5 minute read
The role of patients in the development of Nordic dermatology / Lars F. Werner
How can we include the patient’s perspective in future dermatological treatment? Here is an update on hot topics in patient-centered treatment from the 35th NCDV Congress 2022 as seen from the patient’s perspective.
LARS WERNER is Managing Director at the Danish Psoriasis Association and a long-term patient research partner and advisory board member in the field of psoriasis.
At the recent Nordic Congress of Dermatology and Venereology held in Copenhagen, Denmark April 19-22, I was invited to give a small oral presentation on the subject of “The role of patients in the development of Nordic dermatology”.
I chose to focus on the recent development in treatment options, the life quality aspect, and patient empowerment.
Concordance as guidance in treatment
Certainly, within the area of psoriasis, the number of new treatments has increased significantly over the past 20 years. The biological treatments have given hope to many patients. When it comes to communication between health care providers and patients, we have come a long way in achieving a mutually respectful dialogue. The number of patients in the dermatological field seems to be endless, and it seems that it can be tempting sometimes to make consultations swift. However, we do see that the overall treatment result improves by implementing the practice (or philosophy, if you like) of concordance.
Both “compliance” and “adherence” focus more on patient behavior regarding medication-taking. In contrast, “concordance” highlights the processes that underlie medication-taking, such as an equal and effective therapeutic relationship that supports the patient during the entire course of long-term treatment.
From a patient perspective, concordance should be a standard operating procedure (SOP) in all corners of the health care system.
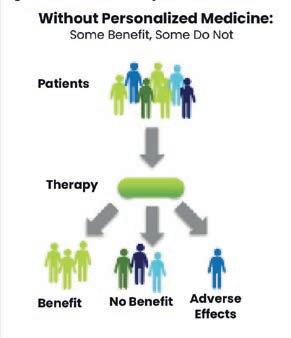
Biomarker diagnostics personalizes treatment
In years to come, patients may look forward to a more personalized treatment/medication that is driven by the implementation of biomarker diagnostics on a much larger scale than is the case today (figure 1).
Figure 1 – Benefits of personalized medicine
Adapted from Bayer Healthcare, “Personalized Medicine”.
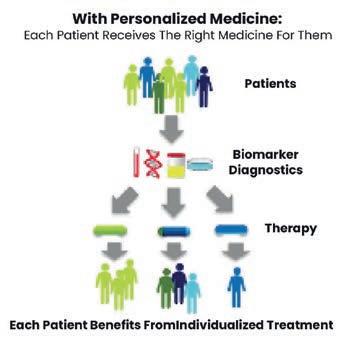
Table 1 – Depression in patients with common skin diseases and controls Table 1. Depression in patients with common skin diseases and controls in percentages and ORs in percentages and ORs (95% confidence interval) N = 4,994 (95% confidence interval) N = 4,994
Diagnosis
Psoriasis Non-melanoma skin cancer Infections skin Eczema Acne Nevi Atopic eczema Benign skin tumors Hand eczema Leg ulcers Dermatological out-patients overall Controls Depression clinical case HADS ≥ 11% (n) 13.8 (84) 4.8 (18) 8.9 (21) 8.0 (18) 5.7. (12) 6.0 (11) 10.1 (16) 4.8 (7) 15.1 (21) 24.3 (28) 10.1 (357) 4.3 (58) P-value
<0.001 0.729 0.001 0.007 0.311 0.215 <0.001 0.587 <0.001 <0.001 <0.001 — Crude OR1 depression clinical case HADS > 11 3.23 (2.06-5.05) 1.21 (0.62-2.36) 2.59 (1.40-4.76) 1.79 (0.89-3.59) 1.53 (0.74-3.13) 2.05 (0.99-4.22) 3.55 (1.28-6.92) 1.50 (0.69-3.65) 4.85 (2.59-9.10) 11.23 (5.71-22.09) 2.69 (1.88-3.84) 1 Adjusted OR2 depression clinical case HADS > 11 3.02 (1.86-4.90) 0.97 (0.41-2.32) 2.65 (1.39-5.06) 1.68 (0.80-3.53) 1.74 (0.73-4.17) 2.14 (1.01-4.53) 3.27 (1.61-6.62) 1.43 (0.55-3.74) 4.00 (2.01-7.97) 10.217 (4.07-25.41) 2.40 (1.67-3.47) 1
Abbreviations: HADS, hospital anxiety and depression scale; MD, missing data; OR, odds ratio. Missing data hospital anxiety depression scale-depression = 109 (patients = 102; controls = 71). Without participants with missing data for one or more of the predictors. 1 Regression model for each disease separately, adjusting for gender, age, socio-economic status, stress, and co-morbidity. 2 Adapted from: Dalgard FJ, Gieler U, Tomas-Aragones L, et al. The Psychological Burden of Skin Diseases: A Cross-Sectional Multicenter Study among Dermatological Out-Patients in 13 European Countries. Journal Invest Dermatol. 2015;135(4): 984–991. Table 3.
Abbreviations: HADS, hospital anxiety and depression scale; MD, missing data; OR, odds ratio. Missing data hospital anxiety depression scale-depression = 109 (patients = 102; controls = 71). 1Without participants with missing data for one or more of the predictors. 2Regression model for each disease separately, adjusting for gender, age, socio-economic status, stress, and co-morbidity. Adapted from: Dalgard FJ, Gieler U, Tomas-Aragones L, et al. The Psychological Burden of Skin Diseases: A Cross-Sectional Multicenter Study among Dermatological Out-Patients in 13 European Countries. Journal Invest Dermatol. 2015;135(4): 984–991. Table 3.
Life Quality – Patient-reported outcome measures
The psychological burden of skin diseases is well known. Here is the result of a 2015 study with the esteemed professor Jemec as one of the co-authors:
Overall, 10.1% of dermatological patients were clinically depressed compared with 4.3% of controls. And the numbers of depressed patients were higher for those with leg ulcers, hand eczema, and psoriasis, as measured on the HADS score (Hospital Anxiety and Depression Scale).
One tool that is very useful to capture all aspects of skin diseases is Patient-Reported Outcome Measures (PROM), which is a questionnaire capturing relevant issues for both health care providers and patients. In 2022, we are implementing this tool for psoriasis in Denmark. This means that at least once a year, a psoriasis patient will also be asked questions related to how the skin disease affects the person’s daily life – his or her life quality.
Patient Empowerment
I would also like to briefly touch upon the area of patient empowerment. WHO’s definition of patient empowerment is “A process through which people gain greater control over decisions and actions affecting their health.”
As a patient organization, we know that many patients want to learn more about their skin disease, particularly how to control symptoms. Patient organizations in all the Nordic countries put a lot of resources to support this by developing: • Patient education – in print • Patient education – face-to-face (e.g. patient schools) • Patient education – virtual.
CONCLUSION: The next step toward more patient-centered treatments includes: A movement away from a narrow focus on compliance, and towards more concordance-based interaction. We also need development and implementation of biomarker diagnostics to supply precision medicine-based treatments , and utilization of PROM to support patient empowerment.









