tablets, capsules, or powder taken for at least 1 month. According to the investigators, cranberries contain proanthocyanidins that prevent adherence of Escherichia coli to urothelial cells lining the bladder walls. No formal proanthocyanidin dose, formulation, or regimen has been established for UTI prevention.
“This is a review of the totality of the evidence and as new evidence emerges, new findings might occur,” senior author Jonathan Craig, MBChB, PhD, vice president and executive dean of the College of Medicine & Public Health at Flinders University in Australia, stated in a news release. “In this case, the new evidence shows a very positive finding that cranberry juice can prevent UTI in susceptible people.” The investigators did not have sufficient data to determine whether cranberry products are more or less effective than probiotics or antibiotics in preventing UTI. ■
and 12.4), infection/sepsis (7.1 and 8.0), and seizure (1.05 and 1.14), respectively. Seizure occurred at a 3-fold higher rate in patients on dialysis compared with those with NDD-CKD. Overall, AE rates were higher among patients on hemodialysis than peritoneal dialysis,
“Collectively, the increased incidence of adverse clinical events likely reflects the higher comorbidity burden of patients on or transitioning to dialysis versus those with NDD-CKD,” Dr Little’s team wrote. They noted that the higher AE rates among patients on dialysis may be due to an increase in risk factors or monitoring and reporting. ■
Smoking Has No Effect on OS After IO-Based mRCC Therapy
SMOKING STATUS at diagnosis does not affect overall survival (OS) or time to treatment failure in patients with metastatic renal cell carcinoma (mRCC) receiving first-line, standard of care immune-oncology (IO) combination regimens, investigators reported at the American Society of Clinical Oncology’s 2023 Annual Meeting in Chicago.
“As opposed to other cancer types (i.e., NSCLC), current or past smoking history did not appear to be predictive of benefit from IO-based therapy,” Georges Gebrael, MD, of Huntsman Cancer Institute, University of Utah in Salt Lake City, Utah, and colleagues concluded in a poster presentation.
Using the International Metastatic Renal Cell Carcinoma Database Consortium (IMDC), the researchers identified 989 patients with mRCC treated with dual immunotherapy or immunotherapy plus a VEGF-targeted therapy in the first-line setting. Of these, 438 (44.3%), 415 (42%), and 136 (13.7%) patients were
never, former, and current smokers, respectively. The groups were similar in age, IMDC risk categories, body mass index, and sarcomatoid features.
On multivariable analysis, there were no significant differences in OS or time to treatment failure between the smoking status groups, Dr Gebrael reported on behalf of his team. At a median follow-up of 21.2 months, the OS rates at 2 years were 70.8%, 73.1%, and 62.8% for never, former, and current smokers, respectively. Median overall survival was 48.2 months, not reached, and 37.4 months, respectively. The time to treatment failure was 7.8, 7.3, and 6.4 months, respectively. The objective response rates were 40.9%, 48.5%, and 41.7%, respectively.
Former smokers had significant 1.5-fold increased odds of objective response to treatment compared with never smokers. The investigators observed no significant effect on objective response among current smokers. ■
4 Renal & Urology News SUMMER 2023 www.renalandurologynews.com
Source:
■ Pneumonia/respiratory infection ■ Urinary tract infections 9.3 8.2 18.0 11.3 19.9 12.4 Event rates per 100 person years NDD-CKD Prevalent dialysis Incident dialysis 20 15 10 5 0 Adverse
Little DJ, et al. Rates of adverse clinical events in patients with chronic kidney disease: analysis of electronic health records from the UK clinical practice research datalink linked to hospital data.
BMC Nephrol 24(1):91.
BCG Response Linked to Tumor Microbiome
Lactobacillus bacteria in patients with NMIBC increase internalization of bacillus Calmette-Guérin
 BY JOHN SCHIESZER
BY JOHN SCHIESZER
MODIFYING the bladder microbiome may improve responses to intravesical instillation of bacillus Calmette-Guérin (BCG) for the management of non-muscle invasive bladder cancer (NMIBC), according to a new study. The findings suggest that Lactobacillus bacteria may be associated with a significant increase in the internalization of BCG.
While BCG is the gold standard for the management of NMIBC, approximately 30% to 40% of patients experience treatment failure, according to investigators.
“Recently, there’s been an increased interest in the role of the urinary microbiome in numerous urologic disease processes,” said first author Zaeem Lone, a fourth-year medical student at the Cleveland Clinic Lerner College of Medicine in Ohio. “In the bladder cancer space, no study to our knowledge has looked at how the tumor intrinsic microbiome may modulate treatment response. Therefore, this study is critical to see if we can find any associations that explain preferential response to treatment.”
The researchers performed next-generation sequencing (NGS) and shotgun metagenomics on formalin-fixed bladder tumors from patients prior to intravesical BCG therapy for NMIBC. The team examined the alpha and beta diversity in 23 responders (83% male) and 24 non-responders (88% male) and found that the overall microbiome composition differed significantly as determined by both NGS and shotgun metagenomics.
The researchers defined BCG responders as patients who had no disease recurrence 2 years after induction.
“BCG is an effective treatment option for non-muscle invasive bladder cancer; however, many patients will experience cancer recurrence requiring additional and potentially more aggressive treatment. Developing a better understanding of optimizing the efficacy of BCG may allow us to improve outcomes with bladder cancer treatment,” said study co-author Nima Almassi, MD, a urologist at Glickman Urological & Kidney Institute at the Cleveland Clinic.
The researchers validated the NGS data with GFP-tagged BCG co-cultured
with a urothelial carcinoma (UC) cell line (SW780) and candidate bacteria based on the NGS data. In addition, fresh tumor samples were collected at the time of transurethral resection of bladder tumor (TURBT). Those samples were cultured under 5 different media conditions, confirming the viability of the tumor microbiome and quantifying the bacterial mass per sample.
Lone and colleagues team found that Lactobacillus species were enriched in patients who responded to BCG.
“We saw that the presence of Lactobacillus was associated with improved response,” Lone said. “In our in vitro assays to validate our sequencing data, we also observed that co-culture of Lactobacillus, BCG, and bladder cancer cells led to increased uptake of BCG into the cancer cells, which is important as internalization of BCG is the first step in engendering an immune mediated response.”
The co-culture with increasing concentrations of Lactobacillus demonstrated a significant increase in BCGGFP internalization in UCC (16%) compared with controls (6%). When the researchers examined 10 fresh tumor samples, they found that 4 samples produced viable bacteria through culture-based approaches. Tumor bacterial density was calculated at 1.25×106 colony forming units/gram of tissue.
“Utilizing next generation sequencing, we found that compositional differences do exist in the tumor microbiome of
continued on page 6
En Bloc, Standard Resection for NMIBC Compared
BY JOHN SCHIESZER
EN BLOC resection has the potential to improve outcomes in patients with non-muscle invasive bladder cancer (NMIBC) compared with standard resection, according to investigators.
In the multicenter, randomized phase 3 EB-StaR trial, which compared the surgical approaches in patients with tumors measuring 3 cm or less, researchers found that patients having an en bloc resection had a significantly lower 1-year recurrence rate (the trial’s primary outcome) compared with those undergoing standard resection (28.5% vs 38.1%).
“Bladder tumors are resected in a piecemeal manner,” said Jeremy Teoh, MD, an assistant dean and Associate Professor of Urology at The Chinese University of Hong Kong, who presented the study findings at the American Urological Association’s 2023 Annual Scientific Meeting. “It is difficult to ensure a complete and uniform tumor
resection down to the detrusor muscle layer. Therefore, residual tumor can be present even after standard resection.”
During standard resection, tumor cells float inside the bladder, Dr Teoh explained. These tumor cells can reimplant to the bladder mucosa and lead to early disease recurrence.
The 1-year progression rate was 0% in the en bloc group and 2.6% in the standard resection arm, a nonsignificant difference. The en bloc group had a significantly longer operative time compared with the standard resection group (33.4 vs 24.7 minutes).
All other outcomes were similar between the treatment arms, according to investigators. These included the detrusor muscle sampling rates, occurrence of obturator reflex, use of postoperative mitomycin C instillation, 30-day complication rate, hospital stay, and residual disease and upstaging of disease.
bloc resection, complete resection can be ascertained not only by the surgeon’s judgment, but also based on the histological assessment of the resection margins of the en bloc resected specimen.”
If en bloc was widely adopted, it could help minimize tumor fragmentation and the risk of tumor re-implantation, he said.
