ULTRASOUND ZOOM
A New Mode to Diagnose Pneumo(Peritoneum): Using POCUS to Identify Intra-abdominal Free Air By Brittney Giuffre, MD, PGY-2 Jackson Memorial Hospital
For me, training in a busy public hospital has not only been an incredible opportunity to see a broad range of pathology, but also to experience many of the challenges faced by busy emergency departments. One of our biggest challenges at Jackson Memorial Hospital is the high volume of critically-ill patients, which may result in them waiting several hours for evaluation and imaging. Almost reflexively, after determining a patient is “sick,” I find myself running to grab our ultrasound machine. The ability to get quick answers, with the bonus of low cost and no radiation risk to the patient, has spiked my interest to learn and use point-of-care ultrasound (POCUS), especially on our sickest patients with life-threatening diagnoses. For example, even before the portable x-ray machine rolls into the patient’s room, I can confidently determine whether a patient with shortness of breath has acute decompensated heart failure or a COPD exacerbation. However, I first had to learn to identify B-lines. Recently, I came across an intriguing blog post in which POCUS was used to diagnose intra-abdominal free air (IFA). Now that I’ve learned the technique and signs, I am undoubtedly going to apply this to my next patient with acute abdominal pain, and hopefully, I will diagnose pneumoperitoneum.
PNEUMOPERITONEUM
Pneumoperitoneum is an all-encompassing term for IFA inside the peritoneal cavity but outside the bowel 40
Edited by Leila Posaw, MD, MPH
Emergency Ultrasound Director, Jackson Memorial
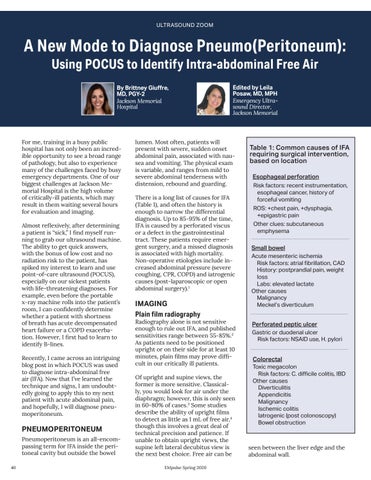
lumen. Most often, patients will present with severe, sudden onset abdominal pain, associated with nausea and vomiting. The physical exam is variable, and ranges from mild to severe abdominal tenderness with distension, rebound and guarding. There is a long list of causes for IFA (Table 1), and often the history is enough to narrow the differential diagnosis. Up to 85-95% of the time, IFA is caused by a perforated viscus or a defect in the gastrointestinal tract. These patients require emergent surgery, and a missed diagnosis is associated with high mortality. Non-operative etiologies include increased abdominal pressure (severe coughing, CPR, COPD) and iatrogenic causes (post-laparoscopic or open abdominal surgery).1
IMAGING Plain film radiography
Radiography alone is not sensitive enough to rule out IFA, and published sensitivities range between 55-85%.2 As patients need to be positioned upright or on their side for at least 10 minutes, plain films may prove difficult in our critically ill patients. Of upright and supine views, the former is more sensitive. Classically, you would look for air under the diaphragm; however, this is only seen in 60-80% of cases.3 Some studies describe the ability of upright films to detect as little as 1 mL of free air,4 though this involves a great deal of technical precision and patience. If unable to obtain upright views, the supine left lateral decubitus view is the next best choice. Free air can be EMpulse Spring 2020
Table 1: Common causes of IFA requiring surgical intervention, based on location Esophageal perforation
Risk factors: recent instrumentation, esophageal cancer, history of forceful vomiting ROS: +chest pain, +dysphagia, +epigastric pain Other clues: subcutaneous emphysema
Small bowel
Acute mesenteric ischemia Risk factors: atrial fibrillation, CAD History: postprandial pain, weight loss Labs: elevated lactate Other causes Malignancy Meckel’s diverticulum
Perforated peptic ulcer
Gastric or duodenal ulcer Risk factors: NSAID use, H. pylori
Colorectal
Toxic megacolon Risk factors: C. difficile colitis, IBD Other causes Diverticulitis Appendicitis Malignancy Ischemic colitis Iatrogenic (post colonoscopy) Bowel obstruction seen between the liver edge and the abdominal wall.