6 minute read
Nail fold changes as a marker for psoriatic arthritis in psoriasis of the skin / Jørgen
Nail fold changes as a marker for psoriatic arthritis in psoriasis of the skin
Patients with psoriatic arthritis may have decreased capillary density and blood flow as well as microbleeds in the nail fold. However, no single diagnostic capillary pattern could identify psoriatic arthritis.
JØRGEN GULDBERG-MØLLER is a trained physiotherapist, doctor and PhD. He is employed as a ward doctor at Sjællands Universitetshospital in Køge as an ultrasound manager. He specializes in musculoskeletal diagnostic imaging and has a special interest in ultrasound. METTE MOGENSEN is a dermatologist. For more than 15 years, she has been working with the development of new advanced imaging diagnostics to detect skin diseases faster, easier, and more accurately by scanning the skin – in close collaboration with the Technical University of Denmark and leading international research groups. She has a special focus on rapid diagnosis of breast cancer, but also imaging of autoimmune skin diseases and detection of vascular changes in the skin in patients with psoriasis and psoriatic arthritis, so-called nail fold capillaroscopy.
Up to 30% of patients with skin psoriasis (PsO) later develop symptoms compatible with psoriatic arthritis (PsA)1 with a time-lag of approximately seven years.2 This delay provides a unique opportunity for early detection in this disease group already associated with highly specialized treatment for their skin disease by a dermatologist.
Alertness for early manifestations of psoriatic arthritis is of utmost importance, as a delay in diagnosis of as little as six months may be associated with a lower treatment response.3 An early intervention with anti-inflammatory drugs can significantly improve the clinical and radiographic results. Dermatologists and general practitioners treating patients with skin psoriasis are primarily responsible for assessing factors that could signal a transition from primary skin disease to also include joint and tendon attachments.
Prognostic factors for disease development
The onset symptom of PsA is rarely a swollen joint or a sausage finger. Therefore, it is important to be aware of other factors that may help identify at-risk patients. Psoriatic nail changes, especially the occurrence of onycholysis (nail plate solution) and nail pitting (thimble dots), are important prognostic markers for the development of arthritis in the outer joints.4
Against this background, nail fold capillaroscopy (NVK) by plain dermoscopy and optical coherence tomography (OCT) has the potential to diagnose PsA, and to differentiate the disease from PsO and even from osteoarthritis of the outer joints (OA), where differential diagnostic plays a role.
We aimed to assess the diagnostic properties of NVK and OCT in patients with PsA compared to patients with PsO and OA based on capillary patterns at the nail bed.
We included 50 patients with PsA, 12 with PsO, and 13 with OA from rheumatology and dermatological outpatient clinics in Zealand, a total of five centers.
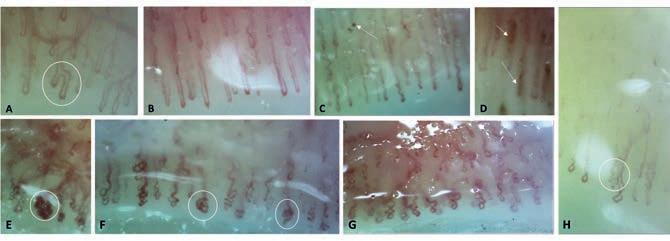
A: branched capillary arm in PsA. B: Extended capillaries in PsA. C: Implementing capillaries with microbleeds in PsA. D: Microbleeds in PsA E: Glomerular and dilated capillaries in OA. F: Glomerular and dilated capillaries in PSO. A: branched capillary arm in PsA. B: Extended capillaries in PsA. C: Implementing capillaries with microbleeds in PsA. D: G: Crossed / meandering capillaries in PsA. H: Capillary branches in OA. Microbleeds in PsA E: Glomerular and dilated capillaries in OA. F: Glomerular and dilated capillaries in PSO. G: Crossed / Definition: Extended capillaries have diameters of 20-50 mm meandering capillaries in PsA. H: Capillary branches in OA. Definition: Extended capillaries have diameters of 20-50 mm.