“I strongly believe oncological principles exist for good reasons. En bloc resection aims to uphold all oncological principles, and I am not surprised it did lead to a better oncological control,” he said.
“As urologists, we should try our best to perform high-quality surgery in order to deliver the best possible outcomes.”
For EB-StaR trial, the investigators randomly assigned 276 patients with histologically confirmed NMIBC to receive an en bloc procedure (143 patients, mean age 69.6 years, 75.5% male) or undergo standard resection (133 patients, mean age 69.1 years, 82.7% male).
“En bloc resection is a potentially superior technique in treating bladder cancer,” Dr Teoh said. “It is important to have a large-scale multicenter randomized trial to investigate whether en bloc resection can lead to a better oncological control in patients with nonmuscle-invasive bladder cancer. With en
Chad R. Ritch MD, MBA, associate professor of urologic oncology within the Desai Sethi Urology Institute at the University of Miami’s Miller School of Medicine in Florida, said the current study is notable because it could lead to increased use of en bloc in this patient
www.renalandurologynews.com SUMMER 2023 Renal & Urology News 5
Operative time is significantly longer with en bloc than standard resection.
Lactobacillus bacteria could affect the outcome of BCG therapy for NMIBC.
American Urological Association 2023 Annual Meeting, Chicago, Illinois ■ AUA 2023, Chicago © KATERYNA KON / SCIENCE PHOTO LIBRARY / GETTY IMAGES
continued
page 6
on
UTUC Unlikely After MIBC Trimodal Therapy
The malignancy developed in only 2.6% of patients who received the treatment, researchers reported
UPPER TRACT urothelial carcinoma (UTUC) seldom develops following trimodal therapy (TMT) for muscleinvasive bladder cancer, with a rate comparable to that associated with radical cystectomy, investigators reported. In addition, renal function may decline slightly in the first year after TMT, but then remains stable long-term.
Those are the findings of separate studies by investigators at Massachusetts General Hospital in Boston. TMT consists of transurethral resection of bladder tumor and radiation therapy combined with chemotherapy. It is an accepted alternative to radical cystectomy. Various chemotherapy agents used for TMT, such as
BCG response
continued from page 5
BCG responders and non-responders,” Lone said. “Particularly interesting is that in numerous other studies it’s been observed that the presence of Lactobacillus in urine is associated with a ‘healthier’ microbiome. Therefore, it was interesting to see this signature also observed in tumor tissue.”
Joshua J. Meeks, MD, PhD, an associate professor of urology, biochemistry and molecular genetics at the
En bloc vs resection
continued from page 5
population. “While it is technically feasible for smaller tumors, those cancers are generally not that aggressive, and recurrences can be managed with repeat resection and intravesical therapy without a major impact on survival,” Dr Ritch said. “What remains to be seen is whether this technique is going to be impactful in the larger more aggressive tumors where recurrences and progression can be more dangerous.”
The study was well designed and could have significant clinical implications, he said. “Randomized controlled studies like these are important because they assess novel surgical techniques in a thoughtful and meticulous manner, thereby eliminating much of the biases introduced by patient selection for one
mitomycin, 5-fluorouracil, and cisplatin, are nephrotoxic.
The studies are the first to describe the subsequent occurrence of UTUC after TMT for MIBC as well as the first to inform clinicians of the potential effect of TMT and chemoradiation on future renal function, said the senior author of both studies, Adam S. Feldman, MD, MPH, Director of Urologic Research/Vice Chair in the Department of Urology at Massachusetts General Hospital and Assistant Professor of Surgery at Harvard Medical School in Boston. The findings from these studies will better inform clinicians and patients who are considering their options for treatment of MIBC, Dr Feldman said.
Northwestern University Feinberg School in Chicago, said the role of the microbiome in the modulation of the immune system is intriguing, and now it is possible to dissect how the host, the tumor, and bacteria interact.
“We all think about profiling a tumor for a personalized medicine approach, but perhaps manipulating the microbiome is the next generation of medicine,” Dr Meeks said. “I am most impressed by their data showing that greater microbiome diversity is associated with response, rather than a single bacterial strain.
approach over the other,” Dr Ritch said. “Endoscopic resection in NMIBC has not changed over many decades, and it is important to introduce new technologies, safely, through well designed studies such as this.”
Sam S. Chang, MD, MBA, professor of urology and medicine and chief surgical officer at the Vanderbilt Ingram Cancer Center in Nashville, Tennessee, said the standard resection techniques are antiquated at best. “The authors should be applauded in performing a randomized trial to evaluate the possible beneficial impact of an en bloc resection. As with any new technique, how results will translate in real world situations is still unknown.”
While the new findings are intriguing, he noted, much larger studies with longer follow-up may help better define the benefits and risks of en bloc. “We
In a study of 271 patients who underwent TMT for MIBC and had a median follow-up of 51.8 months, Jillian Egan, MD, and colleagues found that UTUC developed in 7 patients (2.6%) following
46 months. The researchers concluded that post-TMT UTUC is “relatively rare.”
In a separate study of 287 patients who underwent TMT for MIBC and had a median follow-up of 4.6 years, Affan Zafar, MD, and colleagues found that patients’ mean estimated glomerular filtration rate (eGFR; in mL/ min/1.73 m 2) declined slightly from 65.67 at baseline to 58.43 at 1 year. The eGFR values at 3, 5, and 10 years were 55.40, 54.54, and 57.30, respectively.
completion of TMT. That rate is comparable to rates of UTUC after radical cystectomy for MIBC, Dr Feldman noted. The median time to recurrence was
There are several trials using bacteria to augment the immune response, so hopefully we will have an answer soon.”
To date, no reliable clinical markers are available to predict BCG response. Dr Meeks said there are still many other hurdles to overcome as well. Studies such as the one conducted by Lone and colleagues “are really what we should aim for,” he said. “They begin with a finding from the clinic, employ patient-involved samples, and go right to the bench for mechanism. We look forward to seeing the arc back
know for certain tumors, this technique may not be possible or the best technique,” Dr Chang said. “Careful studies evaluating our current diagnostic, therapeutic, and surveillance management are essential to escalating care when needed but also de-escalating care when appropriate.”
Roger Li, MD, a genitourinary surgeon at Moffitt Cancer Center in Tampa, Florida, said the participants had tumors measuring 3 cm or less, which is the lower end of the risk spectrum in NMIBC. “These tumors tend to be well treated with resection alone with perioperative chemotherapy infusion,” Dr Li said. “The theoretical risk of tumor cell implantation has not been definitively proven. In addition, postoperative chemotherapy administration may serve to eliminate the phenomenon of tumor cell implantation and thus
“Our data on renal function demonstrate that while there may be a slight decline in renal function in the first year after TMT, renal function should not be further affected long term,” Dr Feldman said. ■
from the bench, translating their findings to the bedside.”
Daniel P. Petrylak, MD, Chief of Genitourinary Oncology at Yale Cancer Center in New Haven, Connecticut, said the latest findings are intriguing because there is an urgent need for better treatments.
“Something as easy and cheap as affecting the microbiome is something that could clearly help patients in this situation,” Dr Petrylak said. “It certainly could be leveraged to improve treatments.” ■
abrogate this perceived risk associated with standard TURBT.”
He added that the longer operative time is not trivial, as multiple procedures are typically performed backto-back. While the study shows the feasibility of en bloc resection and that it may reduce recurrence rates in patients with small tumors, it remains to be seen how many patients would be candidates. “The inaccuracy of bladder cancer staging obtained through endoscopic resection has been well described,” Dr Li said. “En bloc resection is a method that has been proven to work well in smaller tumors, providing the anatomical specimen to the pathologist for straightforward evaluation. However, given the constraints to remove larger specimens transurethrally, the clinical impact of en bloc resection is really limited.” ■
6 Renal & Urology News SUMMER 2023 www.renalandurologynews.com
American Urological Association 2023 Annual Meeting, Chicago, Illinois ■ AUA 2023, Chicago
In the first year after TMT, kidney function declines slightly, then remains stable.
First Human Bladder Transplant Planned
Urologic surgeons Inderbir Gill, MD, and Nima Nassiri, MD, investigators with Keck Medicine of the University of Southern California in Los Angeles, have launched a clinical trial to perform the world’s first bladder transplant in a live patient. Renal & Urology News interviewed Dr Nassiri to learn more about this history-making trial and the challenges it presents.
How many patients do you plan to enroll in your trial?
