CASE REPORT
A DISAPPEARING ACT:
The curious case of Lemierre’s Syndrome By Amar Mittapalli, MD
UM Miller School of Medicine
Background The textbook definition of Lemierre’s syndrome is thrombophlebitis of the internal jugular vein. This serious condition usually follows an oropharyngeal infection with ensuing septic emboli. The syndrome usually manifests with Fusobacterium necrophorum as the causative organism. Diagnosis of this rare condition can be made by confirmation of thrombophlebitis of the internal jugular vein via imaging, positive culture of F. necrophorum, or demonstration of septic embolization secondary to thrombophlebitis.1
Case Presentation A 63-year-old-male with questionable retropharyngeal abscess, which extended into the mediastinum, had concerning features for Lemierre’s syndrome. Diagnosis of Lemierre’s syndrome was confirmed by duplex ultrasound of the neck. The condition was managed with prolonged usage of intravenous antibiotics.
Conclusion Having suspicion for Lemierre’s syndrome in any patient who presents with probable retropharyngeal abscess is important as early diagnosis and treatment can lead to a complete recovery of this rare condition.
By Andrew Napier, MD
UM Miller School of Medicine
ments. Due to the patient having a very muffled voice, and the need to secure his airway quickly, gathering a history from the patient was difficult. Much of the history was obtained from the patient’s family. As preparations were made in the Emergency Department for a difficult airway, his O2 saturation began to decline while on room air. He began to complain of inability to swallow secretions, as well as inability to breathe while laying flat. The patient was intubated in the ED for airway protection, using awake intubation with ketamine in a seated position with a GlideScope Video Laryngoscopy device. Intubation was complicated by trismus, edematous vocal cords with a narrowed glottic opening, and pus in the airway; however, it was performed successfully in a single attempt. Prior to arrival from the outside facility, the patient had been given Vancomycin, Zosyn, and Decadron. On physical examination, the patient was intubated and sedated.
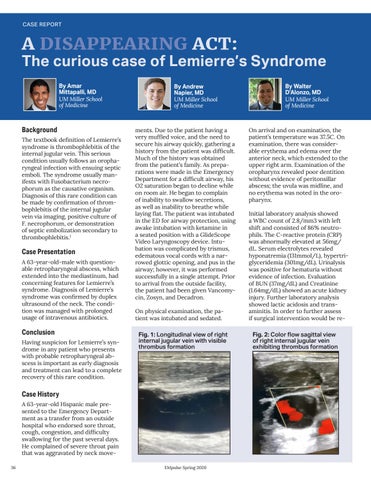
Fig. 1: Longitudinal view of right internal jugular vein with visible thrombus formation
Case History A 63-year-old Hispanic male presented to the Emergency Department as a transfer from an outside hospital who endorsed sore throat, cough, congestion, and difficulty swallowing for the past several days. He complained of severe throat pain that was aggravated by neck move36
EMpulse Spring 2020
By Walter D’Alonzo, MD
UM Miller School of Medicine
On arrival and on examination, the patient’s temperature was 37.5C. On examination, there was considerable erythema and edema over the anterior neck, which extended to the upper right arm. Examination of the oropharynx revealed poor dentition without evidence of peritonsillar abscess; the uvula was midline, and no erythema was noted in the oropharynx. Initial laboratory analysis showed a WBC count of 2.8/mm3 with left shift and consisted of 86% neutrophils. The C-reactive protein (CRP) was abnormally elevated at 56mg/ dL. Serum electrolytes revealed hyponatremia (131mmol/L), hypertriglyceridemia (301mg/dL). Urinalysis was positive for hematuria without evidence of infection. Evaluation of BUN (37mg/dL) and Creatinine (1.64mg/dL) showed an acute kidney injury. Further laboratory analysis showed lactic acidosis and transaminitis. In order to further assess if surgical intervention would be re-
Fig. 2: Color flow sagittal view of right internal jugular vein exhibiting thrombus formation