Table 1: Distribution of NVK and OCTA capillary morphology by PsA, PsO and OA Table 1 – Distribution of NVK and OCTA capillary morphology by PsA, PsO and OA
NVK – rating PsA (n=188) PsO (n=42) OA (n=48) PsAvs PsO PsAvs OA
Belowmeancapillary density,n(%) Irregularlyenlarged capillaries,n(%) Giantcapillary,n(%) 95(51%) 14(31 %) 24(51 %) P=0.019 P=1.000
42(22%) 14(33%) 12(25 %) P=0.163 P=0.703
3(2%) 0 0
P=0.631 P=0.610 Microhaemorrhages,n(%) 24(13%) 3(7%) 1(2%) P=0.429 P=0.034 Capillaryramifications,n(%) 27(14%) 10 (24 %) 14(29 %) P=0.162 P=0.020 Capillarydisorganization,n (%) 84(45%) 24(57 %) 23(48 %) P=0.172 P=0.746
o l C u t o u m d m o d a C T A O OCTA – rating PsA n=193 PsO n=48 OA n=52 PsAvs PsO PsAvs OA
Belowmean capillary density,n(%) Irregularlyenlarged capillaries,n(%) 103(53 %) 10(21 %) 17(33 %) P<0.001 P=0.012
66(34%) 27(56 %) 10(19 %) p=0.005 P=0.062
Giantcapillary,n(%) 0 0 0 - -
Microhaemorrhages,n(%) 0 0 0 - -
Capillary ramifications,n(%) 0 0 0 -
Capillarydisorganization,n (%) 108(55 %) 22(46 %) 25(49 %) P=0.263 P=0.529
A R U L E u m d m o d a K N V Nailthickness* ,mm.,mean (SD) OCTAbloodflow percentage,mean(SD) 0.62 (0.13) 0.73 (0.39) 0.59 (0.08) p=0.876 P=0.020
6.00 6.94 7.88 P=0.052 P<0.001 (2.94) (3.08) (3.30)
Capillarymorphology PsA n=192 PsO n=48 OA n=52 PsAvs PsO PsAvs OA
Tortuous/Crossedcapillaries, n(%) 105(55 %) 34(71 %) 29(56 %) P=0.050 P=1.000 Enlargedcapillarydiameter, n (%) 33(17%) 10(21 %) 9(17 %) P=0.674 P=1.000 Ramifiedcapillaries,n(%) 24(13%) 7(15%) 10(19 %) P=0.810 P=0.258 Microhaemorrhages,n(%) 32(17%) 3(6%) 4(8%) P=0.106 P=0.125 Elongatedcapillaries,n(%) 11(6%) 2(4%) 2 (4%) P=0.747 P=0.741 Differentcapillaryshapes, glomerular,n (%) 5(3 %) 6(13 %) 1(2 %) P=0.010 P=1.000
Data presented as a percentage of the capillary findings within the group, unless otherwise indicated. Differences between PsA and the other groups are presented as a two-sided p-value p <0.05 is considered significant.
CONCLUSION: Even though we identified several characteristic capillary features by NVK and OCT examination in the three patient groups, no single capillary pattern was associated with either increased or decreased likelihood of being diagnosed with PsA.
Although patients with PsO showed the most nail changes on clinical examination, patients with PsA could be differentiated from patients with PsO and OA by significantly lower capillary density and blood flow assessed on OCT and by the presence of microbleeds in the nail fold at NVK.
Patients with PsO could be characterized by a high incidence of crossed and glomerular capillaries assessed on NVK and irregularly enlarged capillaries on OCT.
The OA group showed a significantly higher incidence of capillary branches on NVK, which could perhaps be attributed to a higher age in this group and is also seen in 47% of healthy individuals.5
Despite these differences in capillary morphology between the three patient groups, we could not identify a specific capillary pattern or a particular degree of blood flow that was significantly associated with an increased or decreased likelihood of being diagnosed with PsA.
From a clinical perspective, the results may require greater collaboration between dermatologists and rheumatologists to benefit the patient. With knowledge of common examination tools and a common understanding of the significance of nail changes and arthritis in the outer joints in PsA, patients at risk can hopefully be identified earlier and avoid permanent joint damage with early treatment.
A lower capillary density and low blood flow by OCT examination and the presence of microbleeds in patients with PsA raise exciting questions for further research. Is there an expression of a higher inflammatory burden in PsA compared to PsO and OA?
ORIGINAL PUBLICATION: Guldberg-Møller J, Henriksen M, Ellegaard K et. al. Novel application of optical coherence tomography and capillaroscopy in psoriatic arthritis concerning psoriasis and hand osteoarthritis. Rheumatol Adv Pract. 2021;5(3). DOI: 10.1093 / rap / rkab065.
References:
1. Ritchlin CT, Colbert RA, Gladman DD. Psoriatic arthritis. N Engl J Med. 2017;376(10): 957-970. 2. Tillett W, Charlton R, Nightingale A, et al. interval between the onset of psoriasis and psoriatic arthritis comparing the UK Clinical Practice Research Datalink with a hospital-based cohort. Rheumatol (Oxford). 2017;56(12): 2109-2113. 3. Haroon M, Gallagher P, FitzGerald O. Diagnostic delay of more than 6 months contributes to poor radiographic and functional outcome in psoriatic arthritis. Ann Rheum Dis. 2015;74(6): 1045-1050. 4. Love TJ, Gudjonsson JE, Valdimarsson H, Gudbjornsson B. Small joint involvement in psoriatic arthritis is associated with onycholysis: The Reykjavik psoriatic arthritis study. Scand J Rheumatol. 2010;39(4): 299-302. 5. Hoerth, Kundi, Katzenschlager, Hirschl. Qualitative and quantitative assessment of nailfold capillaries by capillaroscopy in healthy volunteers. Vasa. 2012;41(1): 19-26.
Psoriasis
TreatmentTrajectory