Dr Nassiri: We’re starting with just 1 patient. The procedure has never been done before, and we want to make sure that the inaugural patient does well for several months after surgery to make sure it is safe and feasible. Pending a successful outcome, our trial aims to enroll 5 patients for bladder transplantation. The bladders will be recovered from brain-dead deceased donors, much the same way as kidneys and other solid organs are recovered.
Who are the intended transplant recipients?
Dr Nassiri: The subset of eligible patients is highly selective. There are 3 categories of potential patients. Broadly speaking, the ideal first patient will be someone who is on immunosuppression or in whom immunosuppression is imminent and who has terminal bladder pathology that requires cystectomy. De novo immunosuppression cannot be started in the cancer setting, so this limits the patient population.

Kidneys and other solid organs have been transplanted for decades. Why is it only now that bladder transplantation is being studied?
Dr Nassiri: The vascular anatomy of the deep pelvis area is complicated and
the procedure is technically complex. Furthermore, a unique collaboration and experience between urology and transplant surgery needs to be established. I think urologists used to be more involved in transplantation, but over the years, the transplant experience within urology has waned. This is a detriment because it’s an excellent surgical experience, especially for trainees. Perhaps the time is ripe for urologists to re-familiarize themselves with some aspects of transplantation, especially as more and more disease processes are managed non-operatively.
What preclinical research preceded the trial’s launch?
Dr Nassiri: Over the course of nearly 3 years, we have transitioned gradually, in step-wise fashion, from animal models, then to a pulsatile perfused cadaver model and, ultimately, to brain-dead but heart-beating deceased human research donors whose hearts were kept beating during the procedure.
What technical challenges, if any, have you encountered?
Dr Nassiri: The recovery of the vascularized composite bladder allograft is certainly the most challenging component. We recovered the bladder through both open and robotic approaches, and we found the robotic
approach to be instrumental in facilitating the meticulous vascular dissection in the deep pelvis. With the open procedure, we had some challenges with bleeding and poor visualization and the vascular complexity way down in the deep pelvis. This is a space that we as urologists do not normally operate in, even during a cystectomy, and developing the surgical technique took some time. Ultimately, we were able to decrease the operative time for bladder allograft recovery from 10 hours initially to just under 4.
We recovered the vascularized composite allograft—the bladder with all of its blood vessels intact—and then we prepared that specimen on the back table so there was only 1 arterial inflow and 1 venous outflow. Then we took that allograft and put it back in the body. We wanted to see if the vascular integrity would remain intact and sustained. In one of the donors, we were able to sustain them for 12 hours after the surgery. We then went back in and evaluated the
erfusion of the allograft and it looked great.
Lastly, from a logistic standpoint, the coordination of care it takes in order to perform this on a heart-beating brain-dead research donor is tremendous and takes a village to organize. It took over a year and a half to complete the studies in the brain-dead heart-beating human research donors. The organ procurement organization, OneLegacy, was instrumental in facilitating these studies.
Are there any important considerations regarding cold and warm ischemia times?
Dr Nassiri: With any kind of transplant of a solid organ, you want to limit the warm ischemia time as much as possible. We performed intravesical cooling, and we have also tried infusing ice-cold normal saline into vessels before we ligate them in order to cool the bladder down to minimize the warm ischemia time. Cold ischemia time does affect other organs, such as the kidneys, but this is generally seen beyond 12 hours of cold ischemia. Our cold ischemia times have been around 1 hour. That’s a very short cold ischemia time compared to other organs. It is unclear what the impact of this short cold ischemia time would be on the bladder.
What would be the advantages for patients?
Dr Nassiri: The primary advantage is to avoid the potential complications that can happen with urinary diversion using bowel. The gold standard for urinary reconstruction remains the use of some segment of bowel to reconstruct the bladder. However, this predisposes patients to complications, which we have all seen at some point. You can have metabolic derangements, infectious complications, leaks that can be highly morbid and sometimes fatal. These are not small things, especially in an immunosuppressed population. ■
The subset of eligible [transplant] patients is highly selective.
Continue
on controversial
Catch our discussions at www.renalandurologynews.com/home/expert-perspectives/ On The Web www.renalandurologynews.com SUMMER 2023 Renal & Urology News 7
—Nima
Nassiri, MD
the conversation online! We have many experts who weigh in
topics important to you.
New Drugs for IgAN Offer Promise of Better Outcomes
BY JOHN SCHIESZER
ALTHOUGH immunoglobulin A nephropathy (IgAN) remains incurable, clinicians can now offer patients treatments that can reduce proteinuria and potentially improve outcomes, according to a presentation at the National Kidney Foundation’s Spring Clinical Meetings in Austin, Texas.
Most recently, in February, the FDA granted accelerated approval to sparsentan (Filspari), the first non-immunosuppressive medication for treating adults with primary IgAN. In 2021, budesonide delayed-released capsules (Tarpeyo), an immunosuppressive therapy, received an FDA-approved indication for reducing proteinuria in patients with IgAN.
“For the first time, we have FDAapproved medications for the treatment of IgAN and there are clinical targets to reduce proteinuria as a means of preserving GFR [glomerular filtration rate],” said Sharon Adler, MD,
of CKD, Farxiga’s approval for CKD would extend to IgAN,” Dr Adler said. Sparsentan is an endothelin and angiotensin II receptor antagonist and is only available through a restricted distribution program called FILSPARI Risk Evaluation and Mitigation Strategies (REMS). Some endothelin
receptor antagonists have caused elevations of aminotransferases, hepatotoxicity, and liver failure. With this agent, measuring liver aminotransferases and total bilirubin prior to initiation of treatment is required.
“Clinicians in the US can take a more proactive position in diagnosing IgAN
earlier in its course so that we can treat patients earlier,” Dr Adler said. “From a research perspective, a simple diagnostic test would be a great breakthrough. Applying precision medicine principles to treatment is the next big challenge: the right drug for the right patient at the right time.” ■
Professor of Medicine at the David Geffen School of Medicine at the University of California in Los Angeles (UCLA). Dr Adler is an investigator at the Lundquist Research Institute at Harbor-UCLA Medical Center, where she is a practicing nephrologist, and Editor-in-Chief of Glomerular Diseases.
Speaking at a session on IgAN management, Dr Adler said managing IgAN presents a variety of challenges, especially staying up to date with the contemporary understanding of the disease state. New and emerging treatment options are significantly changing the treatment landscape.
“It is an exceptionally exciting time to be a nephrologist these days, since we have so many new and emerging treatment options for our patients,” Dr Adler said.
In addition to budesonide and sparsentan, clinicians also have in their armamentarium dapagliflozin (Farxiga), a sodium-glucose cotransport-2 (SGLT2) inhibitor originally approved in 2014 for treating type 2 diabetes but in 2021 received approval to prevent disease progression in patients with chronic kidney disease (CKD). “Since IgAN falls under the umbrella
8 Renal & Urology News SUMMER 2023 www.renalandurologynews.com
The recent approval of sparsentan gives physicians another management option.
Statins Increase Diabetes, Cataract Risk in KTRs
STATINS ARE WELL tolerated in kidney transplant recipients (KTRs), but the cholesterol-lowering drugs may slightly increase the risks of specific adverse events, including diabetes, data show. Investigators compared the effects of statin use and nonuse among 57,699 KTRs on Medicare from the United
States Renal Data System. Posttransplant diabetes mellitus occurred within 5 years in 43% of statin users and 35% of nonusers, Mara A. McAdams-DeMarco, PhD, of the NYU Grossman School of Medicine in New York, and colleagues reported in the Clinical Journal of the American Society of Nephrology
The incidence rates of cataracts (22% vs 12%), hemorrhagic stroke (1.9% vs 1.4%), and rhabdomyolysis (1.5% vs 0.9%) were also higher among statin users. Liver injury occurred in a lower proportion of statin users (2% vs 3%). In multivariable analysis, statin use was significantly associated with a 12%
higher risk of posttransplant diabetes mellitus, a 22% higher risk of cataracts, and a 37% higher risk of rhabdomyolysis. Statin use was significantly associated with an 18% lower risk of liver injury. Use of the drugs was not associated with hemorrhagic stroke. These associations did not differ by statin type. ■
www.renalandurologynews.com SUMMER 2023 Renal & Urology News 9
Metformin for PTDM Found to Lower CAD Risk
METFORMIN LOWERS the risk for coronary artery disease in kidney transplant patients with posttransplant diabetes mellitus (PTDM), researchers reported at the 2023 American Transplant Congress in San Diego. In a study that enrolled 1663 kidney transplant recipients without preexisting
diabetes mellitus, PTDM developed in 634 (38.1%). Of these, 406 (64%) received treatment with metformin, Jae Lee, MD, of Asan Medical Center in Seoul, South Korea, and colleagues reported. Metformin use was significantly associated with a 76% lower risk for percutaneous coronary intervention
(PCI) compared with nonuse. Longterm use of metformin (1192 days [median value] or more) was significantly associated with a 78% lower risk for PCI and 55% lower risk for graft failure compared with fewer than 1192 days of use. In a subgroup given tacrolimus, metformin use was significantly associated
with a 76% and 65% lower risk for PCI and graft failure, respectively. Metformin had a renoprotective effect in this subgroup, with users experiencing a significantly slower annual decline in estimated glomerular filtration rate compared with non-users (−0.053 vs −1.31 mL/min/1.73 m2). ■
10 Renal & Urology News SUMMER 2023 www.renalandurologynews.com
CVD, Diabetes Up Hospitalization Risk for LKDs
LIVING KIDNEY donors (LKDs) may have increased risks for end-stage kidney disease (ESKD) following nephrectomy. New study findings presented at the 2023 American Transplant Congress in San Diego, add that LKDs with diabetes or cardiovascular disease — risk factors for ESKD and its sequelae — are more
likely to be hospitalized after donation. Amy Chang, MD, of Johns Hopkins University School of Medicine in Baltimore, Maryland, and colleagues studied postdonation hospitalization records from 2265 LKDs who underwent nephrectomy from 1968 to 2019. Median age at donation was 46 years.
Hospitalization within a median 7 years affected 42% of donors. The most common reasons for hospitalization were surgery (59%), cardiovascular causes (16%), and urologic problems (6%). The investigators predicted that up to half of living kidney donors would eventually experience hospitalization following
nephrectomy. After adjusting for clinical characteristics, cardiovascular and diabetes history in the donor were significantly associated with 1.5- and 2.2-fold increased odds of hospitalization, the investigators reported. Hospitalization was not associated with patient sex, smoking history, education level, or income.
Hospitalization of living kidney donors may be “a sentinel event” for adverse outcomes, according to Dr Chang and colleagues.
“Since diabetes is the leading cause of [ESKD] in this population and cardiovascular disease is the leading cause of death in an [ESKD] population, hospitalization in donors presents a crucial opportunity to avert the most adverse long-term outcomes described in this population.” ■
Black LKDs Have Higher HTN Risk
HYPERTENSION IS more likely to develop in Black vs White living kidney donors (LKDs), investigators reported at the National Kidney Foundation’s 2023 Spring Clinical Meetings in Austin, Texas.
Using data from the Scientific Registry of Transplant Recipients, Ekamol Tantisattamo, MD, MPH, of the University of California Irvine in Orange, California, and colleagues retrospectively studied 174,359 LKDs who donated a kidney from June 1972 to September 2022. The cohort had a mean age of 41 years, and 70% were White, 11% Black, 13% Hispanic, and 3% Asian.
The incidence rate of systolic hypertension (130 mm Hg or higher) was 0.02 person-months. On multivariate analysis that adjusted for age, gender, predonation obesity status and other potential confounders, Black donors had a significant 17% higher risk for systolic hypertension compared with White donors, the investigators reported in a poster presentation. Asian donors had a significant 15% lower risk for systolic hypertension compared with White donors. Other races and ethnicities had no significant difference in risk. ■
www.renalandurologynews.com SUMMER 2023 Renal & Urology News 11
Atrial Fibrillation Risk After a Kidney Transplant Varies by Dialysis Modality
Likelihood of the arrhythmia is higher with HD compared with PD
BY JODY A. CHARNOW
HEMODIALYSIS (HD) vs peritoneal dialysis (PD) prior to a first kidney transplant is associated with a higher risk for newly diagnosed atrial fibrillation, investigators reported at the 2023 American Transplant Congress in San Diego, California.
Risk Increased by 18%
Patients who had been on HD had a significant 18% increased risk for atrial fibrillation compared with those who had been on PD, after adjusting for multiple variables, Leonardo Pozo Garcia, MD, of Baylor College of Medicine in Houston, and colleagues reported.
Using data from the US Renal Data System, United Network for Organ Sharing, and Medicare parts A and B, Dr Pozo Garcia’s team studied 43,621 adult patients undergoing their first kidney transplant and who did not have previously diagnosed atrial fibrillation. Prior to transplantation, 37,055 patients received HD and 6566 received PD. Patients had a mean age of 51 years. The investigators identified other risk factors for posttransplant atrial
fibrillation. Graft failure and receiving a kidney from a female vs male donor were significantly associated with a 2.8fold and 1.1-fold increased cause-specific risk for atrial fibrillation, respectively. Receiving a kidney from a living donor was significantly associated with a 25%
Study identifies transplant factors that increase atrial fibrillation risk.
lower cause-specific risk. A 4-6 vs 0 mismatch was significantly associated with a 26% increased cause-specific risk. In addition, each 1 year on dialysis was significantly associated with a 5% increased cause-specific risk for atrial fibrillation.
Implications for Risk Stratification
“In our study, we found that patients on hemodialysis prior to transplantation were at increased risk of developing new-onset post-kidney transplant atrial fibrillation as compared to patients
5-ARIs May Prevent BC Progression
who were on peritoneal dialysis,” Dr Pozo Garcia told Renal & Urology News. “Both classic atrial fibrillation and transplant-related risk factors play a role in the development of posttransplant atrial fibrillation. As our understanding of transplant-specific risk factors for atrial fibrillation increases, we may be able to better risk-stratify the kidney transplant population and develop monitoring and management strategies that can improve outcomes.”
The study population was 60.8% male, 55.6% White, and 35.8% Black. With respect to comorbidities, 30.3% of patients had diabetes, 25.2% had heart failure, 29.9% had coronary artery disease, and 4.3% had arrhythmias other than atrial fibrillation.
The authors noted in their poster presentation that new-onset atrial fibrillation develops in 7% of kidney transplant recipients within the 3 years following transplantation. The link between pretransplant dialysis modality with new-onset atrial fibrillation in patients receiving their first kidney transplant has not previously been studied, according to the investigators. ■
MAKE Risk Influenced by AKI Subphenotype
INVESTIGATORS have identified
2 distinct acute kidney injury (AKI) subphenotypes with different risks for major adverse kidney events (MAKE). The subphenotypes may improve risk stratification beyond using serum creatinine concentrations alone.
“Acute kidney injury (AKI) is a heterogeneous clinical syndrome with varying causes, pathophysiology, and outcomes,” Pavan K. Bhatraju, MD, MSc, of the University of Washington in Seattle, and colleagues explained. “We incorporated plasma and urine biomarker measurements to identify AKI subgroups (subphenotypes) more tightly linked to underlying pathophysiology and long-term clinical outcomes.”
In the ASSESS-AKI Study (Assessment, Serial Evaluation and Subsequent Sequelae), the investigators analyzed 29 clinical, plasma, and urine biomarkers associated with AKI development and identified 2 classes of patients. Class 1
patients had higher rates of preexisting congestive heart failure and lower concentrations of plasma inflammatory and urinary tubular injury biomarkers. Class 2 patients had higher rates of preexisting chronic kidney disease (CKD) and higher concentrations of biomarkers.
The investigators matched and compared 769 hospitalized adults with and 769 without AKI. The long-term risk for MAKE was 2.1- and 3.0-fold higher for patients with AKI class 1 and 2, respectively, compared with patients without AKI, Dr Bhatraju and colleagues reported in the American Journal of Kidney Diseases. The class 2 AKI group had a 1.4-fold increased risk for MAKE compared with the class 1 group, after adjustment for KDIGO AKI stage and other factors.
The higher risk of MAKE among class 2 patients was explained by a higher risk for CKD progression and dialysis, according to the investigators.
The risk for CKD progression was a significant 3.0-fold higher with class 2 compared with class 1 AKI. The risk for dialysis initiation was a significant 4.6-fold higher with class 2 vs 1. Patients with AKI class 1 or 2 had significantly increased risks for CKD development and early death compared patients without AKI.
“Key variables that differentiated the AKI subphenotypes included host response markers of inflammation, such as sTNFR-1, IL-6, IL-10, and urinary markers of tubular injury and inflammation, such as urinary NGAL and IL-18,” Dr Bhatraju’s team wrote. Serum creatinine ranked 20th out of the 29 variables for differentiating classes 1 and 2. Urine output data were not available, which is a study limitation.
Class 2 patients may benefit from closer follow-up for early signs of CKD progression, according to the researchers. ■
USE OF 5α-reductase inhibitors (5-ARIs) prior to a bladder cancer diagnosis may reduce patients’ risk for disease progression.
Using the Korean National Health Insurance Service database, investigators identified 22,845 men diagnosed with bladder cancer who had preexisting benign prostatic hyperplasia (BPH) treated with an α-blocker with or without a 5-ARI. To reduce biases, they propensity-score matched 5300 users of α-blockers only to 5300 users of 5-ARIs plus α-blockers. BPH medications were required to be taken 12 or more months before bladder cancer diagnosis.
The 5-ARI plus α-blocker group had a significant adjusted 16% and 26% lower risk of bladder instillation and radical cystectomy, respectively, compared with the α-blocker only group, indicating delayed grade and stage progression with 5-ARI use, Seok Ho Kang, MD, PhD, of Anam Hospital, Korea University College of Medicine, in Seoul, Korea, and colleagues reported in JAMA Network Open. The 5-ARI group also had a significant 17% reduced risk for allcause mortality.
The between-group differences in restricted mean survival time were 88.1 days for bladder instillation, 68.0 days for radical cystectomy, and 92.6 days for all-cause mortality.
The investigators also found that the 5-ARI plus α-blocker group had numerically lower incidence rates per 1000 person-years of bladder instillation (66.43 vs 85.59) and radical cystectomy (13.56 vs 19.57) compared with the α-blocker only group.
The investigators also found that only 5-ARI use of 2 years or more was significantly associated with reduced risk of radical cystectomy.
“This cohort study found that the prediagnostic prescription of a 5-ARI was associated with a reduced risk of [bladder cancer] progression,” Dr Kang’s team wrote. “However, the evidence was insufficient to inform the extension of 5-ARI indications.” ■
12 Renal & Urology News SUMMER 2023 www.renalandurologynews.com
KT referrals
continued from page 1
nonadherence, based on their beliefs about its causes and implications. Their beliefs ultimately informed their decisions about referring patients for transplant evaluation.”
The investigators identified 3 themes from provider interviews. First, nonadherence to dialysis treatments, medical appointments, dietary advice, medications, weight loss regimens, wound care, or communication signaled to some providers that a patient was a “risky” rather than “good” candidate for transplant. Perceived reasons for patient nonadherence included socioeconomic factors, comorbidities, and lack of motivation. Second, providers considered the implications of nonadherence. They were concerned about wasting their limited time and resources, their emotional expenditure, a possible negative response from the transplant center, and the potential loss of a valuable and scarce kidney to a “risky” patient.
ED drugs cardioprotective
continued from page 1
Further, compared with sildenafil recipients, tadalafil-treated patients had significant 15%, 14%, and 15% lower 5-year risks for heart failure, myocardial infarction, and overall mortality, respectively.
“I think our study is the first to tease out specific differences among individual PDE5i in relation to cardiac outcomes, with our preliminary results suggesting that tadalafil may be superior to other PDE5i like sildenafil in relation to heart failure, myocardial infarction, and mortality,” Dr Ha told Renal & Urology News. “Since erectile dysfunction is a common harbinger for cardiac disease later in life, it is important for patients to understand what drugs may best address their medical issues, especially in a time when medical care may
Slow graft function
continued from page 1
within 7 days after transplantation, on long-term graft outcomes is well documented, it has been unclear whether SGF (poor kidney function not requiring dialysis) also leads to worse graft outcomes, Dr Venkataraman explained.
He and his colleagues studied 17,579 adult kidney-only transplant recipients from 2001 to 2021 in the Australia and New Zealand Dialysis
Third, providers’ beliefs about whether a patient would be invested in the transplant process affected their decision to delay, deny, or proceed with transplant referral. Providers’ responses were highly individual.
“Dialysis providers have varying understandings of their role in assessing patients,” McDonnell explained. “Where there is any gap between providers’ perceptions of the reasons and
measures of nonadherence to transplant outcomes and sharing these measures with the dialysis and transplant provider communities for decision-making.
Addressing providers’ misperceptions and apprehension may also help, McDonnell added. She noted that previous studies on implicit bias in medical decision-making have shown that racial and ethnic minorities, lowincome patients, and other marginalized patients are less likely to receive preferred medical treatments.
Febuxostat Cuts CI-AKI Risk in CKD
implications of nonadherence and the true reasons and implications, patients’ access to kidney transplantation may be impeded.”
Researchers can provide useful information to fill the gap, she said, by linking clearly defined and internally valid
be siloed in different (and oftentimes disconnected) specialties. “
As for the greater cardiac benefit observed with tadalafil, Dr Ha said, “We speculate that this may be due to differences in pharmacokinetics, with tadalafil offering more specific inhibition of PDE5 enzymes with less cross reactivity, as well as a longer duration of efficacy. As such, this may promote medication compliance, particularly in patients with both ED and CAD. However, our results are preliminary, and as such, we cannot definitely conclude that clinicians should preferentially prescribe tadalafil until additional research is performed.”
The study population included 12,214 sildenafil users, 6751 tadalafil users, and 22,321 men who received no treatment. Dr Ha’s team performed propensity-score matching using baseline
and Transplant Registry. The study population included 5904 recipients of living-donor kidneys, 9316 recipients of brain-dead donor kidneys, and 2359 recipients of kidneys donated following circulatory death. The investigators followed patients for a median of 7.3 years.
SGF in recipients of living-donor kidneys increased their risk for graft failure and death by 1.5- and 1.6-fold, respectively, in adjusted analyses, Dr Venkataraman reported. Among recipients of kidneys from brain-dead donors, SGF significantly increased the
McDonnell acknowledged that providers are constrained by time and resources. “Affording social workers and other dialysis providers the time and resources needed to support these patients may require reallocating tasks and providing for additional time and staff resources, prioritizing interventions that uncover and address the real reasons for patient nonadherence. Such efforts and interventions could help improve adherence among patients, and in the long term, increase rates of patient referral, waitlisting, and transplant receipt.” ■
comorbidities of hypertension, ischemic heart disease, cerebral infarction, diabetes, and hyperlipidemia.
The association between PDE5i therapy and lower MACE risk also was demonstrated in a retrospective, observational cohort study published in The Journal of Sexual Medicine in January. The study, by Robert A. Kloner, MD, PhD, of Huntington Medical Research Institutes in Pasadena, California, and colleagues, included 72,498 men with ED and no prior MACE within the previous year identified using a claims database. Of these, 23,816 had at least 1 claim for a PDE5i (exposed group) and 48,682 did not (unexposed group). On multivariable analysis, the exposed group had a significant 13% lower risk for MACE, 39% lower risk for cardiovascular death, and 25% lower risk for overall mortality compared with the unexposed group. ■
risk for graft failure by nearly 1.2-fold, but did not influence patient survival. SGF was not significantly associated with graft or patient survival among recipients of kidneys from circulatorydeath donors.
DGF significantly increased the risk for graft failure by approximately 2.1-, 1.4-, and 1.7-fold in recipients of kidneys from living donors, brain-dead donors, and circulatory-death donors, respectively, and significantly increased the risk for patient death by approximately 2.0-, 1.4-, and 1.5-fold, respectively. ■
Febuxostat reduces the risk for contrast-induced acute kidney injury (CI-AKI) in patients with stage 3 chronic kidney disease (CKD) undergoing percutaneous coronary intervention (PCI) for acute coronary syndrome. In a trial, investigators randomly assigned 120 patients to receive traditional treatment with intravenous hydration and N -acetylcysteine with and without the addition of febuxostat. Each group had 60 patients. The intervention group received 80 mg febuxostat 6-18 hours before and after PCI and stenting with 24 hours in between doses.
CI-AKI occurred in a significantly lower proportion of the febuxostat than control group: 11.7% vs 25.0%, Nahla Mohamed Teama, MD, of Ain Shams University in Cairo, Egypt, and colleagues reported in BMC Nephrology. They noted that no serious adverse reactions occurred in the febuxostat group.
Serum uric acid levels did not change significantly from baseline to 3-5 days after contrast exposure in either group, but urea and serum creatinine levels rose significantly higher in the control group. In multivariate analysis, only febuxostat nonuse, baseline serum creatinine, and high Mehran score predicted contrastinduced AKI. The Mehran Score gives points for hypotension, use of an intraaortic balloon pump, congestive heart failure, age older than 75 years, anemia, diabetes, contrast media volume, and estimated glomerular filtration rate less than 60 mL/min/1.73m2
Despite the limited studies regarding the use of febuxostat to protect against CI-AKI among CKD patients, “we recommend its use in CKD stage 3 patients, especially patients with hyperuricemia,” the investigators wrote. “We recommend using risk scores for acute kidney injury before giving contrast to CKD patients to stratify the patients and individualize contrast type, volume and preventive measures according to the results of these scores.” ■
www.renalandurologynews.com SUMMER 2023 Renal & Urology News 13
Researchers zero in on why caregivers perceive patients as nonadherent.
Renal Nutrition Update
Treating metabolic acidosis with nutritional interventions can decrease the risk for kidney disease progression
BY LINDSEY ZIRKER, MS, RD, CSR
Nephrology providers are used to looking at multiple ways to preserve kidney function, such as managing hypertension and blood sugar levels and using medications to reduce proteinuria and ameliorate cardiovascular problems. For many patients, however, kidney function continues to deteriorate and progress to kidney failure. This could be due to modifiable risk factors that clinicians fail to identify and address. Metabolic acidosis is one of them.
Metabolic Acidosis Undertreated
Metabolic acidosis, defined as serum total CO 2 concentration less than 22 mmol/L, is estimated to be present in about 27.6% of those with CKD stage 4 and 46.4% of those with stage 5 CKD.1 Metabolic acidosis is associated with poor outcomes in those with CKD, such as bone demineralization, muscle wasting, hormone imbalance, hyperkalemia, failure to thrive, malnutrition, increased risk of falls or fractures, and increased progression of CKD.2,3 Despite this, it is estimated that only 17% of patients receive treatment for metabolic acidosis.4 There are clear targets and interventions for correcting metabolic acidosis.
that may be more appropriate for some patients or may be used successfully in addition to sodium bicarbonate.
NEAP Reduction Through Diet
Multiple studies show that reducing net endogenous acid production (NEAP) can help to improve or correct metabolic acidosis. 2,5 Dietary components such as phosphorus and protein are acidforming in the body, whereas potassium, calcium, and magnesium

which can deplete the body’s stores. Highly motivated patients can keep electronic food logs that can estimate mineral intake and a diet’s potential renalacid load. A renal dietitian can review these logs to help the patient make food choices that support a lower acid load as well as adequate alkalizing minerals. In some cases, supplements may be appropriate to ensure adequate nutrition and good food quality of life because magnesium and calcium from plant sources are not as well absorbed.
Multiple Benefits
Research indicates that correcting metabolic acidosis through dietary changes can provide a multitude of benefits: increased insulin sensitivity, improved muscle mass growth, increased protein reserves, slower progression of kidney disease, reduced inflammation, improved lipid profiles and blood pressure, and reduced pill burden from sodium bicarbonate.2,5,7,8
Correcting metabolic acidosis is another tool for providers to help slow the progression of kidney disease. Including dietary changes (and dietitians) as an intervention for metabolic acidosis provides additional benefits that can support the patient’s health on multiple levels. ■
Lindsey Zirker, MS, RD, CSR, is a renal dietitian and Director of Clinical Services for the Kidney Nutrition Institute in Titusville, Florida. She specializes in autoimmune kidney disease and advanced practice medical nutrition therapy for people with kidney disease.
REFERENCES
1. Kim HJ. Metabolic acidosis in chronic kidney disease: Pathogenesis, clinical consequences, and treatment. Electrolyte Blood Press. 2021;19(2):29-37.
2. Noce A, Marrone G, Wilson Jones G, et al. Nutritional approaches for the management of metabolic acidosis in chronic kidney disease. Nutrients. 2021;13(8):2534.
The KDOQI (Kidney Disease Outcomes Quality Initiative program) guidelines recommend a serum bicarbonate level between 2426mmol/L.5 Sodium bicarbonate is a common and effective treatment for metabolic acidosis, but there are nutrition interventions
are more alkalizing.2 Following a lowprotein diet or a diet richer in plant proteins naturally reduces the amount of phosphorus and protein, thus reducing NEAP. Without careful planning, however, these diets can still be low in potassium, magnesium, and calcium,
While all these approaches may not be the perfect option for every patient, a survey of CKD patients found that 43% of patients felt that they were capable of making lifestyle changes to reduce complications of CKD and 32% of patients indicated that they would be interested in being referred to see a dietitian.6 The dietitian can work with the patient individually to assess the best way to help them make changes.
The key is for the patient to know that they have options to make dietary changes or to see a dietitian to slow the progression of their kidney disease.
3. Mathur V, Reaven NL, Funk SE, et al. Association of metabolic acidosis with fractures, falls, protein-calorie malnutrition and failure to thrive in patients with chronic kidney disease. Clin Kidney J. 2022;15(7):1379-1386.
4. Whitlock RH, Ferguson TW, Komenda P, et al. Metabolic acidosis is undertreated and underdiagnosed: a retrospective cohort study. Nephrol Dial Transplant. Published online ahead of print Nov. 2, 2022.
5. Ikizler TA, Burrowes JD, Byham-Gray LD, et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am J Kidney Dis. 2020;76(3 Suppl 1):S1S107. [Erratum published in Am J Kidney Dis. 2021 Feb;77(2):308].
6. Jimenez EY, Kelley K, Schofield M, et al. Medical nutrition therapy access in CKD: A cross-sectional survey of patients and providers. Kidney Med. 2020;3(1):31-41.
7. Goraya N, Narayanan M, Wesson DE. Management of metabolic acidosis in chronic kidney disease: Past, present, and future direction. Adv Chronic Kidney Dis. 2022;29(4):416-423.
8. Scialla JJ, Anderson CA. Dietary acid load: a novel nutritional target in chronic kidney disease? Adv Chronic Kidney Dis. 2013;20(2):141-149.
Renal & Urology News will be covering the American Society of Nephrology’s Kidney Week 2023 conference in Philadelphia, PA, November 2-5. Go to www.renalandurologynews.com for daily reports on noteworthy studies.
14 Renal & Urology News SUMMER 2023 www.renalandurologynews.com
Multiple studies show that reducing net endogenous acid production can help to improve or correct metabolic acidosis.
Diets rich in plant protein may correct metabolic acidosis in patients with kidney disease.
© HUIZENG HU / GETTY IMAGES
News
Upcoming
Ethical Issues in Medicine
BY DAVID J. ALFANDRE, MD, MSPH
Last year, I had just finished a frustrating early morning tennis match with my tennis partner. I had not played up to my expectations, was not executing my shots, and felt like I should be playing better. I don’t even remember the score, just that I had played poorly and that it was a disappointing start to my busy workday. On the car ride home, unsolicited, my tennis partner remarked on my game and described elements that could be improved. I was ornery but still confident when I told him, “I didn’t ask you for feedback.” To which he replied, “I’m not giving you feedback, I’m giving you criticism,” which made us both laugh and actually had the intended effect of moving me out of my funk and on to more productive thoughts to begin my day.
This exchange reminded me of the power and value of feedback and the challenges of giving it. From an ethics perspective, giving and receiving feedback are central to quality improvement at both an individual and institutional level. Health care professionals don’t work in a vacuum: They rely on their colleagues to help them continually improve outcomes for patients. Feedback given to patients helps them learn and improve their health. Feedback from patients (often through standardized postvisit surveys) is a central part of the institutional quality improvement process.
Base Feedback on Observed Behavior
There is an ever-expanding literature on how to give thoughtful, effective, and empathic feedback,1,2 including evidence-based techniques to help people learn, grow, and develop to become competent, kind, ethical, health care professionals. When giving feedback, it’s important to do so with adequate privacy. Most people struggle to incorporate feedback in a public setting in front of watchful eyes of others. Feedback should be timely, concrete, actionable, and based on an observation of behavior, not directed at the person, their personality, or other characteristics. For example, saying, “During that last encounter, I noticed that you

interrupted the patient multiple times,” is far preferable to, “You seem like an impatient person.” The former focuses on recently observed behavior and can be intervened on, while the latter is likely to feel like a personal attack. Finally, feedback should be given with humility.
A Challenge to Sense of Identity
How to effectively and respectfully receive feedback is the second half of the feedback equation and arguably more complicated. The fundamental challenge that often interferes with fully embracing this important concept is that while many of us understand that feedback can help us to continually learn and develop personally and professionally, it can also feel unsettling and challenge our sense of self. We want to learn and grow, but we don’t want to get hurt.
As my tennis partner demonstrated, we don’t always get to control when and where feedback comes from. It can come unexpectedly or without permission. Therefore, we should be prepared for how we’re going to manage it including setting boundaries when appropriate. The highly readable and useful book, Thanks for the Feedback: The Science and Art of Receiving Feedback Well, provides both a conceptual
like talking about it. Thanks for coming out this morning. I’m looking forward to next week.” This is more likely to prompt a supportive comment from him even if his joke was effective and well-timed. Maybe I’ll be ready for feedback the following week.
Consider the Source
There are other points to consider. Just because someone speaks up about your behavior, doesn’t mean they are
Be Clear About Intent
One overarching strategy to address these challenges is to be clear about the intent of the feedback before giving it. Will the feedback be designed to support the learner and highlight what they are doing well, or will it also be used to honestly identify areas for improvement?
Giving and receiving feedback is essential to all of us in the health care profession. Without good information from our colleagues and patients, it becomes much harder to learn, grow, and continually improve. This requires specific skills — skills that can be learned, practiced, and taught. ■
framework for approaching this issue and tips for making it work.3
Feedback may challenge our sense of identity, threatening to undermine our belief in ourselves. We may not be ready to hear what others have to say about our behavior. Or if the feedback is not executed thoughtfully, we may not want the commentary. Perhaps I could have preempted my tennis partner’s comments by letting him know as we left the court, “I felt like I wasn’t playing my best and I don’t really feel
right. Sometimes, how we respond to feedback may depend more on the person giving it than the content of the feedback. One’s reaction may be more a function of that particular relationship rather than the validity of what they’re saying. Further, feedback from one’s spouse may elicit a different reaction than feedback from one’s colleague at work. For all of these scenarios, recognizing our initial triggers to the feedback provide the right foundation to use the information productively.
David
J. Alfandre, MD, MSPH, is a health care ethicist and an Associate Professor in the Department of Population Health at the NYU School of Medicine in New York. The views expressed in this article are those of the author and do not necessarily reflect the position or policy of the VA National Center for Ethics in Health Care or the US Department of Veterans Affairs.
www.renalandurologynews.com SUMMER 2023 Renal & Urology News 15 © PM IMAGES / GETTY IMAGES
10.1089/jpm.2010.0093
REFERENCES 1. Thomas JD, Arnold RM. Giving feedback. J Palliat Med. 14.2 (2011): 233-239. doi:
2. Bottles K. Tossing hand grenades: how to deliver feedback in medicine today. Physician Exec. 2006 Sep-Oct;32(5):32-37. 3. Stone D, Heen S. Thanks for the Feedback: The Science and Art of Receiving Feedback Well. Viking. 2014.
Without good information from our colleagues and patients, it becomes much harder to learn, grow, and continually improve.
Giving and receiving feedback is central to quality improvement at both an individual and institutional level
Feedback from colleagues can help health care providers improve patient outcomes.
Practice Management
Technological advances promise to elevate telemedicine to a new level with interactive data visualization
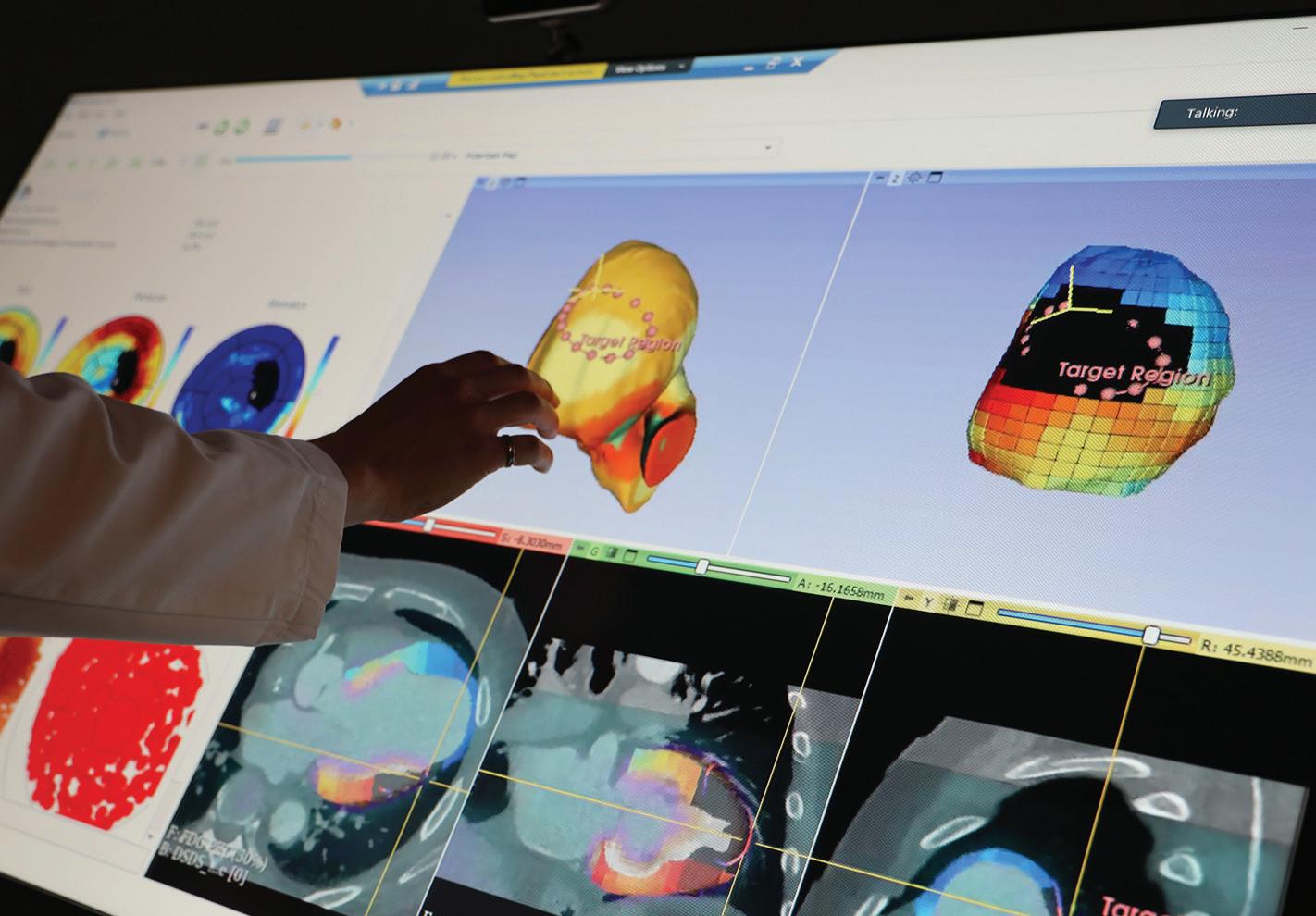 BY JOHN SCHIESZER
BY JOHN SCHIESZER
Development of more sophisticated technologies involving large multi-touch displays could transform the way doctors and patients communicate by telemedicine. Instead of remaining passive recipients, patients could provide more data when appropriate and play a more active role in the healing process. Additionally, patients may retain health information more readily if it’s shared in a visual way.
Fateme Rajabiyazdi, PhD, an assistant professor in the Department of Systems and Computer Engineering at Carleton University in Ottawa, Canada, is part of a Canadian team developing health information visualization software for large, multi-touch displays. These displays can be positioned upright like a television, or at the touch of a button, slide flat like a table. It’s a hardware and software innovation with the potential to improve communication between patients and health care professionals and foster more collaborative, datadriven decisions.
Decision-Making Support
“We need to change the way clinical offices and the communication dynamic in a clinic occur,” Dr Rajabiyazdi said. “One solution to address these challenges is to bring
functionality. They also can accommodate interaction by multiple users and different mediums. Users can touch with gloves or ungloved fingers as well as pens, allowing many people to work simultaneously.
More Patient Involvement
“With our proposed technology, patients can look at their whole data and get involved in their care,” Dr Rajabiyazdi said. “By having patients involved in their care, we can expect to have more effective data communication, which can improve patient knowledge, cultivate a shared understanding of treatment plans and care decisions between patients and their clinicians, and increase patient agency and compliance with treatment plans, thus resulting in fewer medical errors and better patient health outcomes.”
Many new apps and platforms are available, but it’s challenging to integrate them because clinicians are busy and patients can be in a vulnerable situation, Dr Rajabiyazdi said. With the rise of self-monitoring devices for blood pressure and glucose levels, as well as Fitbits and other gadgets that record things such as heart rate and calories burned, people increasingly have an array of data that could inform their
affordable, pleasant, and even effective,” Dr Dorn said. “But it all depends on the context and reason for care. Patients with certain conditions should be evaluated in person.”
Potential Uses
Anne Chiang, MD, PhD, a member of National Comprehensive Cancer Network’s Guidelines Panel for Small Cell Lung Cancer and an associate professor at Yale Cancer Center/Smilow Cancer Hospital in New Haven, Connecticut, said the challenge with the latest technology is how best to integrate it into the regular workflow.
visualization may replace, in a very cool way, physicians drawing diagrams and mapping out plans, but the most important thing is a health care worker who wants to communicate and can communicate in language that the patient can understand,” said Catherine Clase, MB, BChir, MSc, professor of medicine at McMaster’s University in Montreal, Canada. “Accessing a video or using an interactive website is very useful for many patients but requires a degree of digital literacy that older patients or those with cognitive impairment may lack.”
technology to facilitate patient-clinician communication. We expect our interactive large tabletop and interactive health data visualization technologies will support patients in clinical decision-making. The design of these technologies will be done by having patients in the loop to make sure patients find it useful and easy to use.”
With recent advances in technology, the displays can have fast, accurate, reliable, robust, and unlimited touch
diagnoses and treatment plans. But it needs to be meshed with the test results and other risk factors.
Spencer Dorn, MD, MPH, vice chair of the Department of Medicine and a professor in the Division of Gastroenterology and Hepatology at The University of North Carolina at Chapel Hill, said some patients like telemedicine and want to continue using it. “Telemedicine is a channel that can make care more accessible,
“It would be great to show my patients large clinical study data,” Dr Chiang said. “Now, I have to click through all the data. It would be nice to have a display of how their tumor started and how it shrank. It would be nice to show them in a 3D form. That would be fantastic.” Dr Chiang noted that costs and training could be barriers to adoption. “You have to know how to troubleshoot when something doesn’t work for the patients,” Dr Chiang said.
The physician entering data is a frequent problem with electronic medical records because clinicians are more focused on entering data than examining and listening to the patient.
“This novel interactive health data
If telemedicine is more than a phone call or video call, it could include home blood pressure monitoring by the patient or caregiver, or a physical exam by a health care worker in the patient’s home, according to Dr Clase. Clinicians could in real-time download data from continuous glucose monitoring or analyze photos of wounds. This could be coupled with devices that detect atrial fibrillation or hyperkalemia. “For these new technologies, we will need to look at clinical effectiveness and cost-effectiveness as rigorously as if we were talking about drugs,” Dr Clase said. ■
John Schieszer is a freelance medical journalist based in Seattle, Washington.
© BRENNA MACKAY, CARLETON UNIVERSITY
16 Renal & Urology News SUMMER 2023 www.renalandurologynews.com
A large interactive multi-touch display being developed by Canadian researchers.
“We expect our interactive large tabletop and interactive health data visualization technologies will support patients in clinical decision-making.”
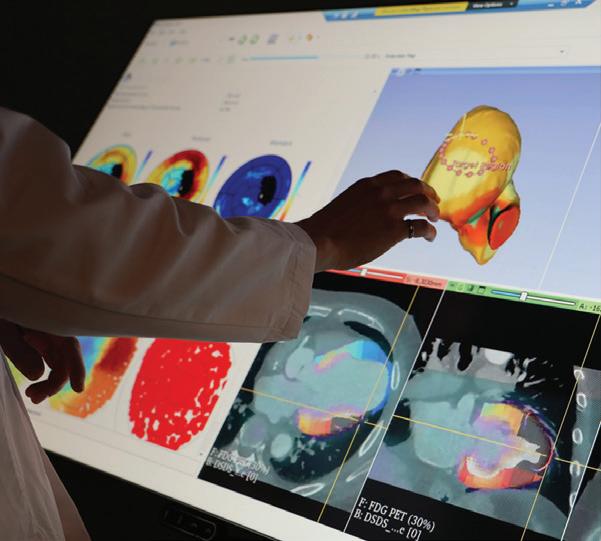




 BY JOHN SCHIESZER
BY JOHN SCHIESZER



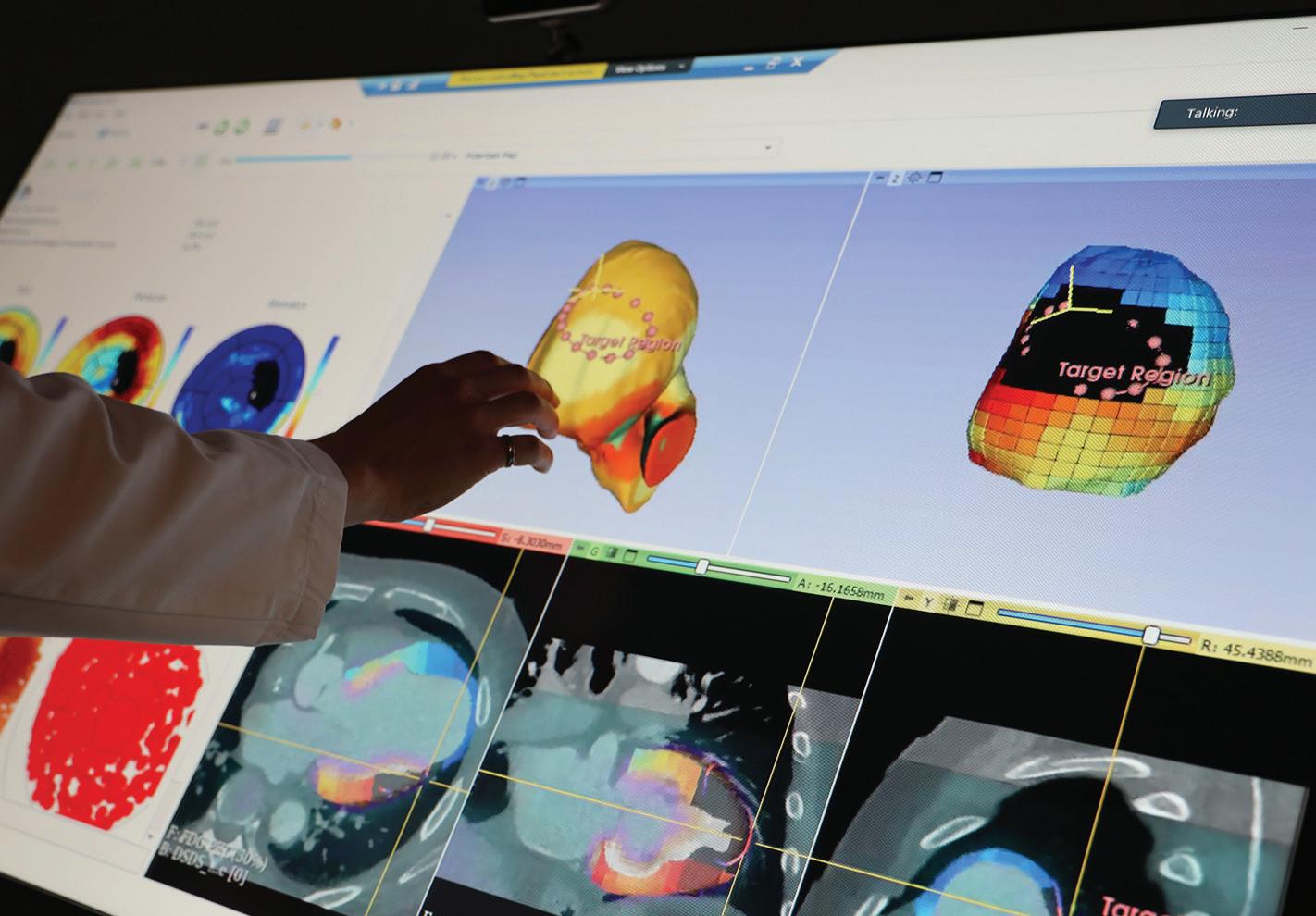 BY JOHN SCHIESZER
BY JOHN SCHIESZER
